Integration of Primary Care and Behavioral Health
Integration of Primary Care and Behavioral Health
Nancy V. Wallace, MSN, FNP
Daily Planet Healthcare for the Homeless
VACPN Conference
October 14, 2011
Learning Objectives
Define integrated care
Explain the need for integrated care
Describe various models of integrated care
Identify benefits to integration of care
Identify challenges to overcome in the effort to deliver integrated care
Primary care
Behavioral health
Collaborative care
Integrated care
DEFINE INTEGRATION
Primary Care
The medical setting where patients receive most of their medical care and is therefore the first source for treatment
Family medicine
General medicine
Pediatrics
OB-GYN (sometimes)
Behavioral Health
Includes both mental health and substance abuse services
In the US, is most often delivered in separate specialty clinics
Often, substance abuse treatment and mental health treatment are delivered in separate facilities
Collaboration vs. Integration
Collaboration
Involves BH working with primary care
Clients perceive that they are getting care from a specialist who collaborates closely with their PCP
Integration
Involves BH working within primary care
Clients perceive BH services as a routine part of their health care
Biopsychosocial model
Biological, psychological, and social factors all play a significant role in human functioning in the context of disease
Often endorsed, seldom practiced
The burden of mental illness is high
You can ’t separate the mind and body
Healthy behaviors decrease when mental health is poor
There are medical benefits to good mental health
THE NEED TO INTEGRATE
CARE
The Burden of Mental Illness
In 2008, NIMH estimated that 1 in 4 adults suffer from a diagnosable mental disorder
Mental illness begins early in life (1/2 by age 14 and ¾ by age 24)
Mental illness is a chronic disease of the young
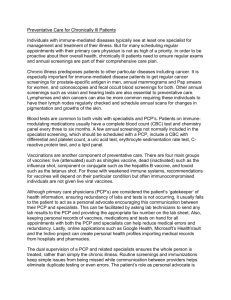
You can ’t separate the mind and body
Physical health problems and mental health problems are correlated
Those with serious medical problems often have co-morbid mental health problems
As many as 70% of primary care visits stem from psychosocial issues
Healthy behaviors decrease when mental health is poor
Tobacco use among those diagnosed with mental illness is TWICE that of the general population
Injury rates (intentional and unintentional injuries) are 26 times higher in those with mental illnesses than the general population
Medical Benefits of Good
Mental Health
Decreased risk for disease, illness, and injury
Better immune functioning
Improved coping and quicker recovery
Increased longevity
Lower cardiovascular risk
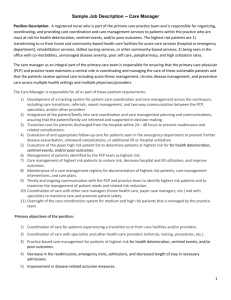
Common concepts
Coordinated, Co-located, Integrated
Specific examples
MODELS OF INTEGRATED
CARE
Concepts common to all integrated care models
The medical home
The healthcare team
Stepped care
Four-quadrant clinical integration
The medical home
NCQA ’s inclusion criteria:
Patient tracking and registry functions
Use of non-physician staff for case management
The adoption of evidence-based guidelines
Patient self-management support and tests(screenings)
Referral tracking
The healthcare team
The doctor-patient relationship is replaced with a team-patient relationship
Members of the team share responsibility for care. The patient perceives that the team is responsible
Visits are choreographed with various team members (nurse, doctor, CM, pharmacist, etc.)
Stepped care
Causes the least disruption to the person ’s life
Is the least extensive needed for positive results
Is the least intensive needed for positive results
Is the least expensive needed for positive results
Is the least expensive in terms of staff training required to provide effective service
Stepped care (BH example)
1. Provide basic education and refer to self help groups
2. Involve clinicians who provide psycho-educational interventions and make follow up phone calls
3. Involve highly trained BH professionals who use specific practice algorithms
4. Refer to specialty MH system
Four-Quadrant Clinical
Integration
II.
High BH needs/Low
PH needs
IV.
High BH needs/High
PH needs
I.
Low BH needs/Low
PH needs
III.
Low BH needs/High
PH needs
Four-Quadrant Clinical
Integration Service Delivery
II.
Served in primary care and specialty
MH settings
IV.
Served in primary care and specialty
MH settings
I.
Served in primary care setting
III.
Served in primary care setting
Four-Quadrant Clinical
Integration Examples
II.
Patient with bipolar disorder and chronic pain
IV.
Patient with schizophrenia and metabolic syndrome or hepatitis C
I.
Patient with moderate
ETOH abuse and fibromyalgia
III.
Patient with moderate depression and uncontrolled
DM
Wide range of models in practice
Can be thought of as a continuum of
Coordinated Care
Co-located Care
Integrated Care
Most models in practice currently are hybrids of the above models
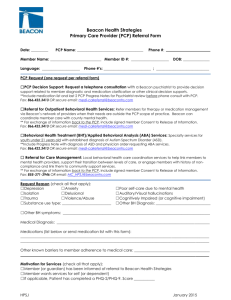
Coordinated care
Routine screening for BH problems conducted in primary care
Referral relationship between PCP and BH settings
Routine exchange of information between both treatment settings
PCP delivers BH interventions using brief algorithms
Connections are made between the patient and community resources
Co-located care
Medical and BH services are located in the same facility
Referral process for medical cases to be seen by BH (and vice versa)
Enhances communication between providers because of proximity
Co-located care
Consultation between providers to increase the skills of both
Increase in the level and quality of BH services offered
Significant reduction of “no-shows” for
BH treatment
Integrated care
Medical services and BH services are delivered in the same or separate locations
One treatment plan includes both medical and BH elements
A team working together to deliver care using a prearranged protocol
Integrated care
Teams composed of a physician and one or more of the following: NP, PA, nurse, case manager, family advocate, BH therapist, pharmacist
Use of a database to track the care of patients who are screened into behavioral health services (and vice versa)
A collaboration continuum
MINIMAL
BASIC
At a distance
BASIC
On-site
CLOSE
Partially
Integrated
CLOSE
Fully
Integrated
Collaboration continuum
Minimal
BH and PCP work in separate facilities, have separate systems, and communicate sporadically
Basic Collaboration at a distance
PCP and BH providers have separate systems at separate sites but now engage in periodic communication about shared patients
Collaboration continuum
Basic collaboration on-site
BH and PCP have separate systems but share the same facility. Proximity allows for more communication, but each provider remains in his or her own professional culture
Collaboration continuum
Close collaboration in a partially integrated system
BH professionals and PCP share same facility and have some systems in common (i.e. scheduling, medical records). Physical proximity allows for face to face communication between providers. There is a sense of being part of a larger team.
Collaboration continuum
Close collaboration in a fully integrated system
The BH and PCP are part of the same team. The patient experiences the BH treatment as part of his or her regular primary care
For the patient
For the providers
BENEFITS TO INTEGRATED
CARE
Benefits to integrated care
Patient
Improved health outcomes
Greater engagement in participating in own care
Decreased risk for adverse events
Increased access to services (less stigma, more convenient)
Provider
Practice as a part of a team who's members support each other ’s efforts to help improve the heath of patients
Learn from other providers
Potential payment incentives
CHALLENGES TO OVERCOME
TO FULLY INTEGRATE CARE
Challenges to overcome
Psychiatric resources are scarce
Telemedicine
Mentoring relationships
Primary care resources are scarce
Utilize non-physician staff (NPs, PAs)
Challenges to overcome
Privacy concerns limit access to patient records across disciplines
HIPPA allows for sharing information for the purpose of care coordination without a formal consent. State laws are sometimes more strict
There is discussion regarding federal regulation CFR 42 (which regulates SA services information) to allow sharing of information for the purpose of treatment coordination
Challenges to overcome
Payment and parity issues
Medical home models typically receive a
“per-member-per-month” fee, perhaps the fee could be enhanced for members in higher value quadrants
References
Collins, C. 2010. Evolving Models of Behavioral Health
Integration in Primary Care. New York, NY:Milbank Memorial
Fund.
Mauer, B. 2009. Behavioral Health/Primary Care Integration and the Person-Centered Healthcare Home. Washington,
DC: National Council for Community Behavioral Healthcare.
Available at http://www.allhealth.org/BriefingMaterials/BehavioralHealtha ndPrimaryCareIntegrationandthePer son-
CenteredHealthcareHome-1547.pdf.
Centers for Disease Control and Prevention. Public Health
Action Plan to Integrate Mental Health Promotion and Mental
Illness Prevention with Chronic Disease Prevention, 2011 –
2015. Atlanta: U.S. Department of Health and Human
Services; 2011.
Discussion
Do you have any questions about the presentation?
Are there any questions about my practice?
What are you doing in your practices?
What challenges have you faced?
Any good outcomes or client feedback?