liver abscesses
advertisement
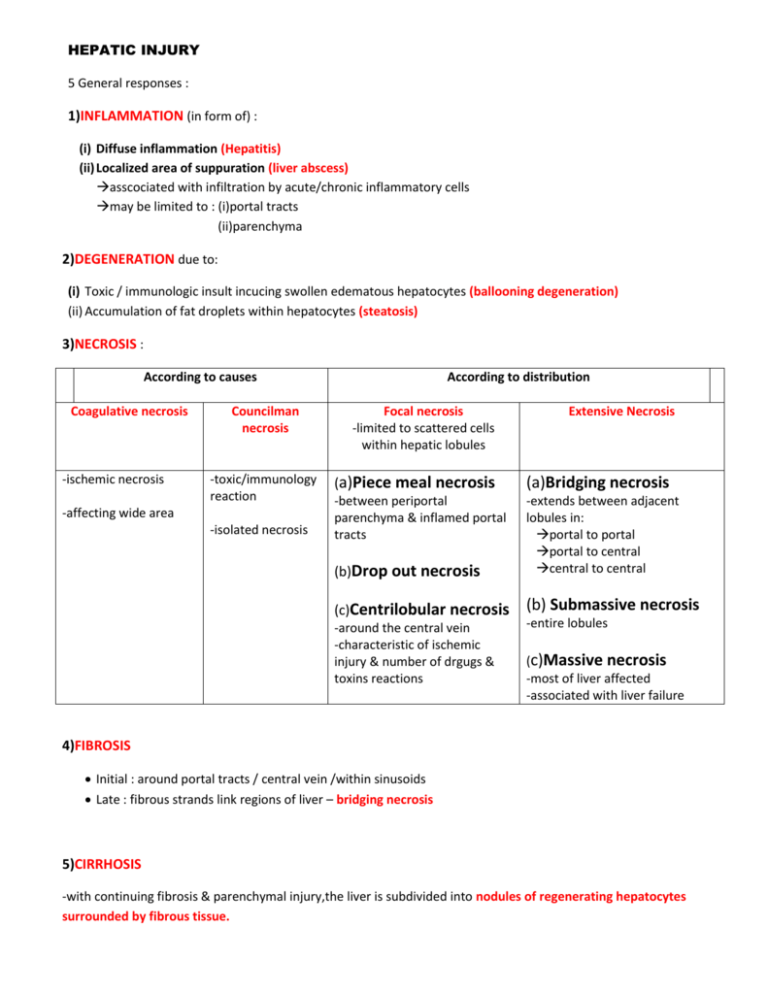
HEPATIC INJURY 5 General responses : 1)INFLAMMATION (in form of) : (i) Diffuse inflammation (Hepatitis) (ii) Localized area of suppuration (liver abscess) asscociated with infiltration by acute/chronic inflammatory cells may be limited to : (i)portal tracts (ii)parenchyma 2)DEGENERATION due to: (i) Toxic / immunologic insult incucing swollen edematous hepatocytes (ballooning degeneration) (ii) Accumulation of fat droplets within hepatocytes (steatosis) 3)NECROSIS : According to causes Coagulative necrosis -ischemic necrosis Councilman necrosis -toxic/immunology reaction -affecting wide area -isolated necrosis According to distribution Focal necrosis -limited to scattered cells within hepatic lobules Extensive Necrosis (a)Piece meal necrosis (a)Bridging necrosis -between periportal parenchyma & inflamed portal tracts (b)Drop out necrosis -extends between adjacent lobules in: portal to portal portal to central central to central (c)Centrilobular necrosis (b) Submassive necrosis -around the central vein -characteristic of ischemic injury & number of drgugs & toxins reactions -entire lobules (c)Massive necrosis -most of liver affected -associated with liver failure 4)FIBROSIS Initial : around portal tracts / central vein /within sinusoids Late : fibrous strands link regions of liver – bridging necrosis 5)CIRRHOSIS -with continuing fibrosis & parenchymal injury,the liver is subdivided into nodules of regenerating hepatocytes surrounded by fibrous tissue. LIVER ABSCESSES Developing countries liver abscesses due to parastic infections Western countries most are pyogenic due to bacterial or fungal infections Sources of pyogenic infections (reach liver through): (i) Ascending infection in biliary tract (ascending cholangitis) (ii) Vascular seedling through portal vein or arterial supply (iii) Direct infection of the liver from a nearby organ (iv) Penetrating injuries Morphology: Pyogenic liver abscess Amoebic liver abscess - Solitary /multiple - Usually SOLITARY - Small / large - Formed of necrotic tissue - Bacteremic spread through arterial/portal system produce small multiple abscess - But NO PUS (note a true abscess) - Direct extension & trauma cause SOLITARY LARGE abscess - Biliary abscess are asscociated with purulent material in adjacent liver ducts CLINICAL FEATURES - Fever - Right upper quandrant pain - Tenderness - Hepatomegaly - Jaundice may occur due to extrahepatic biliary obstruction COMPLICATIONS (i) Rupture of subscapular hepatic abscess lead to: Peritonitis Localized peritoneal abscess (ii) Rupture of amoebic abscess lead to: Amaebic abscess in subdiaphragmatic region which may burrow into thoracic cavity to produce empyema or lung abscess LIVER CIRRHOSIS Definiton : (i) clinically : diffuse chronic progressive liver disease (ii)pathologically : end stage of liver disease Characteristics (criteria) : 1) Diffuse parenchymal injury in form of hepatocellular necrosis 2) Healing by: (a)Bridging fibrous septa form of delicate bands or broad scars replacing & connecting multiple adjacent lobules (b)Formation of regenerating nodules micronodules or macronodules 3) Loss of normal architecture of liver ETIOLOGIC CLASSFICATIONS OF CIRRHOSIS 1) 2) 3) 4) 5) 6) 7) 8) Post hepatic cirrhosis mainly due to HBV & HCV Alcoholic cirrhosis (Laennec’s cirrhosis / portal cirrhosis) Biliary cirrhosis Genetic hemochromatosis Wilson’s disease (rare) α1 antitrypsin deficiency (rare) cryptogenic cirrhosis Others : drugs, galactosemia, tyrosinosis, diffuse infiltrative cancer ,syphillis and severe cases of central hepatic necrosis PATHOGENESIS : “Continuing liver cell necrosis and it’s replacement by progressive fibrosis” 1) Injured hepatocytes & infllammed cells release cytokines stimulate Ito cells secrete type I & III collagens Form fibrous tissue 2) Necrotic walls being replace by regenerating hepatocytes regenerating nodules 3) Net result : (i) Severe distruption of bloodflow and impaired diffusion of solutes (esp. albumin ,clotting factors,lipoproteins) (ii) Obstruction of portal circulation porto-systemic shunts splanchnic congestion & ascites Gross Early : enlarged liver Progression : become smaller due to cell loss & fibrosis Firm consistency Microscopically Early : fibrous septa are delicate and extend through sinusoids Progression : wider bands of fibrous tissue (scar) surrounds regenerating nodules in which regenerating hepatocytes organized into irregular plates Multiple nodules (micro /macronodular) Clinical Features Complications -may be silent 1) -1st sign : complications of portal hypertension ascites splenomegaly caput medusae hematemesis hepatic encephalopathy liver failure 2) Portal hypertension -non-specific symptoms : malaise anorexia weakness weight loss -followed by jaundice,ascites & peripheral edema -Biochemically : elevation of serum transaminase level hyperbilirubinemia alkaline phosphatase hypoproteinemia anemia 3) Liver failure Hepatocellular carcinoma Post necrotic Cirrhosis Alcoholic Cirrhosis (Laennec’s /Portal Cirrhosis) -most common type in egypt -common type in Western countries Causes: -mainly by HCV (25%) -starts with fatty liver -HBV (1 -5 %) -history of acute liver damage caused by hepatotoxins or drugs Morphology: (i) exhibits nodules of varying size (ii) broad bands of scarring (iii) shrunken liver due to severe collapse Morphology : Early : (i) enlarged (ii)yellow-tan colour (iii)greasy Late : (i) size decreases (ii)brown colour (iii)uniformly sized micronodules (iv)mixed micronodular& macronodular pattern Microscopically : (i)Broad bands of fibrous tissue (ii)Mallory bodies degenerated hepatocytes showing eosinophilic cytoplasmic inclusions are characteristics BUT NOT specific features of alcoholic liver disease BILIARY CIRRHOSIS Causes :Obstruction/ destruction of the intrahepatic or extrahepatic branches of biliary tree Clinical features: - Onset is insidious Pruritis ( due to retention of bile & bile salts) Jaundice Portal hypertension Liver failure Increase serum level alkaline phosphatase Increase cholestrol level (markers of cholestasis) Gross : - Yellow –green pigmentation - Finely granular external surface Primary Biliary cirrhosis Etiology : - an autoimmune disease - characterized by primary destruction of the intrahepatic biliary branches by granulomatous inflammation. - Scarring which progress into liver cirrhosis & Failure Age: - Middle-aged women - Peak incidence 40-50 years old - Formation of autoantibodies especially antimitochondrial Ab (90% cases) Microscopically Secondary Biliary Cirrhosis Etiology : - Prolonged obstruction of extrahepatic biliary tree resulting liver damage Cause of obstruction: (i) Gall stones (most common) (ii) Congenital biliary atresia (iii) Maglinancies of biliary trees and head of pancrease (iv) Stricture from previous surgical procedure Microscopically - inflammatory infiltrate within portal tracts - followed by fibrosis & scarring - inflammatory infiltrate within portal tracts - followed by fibrosis & scarring - Inflammation is granulomatous - mixture of acute & chronic inflammatory cells - Interlobular bile ducts are destroyed - interlobular bile ducts are: dilated contained inspissated bile (bile thrombi) proliferation os smaller bile ductules - End stage is indistinguishable from other forms of cirrhosis - End stage is indistinguishable from other forms of cirrhosis Genetic (primary) Hemochromatosis Def : - A systemic autososomal recessive(AR) disorder - Characterized by elevated serum iron - with excessive accumulation o f hemosiderin in body (liver,pancreas,myocardium,skin,synovial membrane & endocrine glands) Pathogenesis ; primary defect in intestinal absorption of dietary iron resulting excessive iron absorption increase serum level 1/3 accumulates in liver liver injury Clinical features: - usually affects male - rarely becomes evident before 5th decade of life - liver cirrhosis ( 100% cases) - panceatic fibrosis (80% cases) - Diabetes mellitus (80% cases) - skin pigmentaion (80% cases) - cardiomegaly in some cases - hypogonadisim in some cases - arthritis in some cases Morphology: - micronodular cirrhosis - chocholate in colour Causes of death: - liver cirrhosis & it’s complications - hepatocellular carcinoma - cardiac dysfunction (arrythymia,cardiomyopathy) Wilson’s Disease Def: - autosomal recessive (AR) disorder of copper metabolism - marked toxic levelsof copper in many tissues (liver , eye ,brain) Pathogenenis : copper absorption & transport ARE NORMAL absorped copper FAILS to form ceruloplasmin absorped copper fails to reach circulation Accumlate in liver age of 5 :non-ceruloplasmin bound copper spills into circulation Hemolysis & pathologic changes at other organs Morphology of liver: - mild to severe damage (fatty change,acute & chronic hepatitis,cirrhosis) - intracellular accumulation of copper Clinical features : -rarely manifest itself before age of 6 Most common: (i) Chronic hepatitis/cirrhosis (ii) Associated with elevated hepatic copper level (iii) Increased urinary excretion of copper (iv) Decreased serum level of ceruloplasmin Others: (i) Neuropsychiatric manifestations due to degeneration of basal ganglia in brain (behavourial changes,frank psychosis) (ii) Kayser-Fleischer ring green to brown ring in Descement’s membrane in the limbus of cornea due to copper depostion doesn’t affect the vision α1 antitrypsin deficiency α1 antitrypsin (AAT): plasma glycoprotein synthesized predominantly by hepatocytes a protease inhibitor (particularly neutrophil elactase released at the sites of inflammation) it’s deficiency permits tissue destruction Definition: - Autosomal recessive disorder - Low serum levels of α1 antitrypsin - Abnormalities in gene forming abnormal α1 antitrypsin molecules Accumulation in liver cytoplasm Morphology: Hepatocytes contains strongly positive Periodic acid-Schiff(PAS) stanined around cyoplasmic inclusions of abnormal AAT that persist after application of diastase enzyme Clinical features: (i) Cholestasis in newborn (10-20%) due to swollen hepatocytes (ii) Chronic hepatitis,cirrhois or pulmonary disease in adolescents,adults,older people due to unopposed activity (iii) Hepatocellular carcinoma in 2-3 % homozygous adults due to chronic & continuous irritation Cryptogenic Cirrhosis Hepatic cirrhosis is said CRYPTOGENIC when complete evaluation of the patient failed to identify the cause TUMORS OF THE LIVER BENIGN TUMOURS (uncommon): Cavernous Hemangioma - Most common benign tumor Gross : - Discrete red-blue soft nodules less than 2cm in diameter beneath the liver capsule Microscopically : - Well circumscribed lesions - Composed of vascular channels lined by endothelial cells - Seperated from each other by interverning stroma Compliaction: - May rupture leading to life-threatening intra-abdominal hemorrhage (especially after blind per-cutaneous needle biopsy) Liver Cell Adenoma - Tends to occur in young women - Regresses on discontinuous of the oral contraceptive pills Gross : - Pale-yellow tan - Well demarcated - Frequently bile staineed nodule - Often beneath the liver capsule - May reach up 30 cm Microscopically : - Composed of sheets & cords of cells - Resemble normal hepatocytes BUT with NO portal tracts - May be mistaken with hepatocellular carcinoma Complication: - May rupture particularly during pregenancy due estrogen stimulation lead to intra-abdominal haemorrhage rarely progress to hepatocellular carcinoma MAGLINANT TUMORS PRIMARY TUMORS Type & it’s origin : (i) Hepatocellular carcinoma (hepatocytes-adults) (ii) Hepatoblastoma (hepatocytes-children) (iii) Cholangiosarcoma (intrahepatic bile ducts) (iv) Angiosarcoma (intrahepatic vasculature) METASTATIC TUMORS - Most common maglinant neoplasms involve liver - Origin of maglinant tumor are found anywhere in Body Common primary sites: - Colon - Lung - Breast - Maglinant melanoma Characterized by: - Massive liver enlargement - Multiple nodules - Show central necrosis & umbilication - α-fetoprotein is NOT elevated HEPATOCELLULAR CARCINOMA (HCC) - COMMONEST primary maglinant tumour of liver - Linked strongly prevalance of HBV infection Etiology Age Sex (i) HBV infection chronic carrier state may confer 200 fold increased risk for HCC in adulthood High incidence area : 3rd – 5th decades of life High incidence area : Male to femae ratio 8:1 (ii)HCV infection Low incidence area : 6th – 7th decade of life Low incidence area : Male tofemale ration 3:1 (iii) Liver cirrhosis 80% for those having cirrhosis Due to increased in liver turnover in regenerating nodules cytologic abnormalities due to greater prevalance of HBV,alcoholism & chronic liver disease among males (iv) Aflatoxins a hepatocarcinogen from fungus Aspergillus flavus grows on improperly stored grain &nuts Morphology - Soft mass - Unifocal / multifocal / diffusely infiltrating Microscopically (i) Conventional type (99%) Ranging from well differentiated with intracytoplasmic bile globules to poorly differentiated (ii) Fibrolamellar carcinoma (1%) A rare type Characterized by fibrosis Occurs in young males &females (20-40 years old) NO association with CIRRHOSIS / OTHER RISK FACTORS Distinctly better prognosis Clinical Feature & Laboratory Findings (i) Rapid increase in liver size (ii) Pain (due to involvement of hepatic capsule) (iii) Loss ofweight (iv) Ascites portal hypertension (v) Paraneoplastic syndrome (ectopic hormones) Insulin-like polypeptide hypogycemia Erythropoeitin polycythemia Parathyroid-like hormone hypercalcemia (vi) 90% of patients have elevated α-fetoprotein (>1000 ng/ml) Spread tends to metastasis early (i) Direct spread dipharagm,pleural or peritoneal cavity (ii) Blood stream lumgs (iii) Lymphatics regional lymph nodes Prognosis natural history is grim death occurs within 6 months of diagnosis Best prevention : -comphrehensive program for immunizing high risk world population against HBV Cholangiosarcoma - Uncommon tumor Angiosarcoma - Rare - Originates from the intrahepatic biliary tree - Most arise without evidence/antecedent risk conditions - Highly maglinant vascular tumor - NOT associated with hepatitis / cirrhosis - Linked to : Gross: - Indistinguishable from HCC Microscopically: - Adenocarcinoma - Mucous production - Abudant fibrous stroma “DESMOPLASTIC REACTION” Lab.Findings: - α-fetoprotein is NOT elevated (i)polyvinyl chloride (plastic industry) (ii)thorotrast (radioactive dye) HEPATIC FAILURE Definition : Loss ofmore than 80 -90 % of the hepatic functional capacity Causes (i) Chronic Liver disease Most common cause (ii) Massive hepatic necrosis Due to fulminant hepatits/drugs (iii) Hepatic dysfunction without overt necrosis Hepatocytes are viable but unable to perform normal metabolic function E.g:Rye’s syndrome Tetracycline toxicity Acute fatty liver of pregnancy Preciptating factors In form of: - GiT bleeding Clinical features (i) Jaundice Mainly form of conjugated Hyperbilirubinemia - Systemic infection - Electrolyte disturbance - Severe stress as major surgery - Heart failure (ii) Hypoalbuminemia Predispose to peripheraledema & ascites (iii) Coagulopathy (iv) Hyperammonemia (v) Fector Hepaticus Formation of mercaptans in gut (vi) Impaired estrogen metabolism &hyperestrogenemia leading to: –gynecomastia –testicular atrophy –palmar erythema –spider angiomas (vii)Hepatic encephalopathy (viii) Hepatorenal failure (ix) Respiratory failure with pneumonia &sepsis (x) Coma usually follow enchephalopathy & preceds death BILIARY TRACTS CHOLELITHIASIS (GALL STONES) -affect 10-20% of all adults populations in developed countries Cholestrol stones - Constitute more than 80% of gallstones - Type : (i)pure cholesterol stones (rare) (ii)mixed stones (common) Pathogenesis: (i) Increased cholestrol level (ii) Decreased bile salts in bile Risk factors (5 F): (i) Female (ii) Above age of 40 years (iii) Ethic group (Native American population) Genetic biliary hypersecretion of cholesterol (iv) Persistent estrogen stimulation During pregnancy Effect of oral contraceptive (v) Obesity (vi) Rapid weight loss (vii) Treatments with hypocholesterolemic agents Morphology: (i)Pure cholesterol stones: SOLITARY oval pale yellow maybe translucent 2-3 cm in length associated with excessive cholesterol in bile (ii)mixed stones mixture of cholesterol ,Ca carbonate, Ca Phosphate and blirubin always MULTIPLE Faceted radio opaqe Pigment stones - Constitute less than 20% of gallstones Pathogenesis: - Presence of excess unconjugated bilirubin in biliary tree (as in chronic hemolytic anaemia) Morphology: - Small - MULTIPLE - FRiABLE - BLACK - Radio opaque - Gall bladder is healthy,NOT inflamed & normal thin wall Complications of gall stones : 1) Chronic Cholecystitis 2) Obstruction of cystic duct at the bladder neck leading to : (i)Acute cholecystitis (ii)Mucocele Gall bladder is transformed into a bag full of bile Bile is graduaaly absorbed Gallbladder is transformed into a bag full of mucus (iii)Emphyema if secondary infection occurs,gallbladder is transformed into bag full of pus 3) Obstruction in of common bile duct leading to: (i)Ascending cholangitis (ii)Obstructive cholestasis (iii)Jaundice (iv)biliary colic is common (v)Acute pancreatitis 4) Gallstone ileus Very rarely May ulcerate intointestine leading to fistula Causing intestinal obstruction 5) Carcinoma of gallbladder Chronic irritation of gallbladder wall by gallstones CHOLECYSTITIS Def : Inflammation of gall bladder Type: Acute cholecystitis -usually associated with gallbladder stones (acute calculous cholecystitis) -absence of gall stones (5-12%) (acute acalculous cholecystitis) Gross: - Enlarged gallbladder - Tense & bright red - Frank pus / gangrenous necrosis - Lumen is filled with turbid bile Microscopically: - Edematous wall - Infiltrated by acute inflammatory cells Acute calculous cholecystitis Acute acalculous cholecystitis - Obstruction by gallstones Occur in seriously ill patients: - Lead to obstruction of bile flow - Postoperative state after major surgery - Distruption of normal (non-biliary surgery) protective glycoprotein - Severe trauma mucous layer - Sever burn - Sepsis - Exposyre of mucosal - Postpartum state epithelium to direct detergent action bile salts & toxic effect of lysolecithin - Increased intraluminal pressure may compromis blood flow - Release of prostagladin leading to inflammation - Occur in absecnce of bacterial infection - Later on,bacterial contaminatin & infectionmay develop Chronic cholecystitis - Occur either as : (i)sequal of repeated bouts of acute cholecystitis (ii)de novo - May occur : (i)chronic calculous cholecystitis (ii)chronic acalculous cholecystitis - Most cases are associted with gallstones - BUT gallstones DO Not play direct role in initiation of inflammation - Cause of chronic cholecystitis is SUPER SATURATION of bile Gross: - Gall bladder wall maybe: contracted normal in size enlarged (when associated with gallstones) Microscopically: - Wall is thickened by fibrosis - Infiltration by chronic inflammatory cells Acute calculous cholecystitis Acute acalculous cholecystitis Chronic cholecystitis Clinical features - Steady upper abdominal pain - Radiating pain to right shoulder - Are markedly obscured by the severe clinical conditions of patients Clinical features - Recurrent attacks of either : steady or colicky epiastric pain right upper quandrant pain - Nausea - Fever - Vomiting - Nausea - Intolerance to fatty meal - Vomitting - Tender,rigid right subcostal region - Conjugated hyperbilirubinemia Course : (i) Mildattacks subsides spontaneously over 1-10 days (ii) Surgical intervention for cholecystectomy Complications of cholecystitis : 1) Superadded infection leading to: empyema cholangitis sepsis 2)Perforation of gall bladder due to gangrenous necrosis leading to local abscess formation diffuse peritonitis - CARCINOMA OF GALL BLADDER Frequency : 5th most common cancer of GIT Age & sex : - Most common in female - Most frequent in 7th decade of life Etiology & Pathogenesis ; Certain factor that lead to recurrent trauma & inflammation : (i) Gallstones (ii) Pyogenic & Parasitic diseases in biliary tree Gross Form of either: - Fungating mass - Diffuse mass infiltrating Microscopically - Adenocarcinoma (majority) - Adenosquamous (rare) - Sq.cell carcinoma (5 %) Spread (i) Local invasion to liver (main) (ii) Extension to cystic ducts & portahepatic lymph nodes (iii)Seedling of the peritoneum & viscera (iv)Metastasis to the lungs Clinical features Insidious & indistinguishable symptoms drom those cause by gall stones Prognosis - Extremely poor - Usually unresectable - Fortunate patients develop early obstruction & acute cholecystitits before their extension to liver