iROLL – Does 3-D radioguided occult lesion localization improve
advertisement

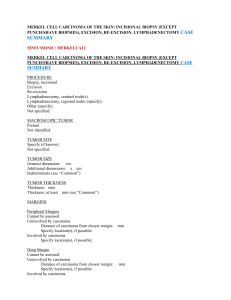
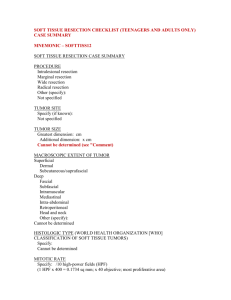
SUPPLEMENTARY MATERIAL iROLL – Does 3-D radioguided occult lesion localization improve surgical management in early-stage breast cancer? Authors Christina Bluemel1, Andreas Cramer2, Christoph Grossmann2, Georg W. Kajdi1, Uwe Malzahn3, Nora Lamp4, Heinz-Jakob Langen5, Jan Schmid1, Andreas K. Buck1, Hanns-Jörg Grimminger2, Ken Herrmann1 Affiliations 1 Department of Nuclear Medicine, University Hospital of Würzburg, Würzburg, Germany 2 Department of Obstetrics and Gynecology, Missionsärztliches Klinikum Würzburg, Würzburg, Germany 3 Institute of Clinical Epidemiology and Biometry, University of Würzburg, Würzburg, Germany 4 Institute of Pathology, University of Würzburg, Würzburg, Germany 5 Department of Radiology, Missionsärztliches Klinikum Würzburg, Würzburg, Germany Short title iROLL in breast cancer Corresponding author Christina Bluemel, MD Department of Nuclear Medicine, University Hospital of Würzburg Oberdürrbacher Str. 6 97080 Würzburg Tel.: +49931-20135983 Fax: +49931-201635405 Email: Bluemel_c@ukw.de 1 file 1: Imaging Protocol Five minutes after intratumoral injection of 99m Tc-nanocolloid, planar images were acquired from ventral and lateral (2 min each) on a dual-head gamma camera or a hybrid camera (e.cam or SymbiaT, Siemens, Erlangen, Germany) equipped with low-energy high-resolution collimators (140 keV, 15% window). Next, 76±8 MBq (range 60–91 MBq) 99m Tc-nanocolloid was injected periareolarly in four deposits (0.2 ml each). Then planar images (ventral and lateral, 5 min each) with and without lead shielding and a 57 Co flood source were acquired (Fig. 2b). Late imaging 1–2 h after injection was performed in all patients. In one patient (3%) with no detectable SLN, planar images were again acquired at 4 h post injection. In the case of aberrant lymphatic drainage (n=1; 3%), SPECT/CT imaging was performed (128×128 matrix, 40 frames, 20 s/frame and CARE Dose modulation, 130 kV, and B30s kernel). The location(s) of the SLNs were marked with indelible ink on the overlying skin. file 2: depth and distance measurements using fhSPECT FhSPECT provides a 3-D navigation tool to measure the distance between the probe tip and the center of the injected activity, which is displayed on the screen of the fhSPECT as shown in Fig.2c,e in plane images or in a 3-D mode (Fig.5). In the present study this tool was used in the pre-incision scan to determine the distance between the body surface and the tumor, as such the center of the intratumorally injected activity. This distance was compared to the preoperative ultrasound, assuming that the center of the injected activity is next to the needle tip used for intratumoral injection of the 99m Tc-nanocolloids. The 3-D tool was also used in the specimen scans for the assessment of the tumor free margins additionally to only visual assessment of the tumor position within the resected breast tissue. For calculation of the distances between the tumor and the specimen planes, which were compared to histopathologically measured margins, the measurements were corrected by half of the tumor size as shown in suppl.Fig.2. To simulate the 3-D volume of the tumor, measurements were performed from 6 different directions corresponding to those determined by histopathologic analysis (Fig. 2f and suppl.Fig.2). 2 Supplementary figure 1: 3-D mode of distance measurement Measurement of the distance between the probe tip and the hottest part (green, crosshairs) of the intratumorally injected activity is measured (in this case 6 mm) Supplementary figure 2: Specimen measurements In each resected breast specimen the distances between the tumor and the resection planes were determined from 6 different directions (ventral and dorsal not shown in the figure) corresponding to the histopathologically assessed directions. It was assumed that the 99m Tc-nanocolloid was injected in the center of the tumor, and accordingly the distances measured with fhSPECT (probe tip to the center of the injected activity; read arrows) were corrected by the half of the tumor size. The yellow arrow displays the calculated distance, which was compared to histopathology. file 3: Histopathology SLNs and axillary lymph node dissection First the number and size of lymph nodes in fresh, unfixed tissue samples obtained from axillae were assessed. Each LN was cut along the longest pole-to-pole diameter or longitudinally through the hilum (slices of 2–3 mm thickness). All nodes were subjected to frozen sectioning and stained with H&E. If metastasis was present, the largest dimension of infiltrate and, when present, extranodal growth was reported (micrometastasis ≤2 mm, metastasis >2 mm). The remaining perinodal tissue was fixed in 4% neutral buffered formalin and embedded in paraffin as well as the nodes after thawing. From each paraffin block, two consecutive slices were mounted every 500 μm throughout the entire block and numbered 1 and 2. Each number 1 section was stained with H&E, while the second section was 3 retained. Metastases were reported as described above. If metastasis was detected during frozen sectioning, axillary lymph node dissection was performed. This tissue was fixed in 4% neutral buffered formalin. The number and size of the lymph nodes were assessed. Depending on their size, the lymph nodes were cut along the longest pole-to-pole diameter or longitudinally through the hilum (slices of 2–3 mm thickness). The nodes were embedded completely or, if macroscopically a metastasis was suspected, representative material was embedded. From each paraffin block, a section was stained with H&E. Metastasis was reported as described above. Breast specimen Resected breast specimen was fixed in 4% neutral buffered formalin for 24 h. For orientation the specimen was marked with titan clips and sutures. Also a sketch of anatomic localization in the breast was given to the pathologist. First the specimen was weighed and the greatest diameter of each dimension was measured. For histopathologic orientation the specimen was marked with different tissue colors and afterwards the tissue was cut along the greatest dimension in slices of 3–4 mm thickness. The size of the macroscopic visible tumor was determined in three dimensions and its closest distance to the resection margins in each direction was measured. Representative material was embedded, and sections from each block were stained with H&E. The definitive distance to the resection margins was determined histologically in millimeters up to 10 mm (any greater distance was given as >10 mm). file 4: Sentinel lymph node biopsy Preoperative lymphoscintigraphy successfully identified SLNs in 97% (30/31) of the patients, including drainage to the internal mammary chain lymph nodes in one patient (3%). No SLN was found in one patient despite late image acquisition after 4 h and reinjection of 30 MBq 99m Tc- nanocolloid. In 26% (8/31) of the patients the SLN could already be detected after the intratumoral injection. The fhSPECT-derived intraoperative detection rate of the preoperatively radiolabeled SLNs was 100% (30/30). In the patient with negative lymphoscintigraphy, an SLN was identified using blue dye. The mean number of SLNs resected per patient was 2±1 (range 1–4).. In 13% (4/31) of the patients up to three metastasized lymph nodes of ≤2 mm (pN1a) were found. Nodes resected due to suspicious palpation (13% of the patients) as well as the radiocolloid-negative but blue dye-positive lymph node did not contain tumor cells. In patients with positive SLNs, axillary lymph node dissection was performed without proof of additional metastasized lymph nodes. file 5: Table: Distance measurements by fhSPECT* (n=164#) compared with histopathology ROC analysis could not identify an optimal cut-off value in fhSPECT distance measurements for the prediction of tumor-positive (≤1 mm) or close (≤3 mm) surgical margins. 4 Histopathologic distances (n) ≤3 mm vs. >3 mm ≤3 mm >3 mm ≤1 mm vs. >1 mm ≤1 mm >1 mm fhSPECT distances [median, mean±SD (range)] 7 mm, 9.4±7.6 (-3 – 30) mm 11 mm, 12.4±9.6 (-6 – 49) mm 7 mm, 10.3±7.9 (0 – 30) mm 9.5 mm, 11.9±10.1 ( -6 – 49) mm * Measurements by fhSPECT were corrected by half of the tumor size, assuming that the injection was in the centroid of the lesion; therefore negative distances were possible; n number of distance measurements in the subgroup; # not all 186 measurements (six directions per specimen) were available owing to false tracking or failure to perform measurements in each direction. 5