CriticalCareNursing - wikifun-usf
advertisement
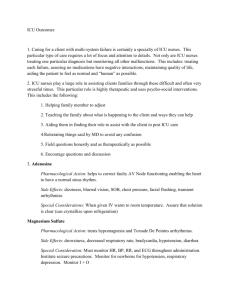
Critical Care Nursing Critically ill patients are defined as those patients who are at high risk for actual or potential life-threatening health problems. The more critically ill the patient is, the more likely he or she is to be highly vulnerable, unstable and complex, thereby requiring intense and vigilant nursing care. Protecting critically ill patients from harm by constant monitoring and prompt intervention is a primary responsibility of nurses in the intensive care unit (ICU). This concept goes back to Florence Nightingale, credited as the first to use an "ICU" by placing the sickest patients nearest the nursing station for closer monitoring.1 Today, the ICU is considered the safest place with the highest level of monitoring for critically ill patients.1–4 But what about when the patient leaves the ICU for diagnostic or therapeutic procedures? Transport of ICU patients out of the ICU for tests and procedures is a necessary part of critical care,5 but there is "considerable danger for the patient to leave the ICU."6 Transporting patients causes stress for many ICU nurses as they perceive the patient to be more vulnerable, while at the same time the resources available to the patient may be more limited.7 The standard for intra-hospital transport is to provide the same level of care, monitoring, and intervention as are available in the ICU.8–14 The goal of this article is to provide a workable, organized framework for safe intra-hospital transport of critical care patients. The target audience is ICU nurses who are required to transport their patients for test and procedures. The Behavior Pain Scale (BPS) has been tested among the broadest range of patients and was found to be a reliable and valid tool in three studies. Research is needed to further demonstrate the reliability and validity of the Critical-Care Pain Observation Tool (CPOT), as the paper of Gelinas et al. did not test its internal consistency and domain structure. The CPOT also needs testing among different critical care populations. The design of Odhner et al. study did not allow adequate testing of the Non-verbal Pain Scale (NVPS). The first consideration for intra-hospital transport is the potential benefit for the patient versus the potential risks to the patient. "Benefit" refers to a diagnostic test that alters management or to a therapeutic procedure that improves outcome.7 "Risk" refers to the potential danger to the patient, directly related to the patient’s level of stability. Red flags to consider when planning transport are noted in Table 5 . Benefit must outweigh risk, with the transport in the best interest of the patient. In a review of transport literature published in 1999, Waydhas et al reported a change in management in 40% to 50% of patients transported for diagnostic procedures, "indicating a good risk/benefit ratio." These older data are not supplemented by more recent studies because little recent research has been conducted. Critical care nurses practice in settings where patients require complex assessment, highintensity therapies and interventions, and continuous nursing vigilance. Critical care nurses rely upon a specialized body of knowledge, skills and experience to provide care to patients and families and create environments that are healing, humane and caring. Foremost, the critical care nurse is a patient advocate. AACN defines advocacy as respecting and supporting the basic values, rights and beliefs of the critically ill patient. In this role, critical care nurses: · Respect and support the right of the patient or the patient’s designated surrogate to autonomous informed decision making. · Intervene when the best interest of the patient is in question. · Help the patient obtain necessary care. · Respect the values, beliefs and rights of the patient. · Provide education and support to help the patient or the patient’s designated surrogate make decisions. · Represent the patient in accordance with the patient’s choices. · Support the decisions of the patient or designated surrogate, or transfer care to an equally qualified critical care nurse. · Intercede for patients who cannot speak for themselves in situations that require immediate action. · Monitor and safeguard the quality of care the patient receives. · Act as a liaison between the patient, the patient’s family and other healthcare professionals. Patients who respond well to treatment regimes are usually transferred out of the critical care unit to a stepdown, telemetry or medical-surgical unit for further recovery before being released from the hospital.