File
advertisement
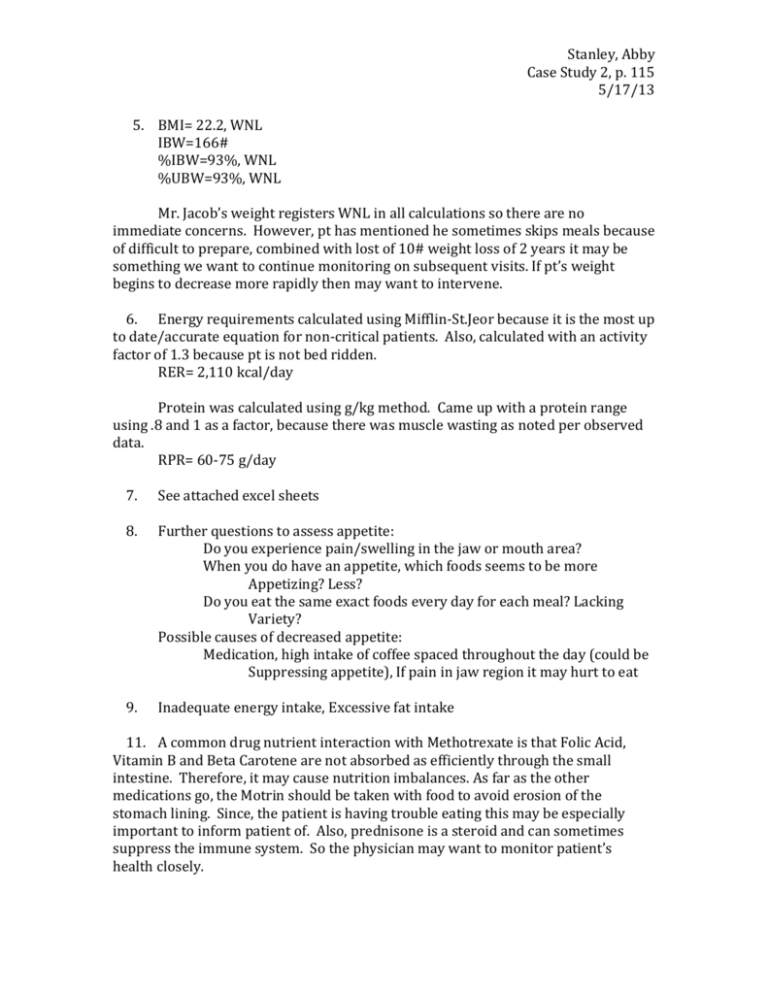
Stanley, Abby Case Study 2, p. 115 5/17/13 5. BMI= 22.2, WNL IBW=166# %IBW=93%, WNL %UBW=93%, WNL Mr. Jacob’s weight registers WNL in all calculations so there are no immediate concerns. However, pt has mentioned he sometimes skips meals because of difficult to prepare, combined with lost of 10# weight loss of 2 years it may be something we want to continue monitoring on subsequent visits. If pt’s weight begins to decrease more rapidly then may want to intervene. 6. Energy requirements calculated using Mifflin-St.Jeor because it is the most up to date/accurate equation for non-critical patients. Also, calculated with an activity factor of 1.3 because pt is not bed ridden. RER= 2,110 kcal/day Protein was calculated using g/kg method. Came up with a protein range using .8 and 1 as a factor, because there was muscle wasting as noted per observed data. RPR= 60-75 g/day 7. See attached excel sheets 8. Further questions to assess appetite: Do you experience pain/swelling in the jaw or mouth area? When you do have an appetite, which foods seems to be more Appetizing? Less? Do you eat the same exact foods every day for each meal? Lacking Variety? Possible causes of decreased appetite: Medication, high intake of coffee spaced throughout the day (could be Suppressing appetite), If pain in jaw region it may hurt to eat 9. Inadequate energy intake, Excessive fat intake 11. A common drug nutrient interaction with Methotrexate is that Folic Acid, Vitamin B and Beta Carotene are not absorbed as efficiently through the small intestine. Therefore, it may cause nutrition imbalances. As far as the other medications go, the Motrin should be taken with food to avoid erosion of the stomach lining. Since, the patient is having trouble eating this may be especially important to inform patient of. Also, prednisone is a steroid and can sometimes suppress the immune system. So the physician may want to monitor patient’s health closely. Stanley, Abby Case Study 2, p. 115 5/17/13 12. In the physician’s assessment he noted slight temporal wasting as well at slight muscle wasting in the extremities. However, the pt BUN, Creatinine and prealbumin all came back WNL. It might be important to use skin fold measurement to determine body fat percentage, and thus a lean muscle mass percentage. 13. If the pt is not taking enough calories throughout the day, due to loss of appetite, his body may be breaking down his protein stores in order to provide energy to the brain/body. This would result in a loss of lean muscle mass, which may be visible through muscle wasting. 14. BUN, Albumin, Prealbumin, 15. Creatinine, ESR, anti-CCP, and CRP 16. Involuntary weight loss, Undesirable food choices 17. A) Inadequate energy intake related to loss of appetite as report by pt as evidences by appearance of slight muscle wasting per Doctor’s report B) Excessive fat intake related to high kcal, high fat meals as evidences by pt reported usual dietary intake C) Involuntary weight loss related to loss of appetite as evidenced by 10# weight loss of 2 years D) Undesirable food choices related to food preparation as evidenced by high amount of meals eaten “out” at restaurants/fast food, 2-3 x per week 18. A, C, B, D 19. A) Increase pt’s intake of nutrient dense foods to prevent protein conversion to energy. Educate pt on nutrient dense foods, so that when he does feel like eating he is getting proper nutrition B) Reduce amounts of high kcal, high fat meals pt is consuming. Educate pt on why fats are not healthy for him, and encourage the intake of unsaturated fats. C) Increase pt appetite for food. Encourage pt to add more variety in meal plan by cooking more meals at home and introduce pt to new, healthy ingredients that will allow this. D) Have patient condense eating out to once a week. Educate pt on easy, healthy, flavorful meals that can be prepped ahead of time to prevent going to fast food establishments or restaurants. Stanley, Abby Case Study 2, p. 115 5/17/13