Present moment focus
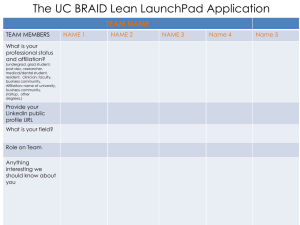
advertisement

Present moment focus - Employing flexible and focused attention to ongoing events. o Alternative: detached focus on conceptualized past, present, or future - Present moment work o Clinical example: Jim begins to describe a distressing experience that occurred last weekend. He reports that he arrived at a reception for his brother and began to experience increasing anxiety mostly around the number of people present and the possibility of inadequate security. He reports that he eventually left the reception. Jim’s speech becomes rapid and his intonation stereotyped as he begins to describe this experience. His posture tightens and his eye contact becomes variable. He begins to repeat himslef, seemingly ruminating over the same ideas of how he “should” have handled this. Jim includes some descriptions of his current experiences, and sometimes appears connected with what he is describing. “Slowing Down” (Advanced work) – Clinician has Julie tell the story, but with prompts to speak more slowly, describe more individual details across sensory, emotional and cognitive domains, and to not offer explanations, just to notice them as thoughts. If Julie had fewer skills in repertoire, clinician might limit to experiences in present, or just to one or two sensory domains. Cognitive Defusion - Experiencing an event fully for its complexity, without certain emotions or cognitions about the event dominating the experience. o Alternative: fusion - Defusion work o Clinical example: Susan is describing struggling to collaborate with doctors to create a satisfactory plan for her diet. It becomes evident as she speaks that she is responding primarily to her classification of foods into “safe” and “dangerous.” “The Buffet” (Early work) – Clinician has Susan imagine foods coming toward her on a conveyer belt. She names the food, and the clinician describes the food, directing Susan’s attention to different aspects of the experience. Depending on Susan’s response, clinician may prompt Susan to try with increasingly “dangerous” foods. If Susan had more skills, clinician might provide less guidance, having Susan describe different aspects of the experience. She might also emphasize “dangerous” foods. Experiential Acceptance - Involves openly embracing one’s experiences, good and bad, without attempting to change them. o Alternative: avoidance Acceptance work o Clinical example: Marsha is describing how self-injury makes her “head shut up,” so she can relax. She describes experiencing it like she is drowning and this is the only thing that “stops the water from rising.” “Floating” (Advanced work) – Clinician extends the metaphor. She directs Marsha to call to mind the experience of feeling waves coming toward her, the water rising around her, and to attend to different aspects of the experience. Clinician then describes two postures, one rigid and one flexible. The rigid posture may be partially effective, but eventually, a big wave comes and the person is knocked down. The flexible posture is sort of uncomfortable because the person is easily lifted and carried by the water this way and that, but even the biggest wave can’t put them on their ass with water over their head because you learn when you’re flexible that you float. The clinician walks slowly through this metaphor, allowing Marsha to supply descriptions or conclusions along the way and wrapping her additions into the metaphor. If Susan had fewer skills, the clinician might not introduce the concept of acceptance, even metaphorically. She might simply have Marsha imagine conditions under which she can accept certain experiences. Transcendent Self-Awareness - Involves contacting different ways of experiencing one’s self flexibly, such that a sense of self that separate from any particular experience emerges. o Alternative: fusion with conceptualized self - Self work o Clinical example: Tonya is describing how “sick” and “screwed up” she is, in contrast to her “perfect” childhood. She attributes her repeated relationship problems to a trauma experienced as a teenager, and attributes that trauma to her “carelessness.” Tonya describes trying to appear perfect, which alienates her from her peers, and completely withdrawing from all activities at the first sign of imperfection. “I-Contact” (Advanced work) – Clinician leads eyes-closed exercise in which Tonya notices specific details of her appearance, ending with her eyes. Then, while Tonya continues to imagine looking into her own eyes, the clinician guides her attention to different experiences she’s had of herself, others, and the world If Tonya had fewer skills, the clinician might have her use an actual mirror instead of imagining. She might also have Tonya do a similar exercise, but with “a person who has struggled like you do” Valued Living - Living in such as way so as to facilitate contact with the way an individual chooses to work and live o Alternative: fused valuing, - Values work o Clinical example: Mark describes a “values conflict” between his painting and being a father. “You Get to Pick” (Advanced) – The clinician asks Mark to describe a specific instance during which the “values conflict” was salient. Clinician directs his attention toward different details of that instance, including the thoughts he had around there being a conflict in values. When Mark proposes abandoning of one or the other, clinician guides Mark’s attention to a moment in which contacts value of painting and value with being a father. Finally clinician guides Marks attention to the idea that painting might serve being a father, and vice versa. If Mark had fewer skills, the clinician might provide more guidance by doing eyes closed exercise. Committed Action - Involves noticing when actions are not consistent with values, and gently turning back to valued living o Alternative: inaction, persistent avoidance - Commitment Work o Clinical example: Beth describes questioning her commitment to her marriage since her husband admitted that he had an affair the last time she was in inpatient treatment for eating problems. She expresses guilt for considering leaving her marriage, saying “a good wife wouldn’t even consider leaving.” “It’s Not in the Cards” (Intermediate) – Clinician asks Beth to write on index cards: 1) three facts or feelings that feel like reasons to hold onto the marriage, 2) three facts or feelings that feel like reasons to leave the marriage, 3) three worries that feel like reasons to leave the marriage, 4) three hopes that feel like reasons to hold onto the marriage, 5) what “saving the marriage” would involve, 6) what “letting go” of the marriage might involve, 7) six possible outcomes for how things turned out 3 to 6 years from now, 8) “and that’s okay” and “and that’s not okay.” Clinician has Beth tell a story using the cards to predict how this should go. Clinician suggests that her choice can be independent of any of the details on the cards. If Beth had more skills, the clinician might end with Beth making a commitment to some small action that is independent of everything that seems to push her in one direction or the other.