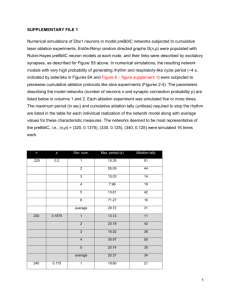
Results Characteristics of Two Patients who showed Multiple
advertisement

Results Characteristics of Two Patients who showed Multiple Morphologies of Ventricular Tachycardia after Initial Ablation In these 2 patients, two or three different morphologies of VT were induced after several attempts of ablation. In one, the first VT originated from the aortomitral continuity region where it was terminated with ablation, but two different morphologies of VTs (both RBBB pattern) were then induced with axes that shifted from inferior leftward to inferior rightward and further ablation extending leftward along the mitral annulus abolished inducible VT. VT was not inducible during isoproterenol infusion after final ablation. In the second patient with VTs were thought to originate from scar between the right coronary cusp (RCC) and the septal RVOT. Ablation was performed in the RCC and then on the adjacent side of the RVOT area, two different morphologies of VTs, with a left bundle branch block pattern with transition at V2 or less inferiorly directed axis (shifting from 80 degrees to 45°), were induced; and further ablation at RCC and left coronary cusp junction rendered all VTs noninducible. Ablation of Ventricular Tachycardia in Inducible Group Fifteen (52%) of the 29 VTi group had ablation lesions placed during sustained VT. Among the remaining 15 in whom RF application was started during sinus rhythm, 4 patients (27%) had sustained VT emerge during ablation, and 8 patients (53%) showed PVCs or nonsustained VT consistent with automaticity during ablation. Among 19 patients who had ablation lesions during sustained VT, 12 (63%) patients had termination of VT during ablation, whereas 7 patients did not have termination of VT during that ablation application (supplementary figure 2). The average time to termination of VT during ablation was 2.3 ± 1.7s (range 0.3 to 3.7s). In the MM group ablation was performed less frequently in the RVOT compared to the SM group (18% vs. 88%, p<0.001). Supplementary figure 1. Tracings from a patient who had successful ablation. Sustained VT was easily induced by rapid ventricular pacing. Earliest activation site was found at RVOT free wall (panel B). Ablation terminated VT at 2.2 seconds (panel A). The 12-lead ECG of VT showed a left bundle branch block configuration with inferior axis QRS morphology (panel C). Supplementary figure 2. Tracings from a patient in the VTni group who had successful ablation. Only nonsustained VT was induced despite high dose isoproterenol infusion and programmed ventricular stimulation (panel A). Earliest activation was found at the RVOT. During ablation, nonsustained VT disappeared, and no arrhythmia was inducible after ablation (panel B). The 12-lead ECG of nonsustained VT showed left bundle branch block with inferior axis QRS complexes, and well matched with pace-mapping (panel C).