NCP PES Samples
advertisement
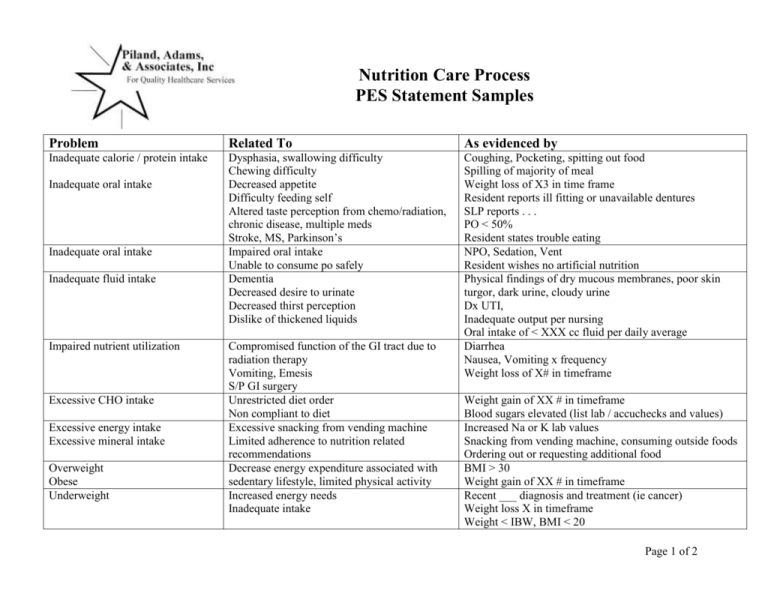
Nutrition Care Process PES Statement Samples Problem Related To As evidenced by Inadequate calorie / protein intake Dysphasia, swallowing difficulty Chewing difficulty Decreased appetite Difficulty feeding self Altered taste perception from chemo/radiation, chronic disease, multiple meds Stroke, MS, Parkinson’s Impaired oral intake Unable to consume po safely Dementia Decreased desire to urinate Decreased thirst perception Dislike of thickened liquids Coughing, Pocketing, spitting out food Spilling of majority of meal Weight loss of X3 in time frame Resident reports ill fitting or unavailable dentures SLP reports . . . PO < 50% Resident states trouble eating NPO, Sedation, Vent Resident wishes no artificial nutrition Physical findings of dry mucous membranes, poor skin turgor, dark urine, cloudy urine Dx UTI, Inadequate output per nursing Oral intake of < XXX cc fluid per daily average Diarrhea Nausea, Vomiting x frequency Weight loss of X# in timeframe Inadequate oral intake Inadequate oral intake Inadequate fluid intake Impaired nutrient utilization Excessive CHO intake Excessive energy intake Excessive mineral intake Overweight Obese Underweight Compromised function of the GI tract due to radiation therapy Vomiting, Emesis S/P GI surgery Unrestricted diet order Non compliant to diet Excessive snacking from vending machine Limited adherence to nutrition related recommendations Decrease energy expenditure associated with sedentary lifestyle, limited physical activity Increased energy needs Inadequate intake Weight gain of XX # in timeframe Blood sugars elevated (list lab / accuchecks and values) Increased Na or K lab values Snacking from vending machine, consuming outside foods Ordering out or requesting additional food BMI > 30 Weight gain of XX # in timeframe Recent ___ diagnosis and treatment (ie cancer) Weight loss X in timeframe Weight < IBW, BMI < 20 Page 1 of 2 Problem Related To As evidenced by Increased calorie / protein needs Increased involuntary physical activity (Parkinson’s disease) Wound, Surgery, Infection, Septic Cancer, MS Non compliance with gluten free diet Excessive consumption of sugar free candy Non compliance with GERD prevention advice Impaction, Illeus No bowel sounds Impaired utilization from renal disease Excessive CHO intake Excessive fat intake Inadequate fluid intake Dietary management of (name specific disease process ie DM, CHF, Renal, Diverticular, HTN, edema, constipation) Low rate of infusion Resident pulled out tube TF not at goal Diet order as written does not meet needs or goal TF or TPN order > or < estimated needs Recent weight loss of x# in timeframe Inadequate protein stores (list alb or prealb value) Wound (stage and location) Altered GI function Altered nutrient related lab value Nutrition related knowledge deficit Inadequate intake from Tube feeding, enteral formula Excessive Intake from TF or TPN Inadequate Intake from TF or TPN Inability or lack of desire to manage self care Impaired ability to prepare foods / meals Physical inactivity Diagnosis (stroke, wound, dementia, etc) Limited mobility Limited knowledge Diarrhea Constipation GI complaints per resident NPO status Need for TPN for nutrition support State lab and value Resident reports lack of knowledge regarding (be specific) Current order less than goal rate of __ cc/hr TF meeting <100% needs Inappropriate lab value (list) Blood sugars elevated (list) Weight loss or gain of X# in timeframe Admission in LTC / rehab care. If no new problems exist, weight stable, all labs WNL, no new wounds, etc then state, “Nutrition interventions in place, no new nutrition problems, pes as above.” Page 2 of 2