Biochemistry Ch 38 707-721 [4-20
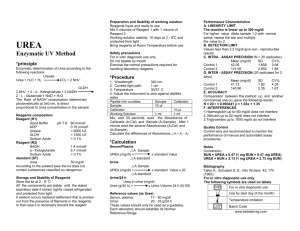
advertisement
Biochemistry Ch 38 707-721 The Urea Cycle Fate of Amino Acid Nitrogen 1. Transamination Reactions – removes nitrogen from amino acids, whereby the N is transferred as an amino group to an α-ketoglutarate to form glutamate -original amino acid converted to α-ketoacid -all AA EXCEPT lysing + arginine can undergo transaminations -done by transaminases -pyridoxal phosphate is REQUIRED COFACTOR, derived from vitamin B6, activation: -Pyridoxine (B6) Pyridoxaldehyde Pyridoxal Phosphate (PLP) -Vitamin B6 deficiency – dermatitis, microcytic, hypochromic anemia. Xanthurenic acid appears in urine because of inability to metabolize amino acids, decreased ability to synthesize heme from glycine causes hypochromic anemia 2. Removal of Amino Acid Nitrogen as Ammonia – cells release nitrogen from AA as ammonia or ammonium. Physiologic pH favors ammonium ion by factor of 100/1 -NH3 also present because it can cross membranes -Glutamate can be oxidatively deaminated by glutamate dehydrogenase to produce NH4 and α-ketoglutarate (Glutamate NH4 + α-ketoglutarate) using NAD or NADP in mitochondria. Readily reversible and ammonium can be interconverted -Many other AA can lose nitrogen as NH4+ -Histidine Urocanate -Serine/Threonine deaminations require pyridoxal phosphate catalyzed by serine dehydratase -Glutamine and Arginine have R groups can be released as NH4 -Asparagine deamidated by asparaginase yielding aspartate and NH4 -Glutaminase acts on glutamine, important in kidney where NH4 excreted -in muscle/brain, purine nucleotide cycle allows NH4 to be released from AA -glutamate collects N and transfers it to oxaloacetate to form aspartate which supplies nitrogen to purine nucleotide cycle, which releases fumarate and NH4 3. Role of Glutamate in Metabolism of Amino Acid Nitrogen – glutamate involved in synthesis and degradation of amino acids -provides N for AA synthesis, and obtains its own nitrogen by transamination reactions or from NH4 by glutamate dehydrogenase -When AA are degraded, glutamate collects N from other amino acids by transamination reactions, some of which is released by ammonia by glutamate dehydrogenase and march larger amounts of ammonia are produced from other sources -NH4 is the one of the main forms in which nitrogen enters urea cycle -second form of N for urea synthesis is aspartate, from which glutamate is source of N 4. Role of Alanine and Glutamine in Transporting AA Nitrogen to Liver – urea cycle enzymes are primarily in the liver, mechanism is in place to transport AA N to liver -Alanine/glutamine are major transporters of nitrogen in blood -Alanine is exported primarily by muscle; pyruvate alanine by transamination through glutamate, which then travels to liver -in liver, alanine is transaminated to pyruvate, and N is used for urea synthesis while pyruvate is used for gluconeogenesis while glucose exported to muscle for energy -cycling of N between liver and muscle called glucose/alanine cycle -glutamine synthesized from glutamate by fixation of ammonia, ATP, and glutamine synthetase in cells around portal vein -under conditions of rapid AA breakdown, ammonia increases, and glutamate that has been formed from transamination accepts another nitrogen to form glutamine, which travels to liver, kidney, or intestines where glutaminase removes amide to form glutamate + ammonia Urea Cycle – major nitrogen product is urea found in urine; it serves as a disposal of ammonia which is toxic to the CNS. -urea cycle was proposed, called Krebs-Henseleit cycle Reactions of the Urea Cycle – nitrogen enters the cycle as NH4 and aspartate to form carbamoyl phosphate, which reacts with ornithine to form citrulline -ornithine initiates and is regenerated by the cycle -aspartate reacts with citrulline to donate its nitrogen to urea after forming arginine -cleavage of arginine by arginase releases urea and regenerates ornithine CO2 + H2O HCO3 + NH4 Carbamoyl Phosphate + Ornithine Citrulline Aspartate Argininosuccinate Arginine Ornithine + Urea 1. Synthesis of Carbamoyl Phosphate – NH4, HCO3 + ATP react to form carbamoyl phosphate with the help of carbamoyl phosphate synthetase (CPSI) 2. Production of Arginine by Urea Cycle – in the mitochondria, carbamoyl phosphate reacts with ornithine to form citrulline and is catalyzed by ornithine transcarbamoylase (OTC) -product is transported across mit. membrane in exchange for cytoplasmic ornithine -citrulline reacts with aspartate in cytoplasm argininosuccinate (argininosuccinate synthetase) driven by ATPAMP + P2 and aspartate comes from deamination of oxaloacetate -Argininosuccinate cleaved by argininosuccinate lyase fumarate and arginine -fumarate converted to malate used for gluconeogenesis or for regeneration of oxaloacetate by TCA cycle -oxaloacetate that is formed is transaminated to aspartate which carries N to urea cycle ***Clinical correlate – ornithine transcarbamoylase deficiency causes carbamoyl phosphate to accumulate and flood pyrimidine biosynthesis instead of enter urea cycle, causing an excess amount of orotic acid (orotate) to be excreted in urine with no ill effects 3. Cleavage of Arginine to Produce Urea – Arginine, containing N from NH4 and aspartate, is cleaved by arginase to produce urea and regenerate ornithine -urea is produced from the guanidinium group on side chain of arginine -ornithine is transported back into the mitochondria in exchange for citrulline Origin of Ornithine – ornithine is an amino acid not incorporated into protein synthesis because it has no codon. Apart from being regenerated by urea cycle, ornithine can be synthesized de novo catalyzed by ornithine aminotransferase in the intestine, converting glutamate semialdehyde to ornithine in the first step Regulation of Urea Cycle – urea cycle is regulated by substrate availability; the higher the rate of ammonia production, the higher is the rate of urea formation (regulation by substrate availability is common among disposal pathways, and is a common feed-forward regulation) -allosteric activation of CSPI by N-acetylglutamate (NAG) positively regulates urea cycle. NAG is only formed to induce CPSI and has no known functions otherwise -NAG is formed from acetyl-coA and glutamate and is stimulated by arginine -Glutamate + Acetyl-CoA N-Acetylglutamate (induced by arginine) -as arginine increases in liver, two reactions are stimulated 1. Synthesis of N-acetylglutamate, which increases rate of carbamoyl phosphate production 2. Production of more ornithine via arginase reaction so that cycle can be rapid -Urea cycle also regulated by induction of urea-cycle enzymes in response to conditions that require increased protein metabolism such as high-protein diet or prolonged fasting, where in both conditions amino acid nitrogen is converted to urea Function of Urea Cycle During Fasting – during fasting, liver maintains blood glucose, and amino acids from muscle protein are a major carbon source for production of glucose by gluconeogenesis -as AA carbons converted to glucose, nitrogens are converted to urea, this urinary excretion of urea is high during fasting -as fasting proceeds, brain starts to use ketone bodies, and not so much glucose is needed, so less muscle protein is cleaved for gluconeogenesis which causes decreased production of urea -major amino acid substrate for gluconeogenesis is alanine, which is synthesized in peripheral tissues to act as a nitrogen carrier -glucagon release during fasting stimulates alanine transport into liver by activating transcription of transport systems for alanine -2 molecules of alanine glucose, and the nitrogen of 2 alanines 1 urea -NH4+ is a toxin that results from degradation of urea or proteins by intestinal bacteria and is not metabolized by the infected liver -elevation of NH4 in brain fluid causes depletion of TCA intermediates and ATP in CNS -α-ketoglutarate combines with NH3 to form glutamate by glutamate dehydrogenase and glutamate + NH3 glutamine -GABA (gamma aminobutyric acid), an inhibitory neurotransmitter is shunted into systemic circulation from gut lumen in patients with hepatic failure -In addition to producing urea, reactions of TCA biosynthesize arginine, making arginine not an essential AA in the diet, but urea cannot be cleaved by humans because Urease is only produced by bacteria -1/4th of all urea released by liver each day is recycled by bacteria Disorders of Urea Cycle – accumulation of ammonia is dangerous in circulation, as it is toxic to CNS, so levels in the body must be controlled. -free ammonia is fixed into α-ketoglutarate or glutamate (through glutamate dehydrogenase to form glutamate and glutamine synthetase to form glutamamine, respectively). -glutamine can be used by liver; as nitrogens removed from carriers, CPSI fixes NH3 into carbamoyl phosphate to initiate urea cycle -when urea cycle enzyme is defective, cycle is interrupted and intermediates accumulate -if there is a block, glutamine levels rise in the blood, and because a-ketoglutarte levels are too low to fix free ammonia, elevated ammonia is found in the blood -any urea-cycle enzyme defect causes glutamine accumulation and high ammonia in the blood -Ammonia toxicity will lead to brain swelling due to osmotic imbalance caused by high levels of ammonia and glutamine in astrocytes -as ammonia levels rise in astrocytes, more glutamine is produced to exacerbate imbalance -ammonia levels inhibit glutaminase to lead to glutamine elevation -high levels of glutamine alter permeability of mitochondrial membrane to open the mitochondrial permeability transition pore, which leads to cell death -absence of glutamate is due to high ammonia, which causes brain dysfunction since glutamate is a neurotransmitter, can cause lethargy and CNS activity reduction -most common urea-cycle defect is OTC deficiency, X-linked disorder -major clinical problem with urea-cycle defects in the effect of excessive blood ammonia on CNS, which can lead to irreversible neuronal damage and mental retardation -low-protein diets re essential to reduce potential for excessive amino acid degradation -drugs are used to form conjugates with amino acids, most frequent are benzoic acid and phenylbutyrate -phenylacetate has a bad odor. Phenylactete forms a conjugate with glutamine which is excreted and removed two nitrogens per molecule -benzoic acid, after activation reacts with glycine to form hippuric acid which is excreted -as glycine is synthesized from serine, body now uses nitrogens to synthesize serine, so more glycine can be produced -gene therapy experiments can be used on people with OTC deficiencies