134_2013_2906_MOESM4_ESM
advertisement

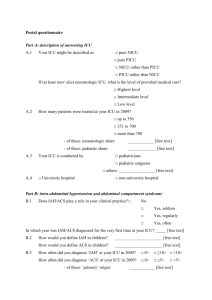
Supplement 4 Section ICU patients at risk for IAH or ACS No., Informal Question 1) Whether to measure IAP Overview of PICOD Structured Clinical Questions PICOD Question Comparator Population Interventions ICU patients IAP measurement No IAP measurement ICU patients with IAH 2) Whether to use APP to guide management ICU patients with IAH IAH management strategies that use APP IAH management strategies that do not consider APP ICU patients with IAH 3) Whether to keep IAP less than 20 mmHg ICU patients with IAH Strategy aimed at keeping IAP less than 20 mmHg No IAP management strategy ICU patients 4) Whether to keep fluid balance neutral or even negative ICU patients Strategy attempting to obtain a neutral or even negative fluid balance after ICU day 3 A comparatively more liberal fluid management strategy Critically injured trauma patients with massive hemorrhage 5) Whether to use damage control resuscitation Critically injured trauma patients with massive hemorrhage No damage control resuscitation ICU patients 6) Whether ICU patients Damage control resuscitation (permissive hypotension, higher ratios of PRBCs to platelets and plasma, and limited crystalloids) Percutaneous Usual care Outcomes Design Mortality, length of hospital or ICU stay, ACS, requirement for decompressive laparotomy, acute renal failure Mortality, length of hospital or ICU stay, ACS, requirement for decompressive laparotomy, acute renal failure Mortality, length of hospital or ICU stay, ACS, requirement for decompressive laparotomy, acute renal failure, healthrelated quality of life Mortality, length of hospital or ICU stay, acute renal failure, ACS, requirement for decompressive laparotomy, IAP Mortality, length of hospital or ICU stay, IAP, ACS, requirement for decompressive laparotomy RCTs, observational studies Mortality, RCTs, RCTs, observational studies RCTs, observational studies RCTs, observational studies RCTs, observational studies with IAH or ACS to use a percutaneous drainage catheter with IAH or ACS catheter drainage of intraabdominal fluid ICU patients with IAH 7) Whether to treat IAH or ACS operatively ICU patients with IAH or ACS Decompressive laparotomy No decompressive laparotomy Trauma or surgery patients requiring open abdominal management 8) Whether to close the fascia or utilize a planned ventral hernia 9a) Whether to use NPWT for temporary abdominal closure ICU patients with open abdominal wounds Fascial closure during the hospital stay Use of the planned ventral hernia, skin grafts, and/or delayed fascial closure Trauma or surgery patients requiring open abdominal management Same ABThera open abdomen NPT system, KCI VAC, or Barker’s vacuum pack technique ABThera open abdomen NPT system, KCI VAC Any other TAC technique Same ABThera open abdomen NPT system KCI VAC Trauma or surgery patients with open abdominal wounds Acute components separation No components separation 9b) Whether to use commercial NPWT for temporary abdominal closure 9c) Choice of commercial NPWT for temporary abdominal closure 10_ Whether to use acute components separation Barker’s vacuum pack technique length of hospital or ICU stay, development of ACS or requirement for decompressive laparotomy, acute renal failure, effect on IAP Mortality, length of hospital or ICU stay, acute renal failure, healthrelated quality of life Mortality, primary fascial closure, length of hospital and ICU stay, abdominal fistulae, intraabdominal infection, IAH, ACS observational studies RCTs, observational studies RCTs, observational studies 11) Whether to use bioprosthetic meshes Trauma or surgery patients with open abdominal wounds Bioprosthetic meshes No bioprosthetic meshes Where ACS indicates abdominal compartment syndrome; APP, abdominal perfusion pressure; IAH, intra-abdominal hypertension; IAP, intra-abdominal pressure; ICU, intensive care unit; KCI, Kinetic Concepts Incorporated; NPT, negative pressure therapy; NPWT, negative pressure wound therapy; PICOD, Patient, Intervention, Comparator, Outcome, Design; RCTs, randomized controlled trials; VAC, vacuum-assisted closure.