New Patient History Form - Eastern Urological Associates
advertisement
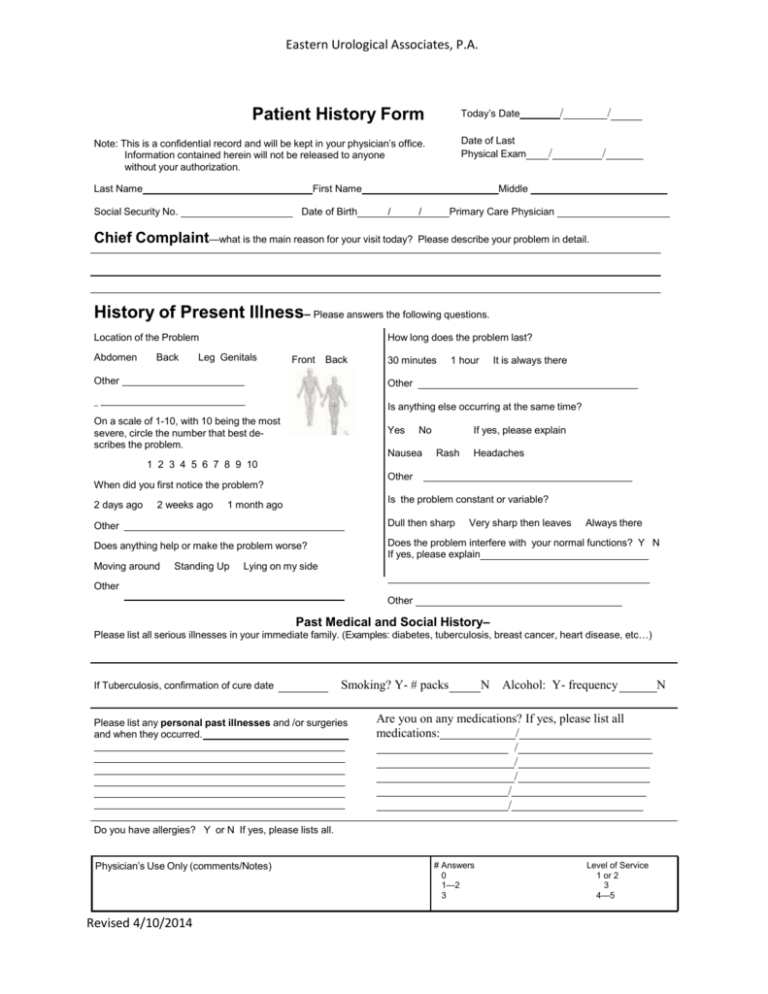
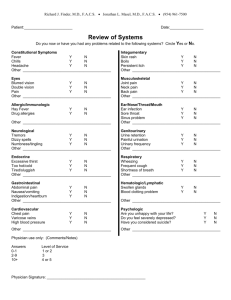
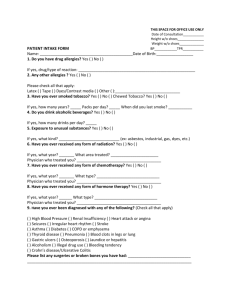
Eastern Urological Associates, P.A. Patient History Form Today’s Date Date of Last Physical Exam Note: This is a confidential record and will be kept in your physician’s office. Information contained herein will not be released to anyone without your authorization. Last Name First Name Social Security No. Date of Birth / / / / Middle / Chief Complaint—what is the main reason for your visit today? / Primary Care Physician Please describe your problem in detail. History of Present Illness– Please answers the following questions. Location of the Problem Abdomen Back How long does the problem last? Leg Genitals Front Back 30 minutes 1 hour It is always there Other Other _ Is anything else occurring at the same time? On a scale of 1-10, with 10 being the most severe, circle the number that best describes the problem. Yes No Nausea If yes, please explain Rash Headaches 1 2 3 4 5 6 7 8 9 10 Other When did you first notice the problem? 2 days ago 2 weeks ago Is the problem constant or variable? 1 month ago Other Dull then sharp Does anything help or make the problem worse? Does the problem interfere with your normal functions? Y N If yes, please explain Moving around Standing Up Very sharp then leaves Always there Lying on my side Other Other Past Medical and Social History– Please list all serious illnesses in your immediate family. (Examples: diabetes, tuberculosis, breast cancer, heart disease, etc…) If Tuberculosis, confirmation of cure date Smoking? Y- # packs Please list any personal past illnesses and /or surgeries and when they occurred. N Alcohol: Y- frequency Are you on any medications? If yes, please list all medications: / / / / / / Do you have allergies? Y or N If yes, please lists all. Physician’s Use Only (comments/Notes) Revised 4/10/2014 # Answers 0 1—2 3 Level of Service 1 or 2 3 4—5 N Last Name Review of Systems First Name Do you now have or have you experienced any problems related to the following systems during the last six months? Circle Y e s or No. Constitutional Symptoms Gastrointestinal Ear/Nose/Throat/Mouth Fever Y N Abdominal pain Y N Ear infection Y N Chills Y N Nausea/vomiting Y N Sore throat Y N Headache Y N Indigestion/ Y N Sinus problems Y N Other heartburn Other Eyes Other Genitourinary Urine retention Y N Blurred vision Y N Cardiovascular Double vision Y N Chest pain Y N Painful urination Y N Pain Y N Varicose veins Y N Urinary frequency Y N High blood pressure Y N Wheezing Y N Frequent cough Y N Y N Other Other Allergic / Immunologic Respiratory Other Hay fever Y N Integumentary Drug allergies Y N Skin rash Y N Boils Y N Shortness of breath Persistent itch Y N Other Other Neurological Tremors Y N Dizzy spells Y N Numbness/tingling Y N Other Hematological/Lymphatic Musculoskeletal Swollen glands Y N Blood clotting problems Y N Joint pain Y N Neck pain Y N Back pain Y N Endocrine Excessive thirst Too hot/cold Y Y Other N Psychological N Other Tired/sluggish Y N Are you generally satisfied with your life? Y N Other Do you feel severely depressed? Y N Have you considered suicide? Y N Other OB/GYN How many pregnancies have you had? ______________ OB How many children do you have? __________________ When was your last menstrual period? ______________ Provider Revised 4/10/2014 #Answer Level of Service 0-1 2-9 10 + Date 1 or 2 3 4 or 5 / /