CPP in TBI - Clinical Departments
advertisement
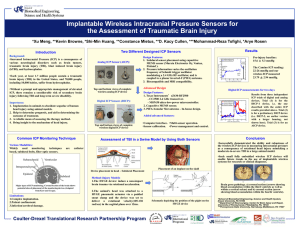
Ebony Hilton CPP in TBI: *Patients with severe TBI (GCS ≤8) &/or clinical symptoms suggesting possible impending herniation from elevated ICP (unilateral or bilaterally fixed and dilated pupil(s), decorticate or decerebrate posturing, bradycardia, hypertension, and/or respiratory depression) should be treated urgently, with head elevation, hyperventilation, and osmotic therapy (mannitol 1 g/kg iv) concurrently with neuroimaging and other assessments. *The principle focus of critical care management for severe TBI is to limit secondary brain injury. In general, treatment efforts are aimed at intracranial pressure management and maintenance of cerebral perfusion as well as optimizing oxygenation and blood pressure and managing temperature, glucose, seizures, and other potential secondary brain insults. *Intracranial pressure — Elevated intracranial pressure (ICP) is associated with increased mortality and worsened outcome -Simple techniques should be instituted as soon as possible: *Head of bed elevation to 30 degrees *Optimization of venous drainage: keeping the neck in neutral position, loosening neck braces if too tight *Monitoring central venous pressure and avoiding excessive hypervolemia -Indications for ICP monitoring in TBI *GCS score ≤8 *abnormal CT scan showing evidence of mass effect from lesions such as hematomas, contusions, or swelling -ICP monitoring in severe TBI patients with a normal CT scan may be indicated if two of the following features are present (age >40 years, motor posturing, SBP<90 mm Hg). -A ventricular catheter connected to a strain gauge transducer is the most accurate and cost-effective method of ICP monitoring and has the therapeutic advantage of allowing for CSF drainage to treat rises in ICP . -treatment for elevated ICP should be initiated when ICP rises above 20 mmHg *Ventricular drainage is generally attempted first. *CSF should be removed at a rate of approximately 1 to 2 mL/minute, for two to three minutes at a time, with intervals of two to three minutes in between -until a satisfactory ICP has been achieved (ICP <20 mmHg) or until CSF is no longer easily obtained. *Slow removal can also be accomplished by passive gravitational drainage through the ventriculostomy. *If ICP remains elevated, other interventions include osmotic therapy, hyperventilation, and sedation. -Osmotic therapy — The intravascular injection of hyperosmolar agents creates an osmolar gradient, drawing water across the blood-brain barrier. This leads to a decrease in interstitial volume and a decrease in ICP. *Mannitol is the agent used most consistently to achieve ICP control in various settings and it has also been shown to improve cerebral blood flow. Mannitol is administered in boluses of 0.25 to 1 g/kg every four to six hours as needed. Monitoring of serum osmolality (maintained <320 mMol/L), fluid balance, renal function, and electrolytes is required. *Hypertonic saline is being used increasingly in this setting, but with varying volumes and tonicity (3 to 23.4 percent) and either as a bolus or continuous infusion. -Hyperventilation — PaCO2 decreases thereby leading to cerebral vasoconstriction, which then results in decreased cerebral blood volume and ICP. *hyperventilation-induced vasoconstriction may also cause secondary ischemia and may thereby worsen outcomes. *Hyperventilation can also increase extracellular lactate and glutamate levels that may contribute to secondary brain injury *Mild to moderate hyperventilation can be considered at later stages, but PaCO2 of less than 30 mmHg should be avoided -Sedation — may lower ICP by reducing metabolic demand. *ameliorate ventilator asynchrony and blunt sympathetic responses of hypertension and tachycardia. *can cause hypotension and cerebral vasodilation that in turn may aggravate cerebral hypoperfusion and elevate ICP. *Barbiturate coma has been used traditionally in this setting. *In refractory cases, barbiturate coma, induced hypothermia, and decompressive craniectomy may be considered