Geriatric Case Study
advertisement
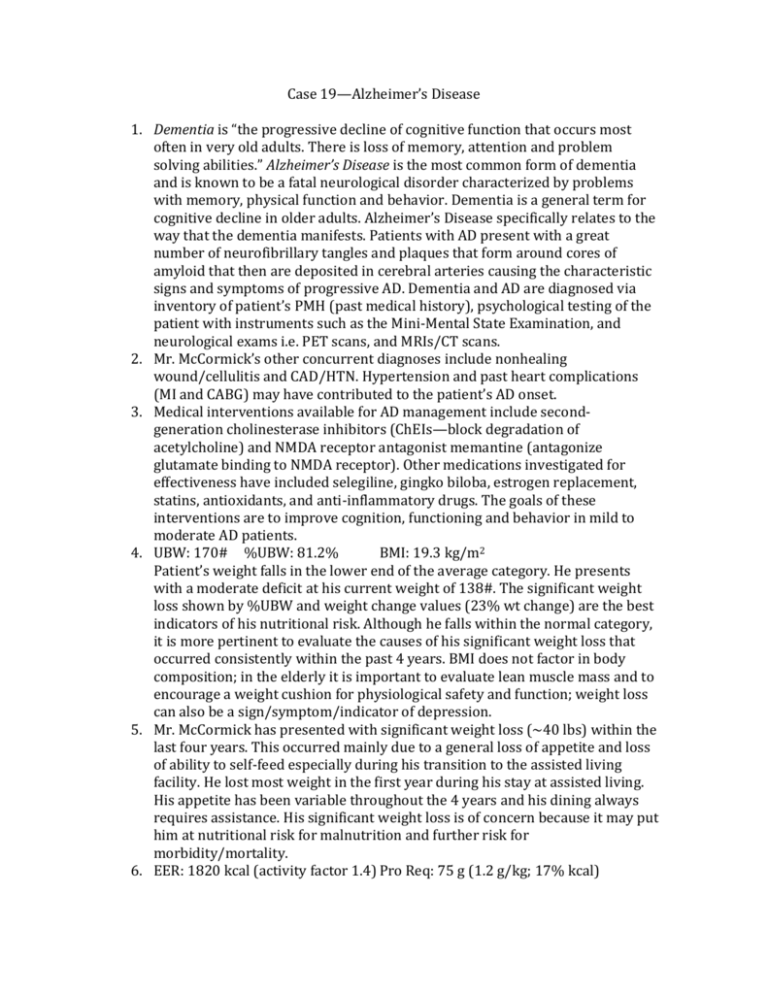
Case 19—Alzheimer’s Disease 1. Dementia is “the progressive decline of cognitive function that occurs most often in very old adults. There is loss of memory, attention and problem solving abilities.” Alzheimer’s Disease is the most common form of dementia and is known to be a fatal neurological disorder characterized by problems with memory, physical function and behavior. Dementia is a general term for cognitive decline in older adults. Alzheimer’s Disease specifically relates to the way that the dementia manifests. Patients with AD present with a great number of neurofibrillary tangles and plaques that form around cores of amyloid that then are deposited in cerebral arteries causing the characteristic signs and symptoms of progressive AD. Dementia and AD are diagnosed via inventory of patient’s PMH (past medical history), psychological testing of the patient with instruments such as the Mini-Mental State Examination, and neurological exams i.e. PET scans, and MRIs/CT scans. 2. Mr. McCormick’s other concurrent diagnoses include nonhealing wound/cellulitis and CAD/HTN. Hypertension and past heart complications (MI and CABG) may have contributed to the patient’s AD onset. 3. Medical interventions available for AD management include secondgeneration cholinesterase inhibitors (ChEIs—block degradation of acetylcholine) and NMDA receptor antagonist memantine (antagonize glutamate binding to NMDA receptor). Other medications investigated for effectiveness have included selegiline, gingko biloba, estrogen replacement, statins, antioxidants, and anti-inflammatory drugs. The goals of these interventions are to improve cognition, functioning and behavior in mild to moderate AD patients. 4. UBW: 170# %UBW: 81.2% BMI: 19.3 kg/m2 Patient’s weight falls in the lower end of the average category. He presents with a moderate deficit at his current weight of 138#. The significant weight loss shown by %UBW and weight change values (23% wt change) are the best indicators of his nutritional risk. Although he falls within the normal category, it is more pertinent to evaluate the causes of his significant weight loss that occurred consistently within the past 4 years. BMI does not factor in body composition; in the elderly it is important to evaluate lean muscle mass and to encourage a weight cushion for physiological safety and function; weight loss can also be a sign/symptom/indicator of depression. 5. Mr. McCormick has presented with significant weight loss (~40 lbs) within the last four years. This occurred mainly due to a general loss of appetite and loss of ability to self-feed especially during his transition to the assisted living facility. He lost most weight in the first year during his stay at assisted living. His appetite has been variable throughout the 4 years and his dining always requires assistance. His significant weight loss is of concern because it may put him at nutritional risk for malnutrition and further risk for morbidity/mortality. 6. EER: 1820 kcal (activity factor 1.4) Pro Req: 75 g (1.2 g/kg; 17% kcal) I used the Mifflin-St. Jeor Equation because it has been tested to give the most reliable and accurate estimations of energy needs. I used an activity factor of 1.4 to take into consideration the pt’s current injury and infection status as well as boost his calories to prevent malnutrition. I decided on 1.2 g/kg of protein to ensure that the pt has enough protein to maintain and support lean muscle mass stores. 7. Intake Domain Dx: inadequate energy intake, inadequate oral/food intake, inadequate fluid intake, evident protein-energy malnutrition, inadequate protein-energy intake, inadequate intakes of multiple nutrients (specified). 8. Medications & Function: Furosemide Diuretic used to treat hypertension Atenolol Beta-blocker used to treat hypertension Lisinopril ACE inhibitor used to treat hypertension Zocor HMG CoA reductase/statins used for reducing “bad” cholesterol levels Haloperidol Antipsychotic med used to manage dementia Warfarin Anticoagulant (blood thinner) Donepezil Prevents breakdown of acetylcholine/improves function of nerve cells 9. Abnormal Biochemical Measures: Albumin (2.9 low), total protein (5.5 low), prealbumin (14 low), transferrin (165 low), BUN (22 high), creatinine (1.3 high), WBC (16.0 high), Hgb (13.5 low), MCV (77 low), MCH (24 low), MCHC (30 low), RDW (17.8 high), % LYM (10 low), LYMPHS (10 low), ferritin (18 low) 10. Clinical Domain Dx: underweight, involuntary weight loss, swallowing difficulty, impaired ability to prepare foods/meals, self-feeding difficulty. 11. Issues associated with Mr. McCormick’s primary diagnosis of Alzheimer’s disease that could potentially interfere with his ability to consume an adequate diet include loss of appetite, inability to self-feed and prepare meals, signs of depression, decline of focus and physical capacity to perform basic functions and carry out basic behaviors i.e. meal preparation and feeding. 12. PES #1: Inadequate energy intake related to Alzheimer’s Disease and associated symptoms such as loss of appetite and inability to self-feed as evidenced by significant weight loss (23% weight change) within the past four years and lab results indicative of malnutrition. PES #2: Self-feeding difficulty related to inability to prepare meals and required assistance at meals as evidenced by Alzheimer’s Disease diagnosis and associated symptoms such as decline in ability to focus and perform basic functions and behaviors and reported inadequate energy intake. 13. Goal #1: Increase energy intake to ~1800 kcal Intervention #1: provide high-energy and high-protein supplements (i.e. shakes, ensure) with and between meals, to be provided with assistance. Emphasize energy dense foods at breakfast when appetite is greatest. Goal #2: Provide food utensils and proper assistance to patient for meal times; allow patient to do what he is able to do independently Intervention #2: Prepare foods that are easy to administer and attractive to patient i.e. finger foods, soft/mechanically processed foods 14. To improve oral intake during an AD patient’s hospitalization, attend to food preferences/likes, prepare foods to be soft/easy to swallow/mechanically processed, and provide utensils that assist patient with self-feeding. 15. Oral intake would be appropriately measured through plate waste records, monitoring weight, checking I&O’s and tolerance to diet, evaluation/assessment of chemistry panel (look for changes in albumin, prealbumin, BUN, creatinine) and observing an overall improvement in immunity status.