Supplemental Table 1 – OGM-Open Surgical Approach Author Year
advertisement

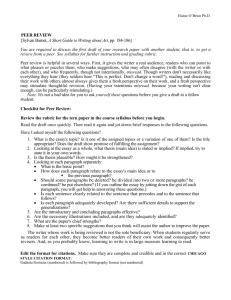
Supplemental Table 1 – OGM-Open Surgical Approach Perioperative Mortality CSF Leak Neurological Morbidity Visual Function Unchanged Year Visual Function Deteriorated Ojemann1 1991 17 – 5.9% – – – – – Apuzzo2 1993 33 – 6.1% – – – – – Schaller3 1994 28 96.4% 3.6% – 3.6% 21.4% – Mayfrank4 1996 18 100.0% 5.6% – – – Yasargil5 1996 91 – 0.0% – – DeMonte6 1996 17 94.1% 5.9% 5.9% 0.0% Turazzi7 1999 37 100.0% 2.7% – Tsikoudas8 1999 13 100.0% 15.4% 23.1% Paterniti9 1999 20 100.0% 10.0% El Gindi10 2000 25 – 0.0% Snyder11 2000 4 50.0% 0.0% Zevgaridis12 2001 5 100.0% Hallacq13 2001 6 Welge-Luessen14 2001 12 Tachikawa15 2002 Wei16 Hentschel17 Obeid18 Mean Follow-Up (Months) Recurrence / Progression Recurrence (/P-Y) – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – 100.0% 0.0% 0.0% 48 0.0% 0.00E+00 – 0.0% – – 7.7% 120 30.8% 3.08E-04 23.1% – – – – – 12-252 0.0% – – 4.0% 8.0% – – 12.0% – – – – – – 25.0% 75.0% 0.0% 24 25.0% 1.23E-03 100.0% 0.0% – – 80.0% 20.0% 0.0% 60 0.0% 0.00E+00 – 100.0% 0.0% 0.0% 0.0% 50.0% 50.0% 0.0% 12 – – 50.0% 100.0% 8.3% – – – – 24 – – 66.7% 1 100.0% 0.0% – – – – – – – – – 2002 1 100.0% 0.0% – – – – – – – – 0.0% 2003 13 84.6% 0.0% 0.0% 0.0% 83.3% 16.7% 0.0% 24 0.0% 0.00E+00 – 2003 15 86.7% 0.0% 20.0% 0.0% 60.0% 33.3% 6.7% 44 0.0% 0.00E+00 0.0% Spektor19 2005 80 90.0% 0.0% 12.5% 0.0% – – – 71 2.5% 4.24E-05 – Tuna20 2005 25 100.0% 0.0% 16.0% 0.0% 53.8% 38.5% 7.7% 58 0.0% 0.00E+00 – Klein21 2006 1 100.0% 0.0% 0.0% 0.0% – – – – – – – Nakamura22 2007 82 92.0% 4.9% 2.4% – 55.0% – – 63 4.9% 9.29E-05 – Bassiouni23 2007 56 100.0% 5.6% 5.4% 0.0% 83.3% 16.7% 0.0% 67 8.9% 1.59E-04 36.6% Colli24 2007 17 94.1% 11.8% – – – – – – – – – Gazzeri25 2008 36 86.1% 2.8% 5.6% 0.0% 25.0% 72.2% 2.8% 111 5.6% 6.01E-05 – Author Gross Total Resection Visual Function Improved No. of Patients – Post-Op Anosmia Romani26 2009 66 90.9% 0.0% 9.1% 19.7% 75.0% – 0.0% 45 6.1% 1.62E-04 18.2% Aguiar27 2009 21 100.0% 4.8% 23.8% – – – – 50 19.0% 4.57E-04 – Ali28 2009 1 – 0.0% – – 100.0% – – 5 – – – El-Bahy29 2009 18 77.8% 5.6% 16.7% – 80.0% 20.0% 0.0% 31 0.0% 0.00E+00 – Tomasello30 2011 18 94.4% 0.0% – – 53.8% 38.5% 7.7% 94 16.7% 2.14E-04 77.8% Telera31 2012 5 100.0% 0.0% 20.0% – 100.0% 0.0% 0.0% 34 20.0% 7.10E-04 – Supplemental Table 2 – OGM-Endoscopic Surgical Approach Visual Function Improved Visual Function Unchanged Visual Function Deteriorated Mean FollowUp (Months) Recurrence/ Progression Recurrence (/P-Y) Post-Op Anosmia Year No. of Patients Gross Total Resection Jho32 2001 1 100.0% 0.0% 0.0% 0.0% 100.0% 0.0% 0.0% 20 0.0% 0.0E+00 0.0% Jho33 2004 1 100.0% 0.0% 0.0% 0.0% 100.0% 0.0% 0.0% 12 0.0% 0.0E+00 0.0% Kassam34 WebbMyers35 2005 1 – 0.0% – 0.0% 100.0% 0.0% 0.0% 24 0.0% 0.0E+00 – 2007 1 100.0% 0.0% 100.0% – – – – – – – – Gardner36 2008 12 83.3% – 27.9% 8.3% 100.0% 0.0% 0.0% (12-48) 0.0% – – Author de Divitiis37 Perioperative Mortality CSF Leak Neurological Morbidity 2008 4 100.0% 0.0% 25.0% – 0.0% 0.0% 0.0% 10 0.0% 0.0E+00 – Greenfield38 2010 6 83.3% 0.0% 16.7% – – – – 39 16.7% 5.1E-04 – Liu39 2011 2 100.0% 0.0% 0.0% – – – – 12 0.0% 0.0E+00 – Kim40 2011 2 100.0% 0.0% 0.0% 0.0% – – – – – – 50.0% Supplemental Table 3 – TSM-Open Surgical Approach Visual Function Unchanged Visual Function Deteriorated 25.0% 72.0% 3.0% 78 8.7% 1.34E-04 10.3% 59.0% 23.0% 19.0% 78 0.0% 0.00E+00 – 3.4% 53.5% 27.5% 19.0% (12-96) 4.5% – 0.0% – – 50.0% 50.0% 0.0% 33 12.5% 4.62E-04 – – – 67.0% 23.0% 11.0% – – – 100.0% 1.0% – – 64.3% 25.9% 9.8% 120 0.0% 0.00E+00 69 91.3% 7.2% – – 54.2% 37.2% 8.4% 110 5.8% 6.33E-05 2000 21 100.0% 0.0% – 23.8% 52.4% 38.1% 9.5% 36 4.8% 1.60E-04 2001 24 96.0% – – 12.5% 54.2% 45.8% 0.0% 124 – – Ohta48 2001 33 63.6% 0.0% – – 42.9% 42.9% 14.3% 128 24.2% 2.27E-04 Ciric49 2001 24 71.0% 0.0% 0.0% 8.3% – – 4.1% 76 16.7% 2.63E-04 Fahlbusch50 2002 47 98.0% 0.0% – – 80.0% – 20.0% 52 2.1% 4.85E-05 Goel51 2002 70 84.0% 3.0% – – 70.0% 16.0% 10.0% 46 1.4% 3.65E-05 Jallo52 2002 23 87.0% 8.7% – 0.0% 55.0% 26.0% 19.0% 112 4.3% 4.61E-05 Chi53 2003 21 61.5% 0.0% – – 47.0% 42.0% 11.0% 3 – – Margalit54 2003 14 87.0% – – Spangenberg55 2004 17 94.1% 0.0% Wiedemayer56 2004 6 100.0% 0.0% Schick57 2005 53 90.6% Pamir58 2005 42 Bassiouni59 2006 62 Park60 Year No. of Patients Gross Total Resection Perioperative Mortality Al-Mefty41 1991 35 91.0% 8.6% – – Conforti42 1991 39 100.0% 7.7% – Gökalp43 1993 88 67.0% 18.2% Honegger44 1993 8 25.0% Ojemann45 1995 18 44.0% Yasargil5 1996 112 Raco46 1999 Arai47 Zevgaridis12 Author CSF Leak Neurological Morbidity Visual Function Improved Mean Follow-Up (Months) Recurrence / Progression Recurrence (/P-Y) – – – – – – – 23.5% 70.6% 23.5% 5.9% (12-136) 0.0% – 0.0% 0.0% 66.7% – – 11 0.0% 0.00E+00 3.7% – 9.4% 37.7% 47.2% 13.2% 30 3.7% 1.48E-04 69.0% 2.4% 9.5% 7.1% 59.5% 26.2% 14.3% 38 2.4% 7.68E-05 90.3% 0.0% – 16.1% 50.0% 35.3% 14.7% 72 3.2% 5.33E-05 2006 30 76.7% 0.0% – – 67.0% 3.3% 30.0% 76 13.3% 2.10E-04 61 Mathiesen 2006 29 89.6% 0.0% – 0.0% 91.0% 9.0% 0.0% 61 6.9% 1.35E-04 Nakamura62 2006 72 91.7% 2.8% 3.9% 2.6% 67.9% 19.6% 12.5% 45 2.8% 7.47E-05 Otani63 2006 32 87.5% 0.0% – 6.3% 78.1% 9.4% 12.5% 38 0.0% 0.00E+00 Czirjak64 2006 9 100.0% – – – – – – – – – Margalit65 2007 20 80.0% 0.0% – 0.0% 28.0% 58.0% 14.0% 3 0.0% 0.00E+00 Kitano66 2007 12 82.0% 0.0% 8.3% 8.3% 33.0% 33.0% 33.0% 24 3.6% 1.80E-04 Li67 2007 43 74.4% 2.3% – 2.4% 46.5% 34.8% 18.6% 65 4.7% 8.68E-05 Nozaki68 2008 20 70.0% 0.0% – – 50.0% 35.0% 15.0% 60 0.0% 0.00E+00 – de Divirtiis69 2008 44 86.4% 0.0% – 6.8% 61.4% 25.0% 13.6% (9-252) 11.4% Kim70 2008 27 74.1% 0.0% – 0.0% 44.4% 33.3% 22.2% 22 7.4% 4.04E-04 Sade71 2009 31 83.8% 0.0% – 3.2% 78.0% 22.0% 0.0% 33 0.0% 0.00E+00 Fatemi72 2009 5 80.0% 0.0% – 0.0% 63.0% 37.0% 11.0% 14 11.0% 9.43E-04 Ganna73 2009 24 87.5% 0.0% – 29.2% 79.0% 17.0% 4.0% 52 0.0% 0.00E+00 Galal74 2010 21 81.0% 4.8% – 0.0% 69.0% 40.0% 0.0% 28 0.0% 0.00E+00 Li-Hua75 2010 67 92.4% 0.0% – 13.4% 65.0% 29.0% 6.0% 29 3.0% 1.23E-04 Mahmoud76 2010 58 86.0% 1.7% – 10.4% 74.0% 18.0% 8.0% 23 1.7% 8.87E-05 Landeiro77 2010 23 82.6% 0.0% – 0.0% 69.5% 21.7% 8.7% 31 0.0% 0.00E+00 Bowers78 2011 22 91.0% 0.0% – 0.0% – – 0.0% – 0.0% – Chokyu79 2011 34 79.4% 0.0% 0.0% 2.9% 90.6% 9.4% 0.0% 96 8.1% 1.02E-04 Terasaka80 2011 9 100.0% 0.0% 11.1% 22.2% 88.9% 11.1% 0.0% 25 0.0% 0.00E+00 Telera31 2012 14 86.0% 7.0% – – 76.9% 7.7% 15.4% 49 14.3% 3.50E-04 Supplemental Table 4 – TSM-Endoscopic Surgical Approach Year No. of Patients Gross Total Resection Perioperative Mortality CSF Leak Neurological Morbidity Visual Function Improved Visual Function Unchanged Visual Function Deteriorated Mean Follow-Up (Months) Recurrence/ Progression Recurrence (/P-Y) PostOp DI Jho81 2001 9 77.8% 0.0% 6.0% 0.0% – – – (1-20) 0.0% – – Jho33 2004 1 100.0% 0.0% 0.0% 0.0% 100.0% 0.0% 0.0% 17 0.0% 0.00E+00 – Cook82 2004 3 100.0% 0.0% 0.0% 0.0% 100.0% 0.0% 0.0% 10 33.3% 4.00E-03 – Laufer83 2007 3 100.0% 0.0% 33.3% 0.0% 100.0% 0.0% 0.0% 9 0.0% 0.00E+00 33.3% de Divitiis84 2007 6 83.3% 16.7% 16.7% 0.0% 100.0% 0.0% 0.0% 3 – – 16.7% de Divitiis37 2008 7 85.7% 14.3% 28.6% 0.0% 100.0% 0.0% 0.0% – 0.0% – – Divitiis69 0.0% – – Author de 2008 7 83.3% 0.0% 28.6% 0.0% 71.4% 28.6% 0.0% (3-20) Gardner36 2008 13 85.0% 0.0% 61.5% 7.7% 100.0% 0.0% 0.0% 36 0.0% 0.00E+00 3.0% Fatemi72 2009 10 80.0% 0.0% 28.5% 0.0% 82.0% 9.0% 7.0% 32 14.3% 5.36E-04 – Wang85 2009 7 85.7% 0.0% 0.0% 0.0% 86.0% 14.0% 0.0% 23 0.0% 0.00E+00 14.3% Bowers78 2011 3 66.6% 0.0% 33.3% 0.0% – – 0.0% – 33.3% – – Van Gompel86 2011 13 53.8% 0.0% 0.0% 7.7% 66.7% 33.3% 0.0% 14 – – – Liu 2011 2 100.0% 0.0% 0.0% 0.0% 100.0% 0.0% 0.0% – – – – Chowdhury88 2012 6 83.3% 0.0% 16.7% 33.3% 83.3% 0.0% 16.7% 7 0.0% 0.00E+00 – 87 Supplemental Table 5 – CRA-Open Surgical Approach Year No. of Patients Gross Total Resection Perioperative Mortality Neurological Morbidity Visual Function Improved Colangelo89 1990 32 22.0% 12.0% Fischer90 1990 37 19.0% 0.0% – 12.0% – – – – – – Yasargil91 1990 144 90.0% Samii92 2.1% – – 28.3% 1991 34 Symon93 100.0% 0.0% – 0.0% – 1991 Hoffman94 1992 50 60.0% 4.0% – 10.9% – 50 90.0% 2.0% 6.0% 6.0% 36.0% Tomita95 Pierre-Kahn96 1993 27 78.0% 0.0% – – 80.0% Maira97 1994 30 83.0% 0.0% – – Mark98 1995 22 71.0% 0.0% 22.7% 1995 49 39.0% 10.0% – De Vile99 1996 75 40.0% 0.0% – Shibuya100 1996 22 – 0.0% Bulow101 1998 26 73.0% Fisher102 1998 30 27.0% Khafaga103 1998 44 Fahlbusch104 1999 Kim105 Author Ven Effenterre106 Mean Follow-Up (Months) Recurrence/ Progression – 55 14.0% 3.04E-04 – – – 126 57.0% 5.43E-04 34.0% – 18.3% 15.1% – 7.0% – 77.1% – – – – 3.0% – 80.0% – – – 30 10.0% 4.00E-04 50.0% 8.7% 23.0% 41.0% 59 29.0% 5.92E-04 93.0% 52.0% 1.0% 19.0% 80 14.0% 2.09E-04 81.0% – 31.0% 40.0% 29.0% 38 – – – – 4.5% – – – 90 0.0% 0.00E+00 – – 10.2% – – – 96 37.0% 4.63E-04 – – 13.0% – – – 77 10.0% 1.56E-04 80.0% 15.0% – 7.0% 72.0% 19.0% 9.0% 33 – – 97.0% – 8.0% – – – – – 150 – – – – 0.0% – – – – – – – – 83.0% – 39.0% 16.0% – – – – – 24 – – – – 148 73.0% 1.1% 18.9% 0.7% 36.7% 14.4% 12.2% 65 5.4% 9.98E-05 – 1.4% 2001 36 100.0% 0.0% – 42.0% – – 25.0% 52 39.0% 9.07E-04 94.0% 6.0% CSF Leak Visual Function Unchanged Visual Function Deteriorated Recurrence (/P-Y) PostOp DI Obesity/ Hyperphagia 2002 122 79.0% 2.5% 0.8% 8.0% 70.0% 19.0% 11.0% 84 13.0% 1.86E-04 57.0% 36.0% Chen107 2003 36 19.0% 5.6% – 14.0% 50.0% 19.0% 31.0% 123 – – 67.0% – Kalapurakal108 2003 25 76.0% 0.0% – – – – – 120 32.0% 3.20E-04 100.0% 32.0% Gonc109 2004 66 33.0% 2.0% – 10.6% – – – 61 41.0% 8.04E-04 52.0% – Stripp110 2004 76 62.0% 1.0% – – 21.0% 64.0% 15.0% 91 – – 80.0% 49.0% Albright111 2005 27 67.0% 0.0% – 11.0% – – 19.0% 108 11.0% 1.22E-04 – – Ersahin112 2005 87 43.0% 7.0% 1.1% 15.0% – – 5.0% 38 5.0% 1.56E-04 33.0% – Karavitaki113 2005 121 15.7% 1.8% 6.5% 9.7% – – 6.5% 103 15.6% 1.82E-04 65.0% 39.0% Lena114 2005 47 66.0% 2.4% – – 16.0% 68.0% 16.0% 114 26.0% 2.74E-04 86.0% 48.0% Minamida115 2005 37 70.0% 0.0% – 2.7% – – 2.7% 133 15.0% 1.35E-04 – – Mottolese116 2005 36 74.0% 6.0% – – – – 14.0% – 16.0% – 100.0% – Sainte-Rose117 2005 66 50.0% – – – 68.0% 11.0% 21.0% 84 36.0% 5.14E-04 – 70.0% Shirane118 2005 42 71.0% 0.0% – 6.7% – – – – 20.0% – – – Sosa119 2005 35 83.0% 0.0% – 20.0% – – 17.0% 55 41.0% 8.91E-04 91.0% – Thompson120 2005 48 33.0% 0.0% – 15.0% 61.0% – – 67 50.0% 8.93E-04 84.0% 20.0% Tomita121 2005 54 61.0% 0.0% 1.9% 9.0% 43.0% 44.0% 13.0% – 27.0% – 87.0% 28.0% Zuccaro122 2005 153 69.0% 3.0% – 10.0% 45.0% 46.5% 8.5% – 0.0% – 50.0% 35.0% Xu123 2005 51 92.0% 0.0% – 8.0% – – – 28 17.0% 7.39E-04 – – Dhellemmes124 2006 37 65.0% 0.0% – 8.0% 7.0% 69.0% 24.0% 121 43.0% 4.26E-04 – 48.0% Rocco125 Di 2006 54 78.0% 3.7% – 18.0% 44.0% 45.0% 11.0% 104 7.0% 8.05E-05 56.0% 18.0% Gupta126 2006 72 26.0% – – – – – – 18 11.0% 7.33E-04 – – Hafez127 2006 62 50.0% 6.0% – 6.0% 68.0% 27.0% 5.0% 42 20.0% 5.71E-04 85.0% – Ohmori Puget (retrospective)128 Puget (prospective)128 2007 27 93.0% 3.7% – – – – – – 14.0% – – – 2007 66 50.0% 1.5% – 6.0% 68.0% 11.0% 21.0% 84 36.0% 5.14E-04 94.0% 70.0% 2007 22 23.0% 0.0% 4.5% 14.0% – – 4.5% 14 0.0% 0.00E+00 100.0% 27.0% Lee129 2008 66 – 0.0% – 6.0% – – – 86 – – 66.7% 18.0% Shi130 2008 309 89.0% 3.9% – 6.0% 42.0% 52.5% 5.5% 25 14.0% 6.67E-04 53.0% – Zhang131 2008 202 40.0% 1.0% – 5.4% 42.0% 53.0% 5.0% – 0.0% – 81.0% 22.0% Kawamata132 2010 55 22.0% 0.0% – – – – 33.0% 178 – – 45.0% – Elliott133 2011 57 100.0% 3.5% – 12.0% 56.5% 18.5% 25.0% 128 20.0% 1.87E-04 78.0% 15.0% Supplemental Table 6 – CRA-Endoscopic Surgical Approach Author Year No. of Patients Gross Total Resection Perioperative Mortality CSF Leak Neurological Morbidity Visual Function Improved Visual Function Unchanged Visual Function Deteriorated Mean Follow-Up (Months) Recurrence/ Progression Recurrence (/P-Y) PostOp DI New Obesity/ Hyperphagia Jho134 1997 1 100.0% 0.0% 100.0% – – – – – – – 100.0% – Frank135 2006 10 70.0% 0.0% 30.0% 0.0% 75.0% 25.0% 0.0% 37.2 0.0% 0.00E+00 30.0% 20.0% de Divitiis136 2007 6 83.3% 16.7% 16.7% 16.7% 75.0% 25.0% 0.0% – – – 50.0% – Laufer83 2007 4 – 0.0% 0.0% 100.0% 100.0% 0.0% 0.0% 8.5 – – 100.0% 0.0% Cappabianca137 2008 6 66.7% 0.0% 16.7% 16.7% 75.0% 0.0% 25.0% – – – 16.7% – Cavallo138 2008 18 72.2% 0.0% 55.6% 46.2% 92.3% – 5.6% 38.5 11.1% 3.46E-04 11.1% – Gardner139 2008 11 63.6% 0.0% 81.8% 18.2% 88.9% 11.1% 0.0% 37.6 18.2% 5.80E-04 9.1% 0.0% Stamm140 2008 7 57.1% 0.0% 28.6% 0.0% 66.7% – – 36.2 0.0% 0.00E+00 57.1% – Fatemi72 2009 12 16.7% 0.0% 6.0% 0.0% 92.0% 8.0% 0.0% 20.4 0.0% 0.00E+00 46.0% – Ceylan141 2009 2 100.0% 0.0% – – – – – 25.5 – – 0.0% – Dehdashti142 2009 4 25.0% 0.0% 25.0% 25.0% 100.0% 0.0% 0.0% 14.0 – – 0.0% – Campbell143 2010 14 28.6% 0.0% 35.7% 7.1% 85.7% 7.1% 7.1% 3.0 7.1% 2.86E-03 7.1% 0.0% Jane144 2010 9 100.0% 0.0% 0.0% 66.7% 100.0% 0.0% 0.0% 13.3 11.1% 1.00E-03 55.6% – Supplemental Table 7 – CHO-Open Surgical Approach CSF Leak Neurological Morbidity Visual Function Unchanged Mean Follow-Up (Months) Recurrence / Progression Recurrence (/P-Y) – 47 – – – 16.7% – – – – – 65 9.3% 1.72E-04 Year Gross Total Resection Gay145 1995 46 47.0% 5.0% 30.0% 76.1% 52.0% 48.0% Goel146 1995 6 50.0% 0.0% 0.0% 0.0% – Carrabba147 2008 43 84.0% 2.3% – 30.2% – Author Perioperative Mortality Visual Function Improved No. of Patients Visual Function Deteriorated Supplemental Table 8 – CHO-Endoscopic Surgical Approach Gross Total Resection Perioperative Mortality Neurological Morbidity Visual Function Unchanged Visual Function Deteriorated Mean FollowUp (Months) Recurrence/ Progression Recurrence (/P-Y) Year No. of Patients Jho134 1997 1 0.0% 0.0% 0.0% – – – – – – – Miyagi148 1998 1 100.0% – – – – – – – – – Jho81 2001 7 71.4% 0.0% 6.0% 0.0% – – – (1-20) 0.0% – 33.3% 66.7% 0.0% 33.3% 25 33.3% 1.62E-03 – – – 15 33.3% 2.73E-03 Author 149 Jho CSF Leak Visual Function Improved 2004 3 100.0% 0.0% 33.3% 150 2005 3 – 0.0% 0.0% 151 Rudnik 2005 1 0.0% 0.0% 0.0% – – – – – – – Frank152 2006 5 40.0% 20.0% 0.0% 0.0% 75.0% 25.0% 0.0% 22 0.0% 0.00E+00 Hwang153 2007 3 0.0% 0.0% 0.0% 33.3% 0.0% 66.7% 33.3% 35 0.0% 0.00E+00 2007 1 0.0% 0.0% 0.0% – – – – – – – Dehdashti 2008 12 58.0% 0.0% 33.3% 16.7% 66.7% 33.3% 0.0% 16 0.0% 0.00E+00 Zhang156 2008 7 85.7% 0.0% – 0.0% 100.0% 0.0% 0.0% 21 14.3% 8.01E-04 2008 17 59.0% 0.0% 24.0% 5.9% 75.0% 25.0% 0.0% 16 0.0% 0.00E+00 100.0% 0.0% 8.3% 21 16.7% 9.52E-04 Solares Pirris 154 155 147 Carrabba Hong Jiang157 2009 12 58.3% 0.0% – 8.3% Stippler158 2009 20 45.0% 5.0% 5.0% 5.0% – – – 13 10.0% 9.23E-04 Fraser159 2010 7 71.4% 0.0% 0.0% 0.0% 100.0% 0.0% 0.0% 18 14.3% 9.52E-04 Fraser160 2010 8 50.0% 12.5% 50.0% 0.0% 66.7% 33.3% 0.0% 12 0.0% 0.00E+00 Alexander161 2010 1 0.0% 0.0% 100.0% 0.0% 100.0% 0.0% 0.0% 14 0.0% 0.00E+00 Holzmann162 2010 13 84.6% 0.0% 7.7% – – – – 18 0.0% 0.00E+00 References 1 Ojemann, R. Meningiomas. Neurosurgery clinics of North America 1, 181-197 (1990). 2 Apuzzo, M. L. J. Brain surgery : complication avoidance and management. (Churchill Livingstone, 1993). 3 Schaller, C., Rohde, V. & Hassler, W. Microsurgical Removal of Olfactory Groove Meningiomas via the Pterional Approach. Skull base surgery 4, 189-192 (1994). 4 Mayfrank, L. & Gilsbach, J. M. Interhemispheric approach for microsurgical removal of olfactory groove meningiomas. British journal of neurosurgery 10, 541-545 (1996). 5 Yaşargil, M. G., Curcic, M. & Abernathey, C. D. Microneurosurgery of CNS tumor. (Georg Thieme Verlag ; Thieme Medical Publishers, 1994). 6 DeMonte, F. Surgical treatment of anterior basal meningiomas. Journal of neuro-oncology 29, 239-248 (1996). 7 Turazzi, S., Cristofori, L., Gambin, R. & Bricolo, A. The pterional approach for the microsurgical removal of olfactory groove meningiomas. Neurosurgery 45, 821-825; discussion 825-826 (1999). 8 Tsikoudas, A. & Martin-Hirsch, D. P. Olfactory groove meningiomas. Clinical otolaryngology and allied sciences 24, 507509 (1999). 9 Paterniti, S., Fiore, P., Levita, A., La Camera, A. & Cambria, S. Venous saving in olfactory meningioma's surgery. Clinical neurology and neurosurgery 101, 235-237 (1999). 10 El Gindi, S. Olfactory groove meningioma: surgical techniques and pitfalls. Surgical neurology 54, 415-417 (2000). 11 Snyder, W. E., Shah, M. V., Weisberger, E. C. & Campbell, R. L. Presentation and patterns of late recurrence of olfactory groove meningiomas. Skull base surgery 10, 131-139 (2000). 12 Zevgaridis, D., Medele, R. J., Muller, A., Hischa, A. C. & Steiger, H. J. Meningiomas of the sellar region presenting with visual impairment: impact of various prognostic factors on surgical outcome in 62 patients. Acta neurochirurgica 143, 471-476 (2001). 13 Hallacq, P., Moreau, J. J., Fischer, G. & Beziat, J. L. Trans-sinusal frontal approach for olfactory groove meningiomas. Skull base : official journal of North American Skull Base Society ... [et al.] 11, 35-46 (2001). 14 Welge-Luessen, A. et al. Olfactory function in patients with olfactory groove meningioma. Journal of neurology, neurosurgery, and psychiatry 70, 218-221 (2001). 15 Tachikawa, T., Adachi, J., Nishikawa, R. & Matsutani, M. An anterior ethmoidal artery aneurysm associated with an olfactory groove meningioma. Case illustration. Journal of neurosurgery 97, 1479, doi:10.3171/jns.2002.97.6.1479 (2002). 16 17 18 19 20 21 22 23 24 25 26 27 28 29 Wei, C. P., Wang, A. D. & Tsai, M. D. Resection of giant olfactory groove meningioma with extradural devascularization. Skull base : official journal of North American Skull Base Society ... [et al.] 12, 27-31 (2002). Hentschel, S. J. & DeMonte, F. Olfactory groove meningiomas. Neurosurgical focus 14, e4 (2003). Obeid, F. & Al-Mefty, O. Recurrence of olfactory groove meningiomas. Neurosurgery 53, 534-542; discussion 542-533 (2003). Spektor, S. et al. Olfactory groove meningiomas from neurosurgical and ear, nose, and throat perspectives: approaches, techniques, and outcomes. Neurosurgery 57, 268-280; discussion 268-280 (2005). Tuna, H., Bozkurt, M., Ayten, M., Erdogan, A. & Deda, H. Olfactory groove meningiomas. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia 12, 664-668, doi:10.1016/j.jocn.2005.05.002 (2005). Klein, O., Freppel, S., Auque, J. & Civit, T. Cavernous angioma within an olfactory groove meningioma. Case report. Journal of neurosurgery 104, 325-328, doi:10.3171/jns.2006.104.2.325 (2006). Nakamura, M., Struck, M., Roser, F., Vorkapic, P. & Samii, M. Olfactory groove meningiomas: clinical outcome and recurrence rates after tumor removal through the frontolateral and bifrontal approach. Neurosurgery 60, 844-852; discussion 844-852, doi:10.1227/01.NEU.0000255453.20602.80 (2007). Bassiouni, H., Asgari, S. & Stolke, D. Olfactory groove meningiomas: functional outcome in a series treated microsurgically. Acta neurochirurgica 149, 109-121; discussion 121, doi:10.1007/s00701-006-1075-z (2007). Colli, B. O. et al. Olfactory groove meningiomas: surgical technique and follow-up review. Arquivos de neuro-psiquiatria 65, 795-799 (2007). Gazzeri, R., Galarza, M. & Gazzeri, G. Giant olfactory groove meningioma: ophthalmological and cognitive outcome after bifrontal microsurgical approach. Acta neurochirurgica 150, 1117-1125; discussion 1126, doi:10.1007/s00701-0080142-z (2008). Romani, R. et al. Lateral supraorbital approach applied to olfactory groove meningiomas: experience with 66 consecutive patients. Neurosurgery 65, 39-52; discussion 52-33, doi:10.1227/01.NEU.0000346266.69493.88 (2009). Aguiar, P. H. et al. Olfactory groove meningiomas: approaches and complications. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia 16, 1168-1173, doi:10.1016/j.jocn.2008.12.013 (2009). Ali, N., Akunjee, M. & Ahfat, F. Acute and severe visual loss due to an olfactory groove meningioma. Canadian journal of ophthalmology. Journal canadien d'ophtalmologie 44, e49-50, doi:10.3129/i09-165 (2009). El-Bahy, K. Validity of the frontolateral approach as a minimally invasive corridor for olfactory groove meningiomas. Acta neurochirurgica 151, 1197-1205, doi:10.1007/s00701-009-0369-3 (2009). 30 31 32 33 34 35 36 37 38 39 40 41 42 43 Tomasello, F. et al. Giant olfactory groove meningiomas: extent of frontal lobes damage and long-term outcome after the pterional approach. World neurosurgery 76, 311-317; discussion 255-318, doi:10.1016/j.wneu.2011.03.021 (2011). Telera, S. et al. Supraorbital keyhole approach for removal of midline anterior cranial fossa meningiomas: a series of 20 consecutive cases. Neurosurgical review 35, 67-83; discussion 83, doi:10.1007/s10143-011-0340-7 (2012). Jho, H. D. Endoscopic endonasal approach to the optic nerve: a technical note. Minimally invasive neurosurgery : MIN 44, 190-193, doi:10.1055/s-2001-19927 (2001). Jho, H. D. & Ha, H. G. Endoscopic endonasal skull base surgery: Part 1--The midline anterior fossa skull base. Minimally invasive neurosurgery : MIN 47, 1-8, doi:10.1055/s-2003-812538 (2004). Kassam, A., Snyderman, C. H., Mintz, A., Gardner, P. & Carrau, R. L. Expanded endonasal approach: the rostrocaudal axis. Part I. Crista galli to the sella turcica. Neurosurgical focus 19, E3 (2005). Webb-Myers, R., Wormald, P. J. & Brophy, B. An endoscopic endonasal technique for resection of olfactory groove meningioma. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia 15, 451-455, doi:10.1016/j.jocn.2007.05.017 (2008). Gardner, P. A. et al. Endoscopic endonasal resection of anterior cranial base meningiomas. Neurosurgery 63, 36-52; discussion 52-34, doi:10.1227/01.NEU.0000335069.30319.1E (2008). de Divitiis, E. et al. Endoscopic transnasal resection of anterior cranial fossa meningiomas. Neurosurgical focus 25, E8, doi:10.3171/FOC.2008.25.12.E8 (2008). Greenfield, J. P. et al. Endoscopic endonasal transethmoidal transcribriform transfovea ethmoidalis approach to the anterior cranial fossa and skull base. Neurosurgery 66, 883-892; discussion 892 (2010). Liu, J. K., Christiano, L. D., Patel, S. K., Tubbs, R. S. & Eloy, J. A. Surgical nuances for removal of olfactory groove meningiomas using the endoscopic endonasal transcribriform approach. Neurosurgical focus 30, E3, doi:10.3171/2011.2.FOCUS116 (2011). Kim, Y. H., Han, D. H., Park, C. K., Lee, C. H. & Kim, D. G. An endoscopic endonsal transethmoidal approach to olfactory groove meningioma. Central European neurosurgery 72, 205-208, doi:http://dx.doi.org/10.1055/s-0031-1291179 10.1055/s-0031-1291179 (2011). Al-Mefty, O., DeMonte, F. & McDermott, M. W. Al-Mefty's Meningiomas. 1st edn, (Thieme Medical, 1991). Conforti, P., Moraci, A., Albanese, V., Rotondo, M. & Parlato, C. Microsurgical management of suprasellar and intraventricular meningiomas. Neurochirurgia 34, 85-89, doi:10.1055/s-2008-1052061 (1991). Gokalp, H. Z., Arasil, E., Kanpolat, Y. & Balim, T. Meningiomas of the tuberculum sella. Neurosurgical review 16, 111-114 (1993). 44 45 46 47 48 49 50 51 52 53 54 55 56 57 Honegger, J., Fahlbusch, R., Buchfelder, M., Huk, W. J. & Thierauf, P. The role of transsphenoidal microsurgery in the management of sellar and parasellar meningioma. Surgical neurology 39, 18-24 (1993). Ojemann, R. G., Thornton, A. F. & Harsh, G. R. Management of anterior cranial base and cavernous sinus neoplasms with conservative surgery alone or in combination with fractionated photon or stereotactic proton radiotherapy. Clinical neurosurgery 42, 71-98 (1995). Raco, A., Bristot, R., Domenicucci, M. & Cantore, G. Meningiomas of the tuberculum sellae. Our experience in 69 cases surgically treated between 1973 and 1993. Journal of neurosurgical sciences 43, 253-260; discussion 260-252 (1999). Arai, H. et al. Transcranial transsphenoidal approach for tuberculum sellae meningiomas. Acta neurochirurgica 142, 751-756; discussion 756-757 (2000). Ohta, K., Yasuo, K., Morikawa, M., Nagashima, T. & Tamaki, N. Treatment of tuberculum sellae meningiomas:a long-term follow-up study. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia 8 Suppl 1, 26-31, doi:10.1054/jocn.2001.0873 (2001). Ciric, I. & Rosenblatt, S. Suprasellar meningiomas. Neurosurgery 49, 1372-1377 (2001). Fahlbusch, R. & Schott, W. Pterional surgery of meningiomas of the tuberculum sellae and planum sphenoidale: surgical results with special consideration of ophthalmological and endocrinological outcomes. Journal of neurosurgery 96, 235243, doi:10.3171/jns.2002.96.2.0235 (2002). Goel, A., Muzumdar, D. & Desai, K. I. Tuberculum sellae meningioma: a report on management on the basis of a surgical experience with 70 patients. Neurosurgery 51, 1358-1363; discussion 1363-1354 (2002). Jallo, G. I. & Benjamin, V. Tuberculum sellae meningiomas: microsurgical anatomy and surgical technique. Neurosurgery 51, 1432-1439; discussion 1439-1440 (2002). Chi, J. H. & McDermott, M. W. Tuberculum sellae meningiomas. Neurosurgical focus 14, e6 (2003). Margalit, N. S., Lesser, J. B., Moche, J. & Sen, C. Meningiomas involving the optic nerve: technical aspects and outcomes for a series of 50 patients. Neurosurgery 53, 523-532; discussion 532-523 (2003). Spangenberg P, R. V., Mayfrank L, Gilsbach JM. Microsurgery of tuberculum sellae meningiomas. International Congress Series, 71-74 (2004). Wiedemayer, H., Sandalcioglu, I. E., Wiedemayer, H. & Stolke, D. The supraorbital keyhole approach via an eyebrow incision for resection of tumors around the sella and the anterior skull base. Minimally invasive neurosurgery : MIN 47, 221-225, doi:10.1055/s-2004-818526 (2004). Schick, U. & Hassler, W. Surgical management of tuberculum sellae meningiomas: involvement of the optic canal and visual outcome. Journal of neurology, neurosurgery, and psychiatry 76, 977-983, doi:10.1136/jnnp.2004.039974 (2005). 58 59 60 61 62 63 64 65 66 67 68 69 Pamir, M. N., Ozduman, K., Belirgen, M., Kilic, T. & Ozek, M. M. Outcome determinants of pterional surgery for tuberculum sellae meningiomas. Acta neurochirurgica 147, 1121-1130; discussion 1130, doi:10.1007/s00701-0050625-0 (2005). Bassiouni, H., Asgari, S. & Stolke, D. Tuberculum sellae meningiomas: functional outcome in a consecutive series treated microsurgically. Surgical neurology 66, 37-44; discussion 44-35, doi:10.1016/j.surneu.2005.11.059 (2006). Park, C. K. et al. Surgically treated tuberculum sellae and diaphragm sellae meningiomas: the importance of short-term visual outcome. Neurosurgery 59, 238-243; discussion 238-243, doi:10.1227/01.NEU.0000223341.08402.C5 (2006). Mathiesen, T. & Kihlstrom, L. Visual outcome of tuberculum sellae meningiomas after extradural optic nerve decompression. Neurosurgery 59, 570-576; discussion 570-576, doi:10.1227/01.NEU.0000228683.79123.F9 (2006). Nakamura, M., Roser, F., Struck, M., Vorkapic, P. & Samii, M. Tuberculum sellae meningiomas: clinical outcome considering different surgical approaches. Neurosurgery 59, 1019-1028; discussion 1028-1019, doi:10.1227/01.NEU.0000245600.92322.06 (2006). Otani, N. et al. Surgical management of tuberculum sellae meningioma: role of selective extradural anterior clinoidectomy. British journal of neurosurgery 20, 129-138, doi:10.1080/02688690600776747 (2006). Czirjak, S. & Szeifert, G. T. The role of the superciliary approach in the surgical management of intracranial neoplasms. Neurological research 28, 131-137, doi:10.1179/016164106X97991 (2006). Margalit, N., Kesler, A., Ezer, H., Freedman, S. & Ram, Z. Tuberculum and diaphragma sella meningioma--surgical technique and visual outcome in a series of 20 cases operated over a 2.5-year period. Acta neurochirurgica 149, 11991204; discussion 1204, doi:10.1007/s00701-007-1280-4 (2007). Kitano, M., Taneda, M. & Nakao, Y. Postoperative improvement in visual function in patients with tuberculum sellae meningiomas: results of the extended transsphenoidal and transcranial approaches. Journal of neurosurgery 107, 337346, doi:10.3171/JNS-07/08/0337 (2007). Li, X., Liu, M., Liu, Y. & Zhu, S. Surgical management of Tuberculum sellae meningiomas. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia 14, 1150-1154, doi:10.1016/j.jocn.2006.09.003 (2007). Nozaki, K. et al. Effect of early optic canal unroofing on the outcome of visual functions in surgery for meningiomas of the tuberculum sellae and planum sphenoidale. Neurosurgery 62, 839-844; discussion 844-836, doi:10.1227/01.neu.0000318169.75095.cb (2008). de Divitiis, E., Esposito, F., Cappabianca, P., Cavallo, L. M. & de Divitiis, O. Tuberculum sellae meningiomas: high route or low route? A series of 51 consecutive cases. Neurosurgery 62, 556-563; discussion 556-563, doi:10.1227/01.neu.0000317303.93460.24 (2008). 70 71 72 73 74 75 76 77 78 79 80 81 Kim, T. W. et al. Prognostic factors of postoperative visual outcomes in tuberculum sellae meningioma. British journal of neurosurgery 22, 231-234, doi:10.1080/02688690701772405 (2008). Sade, B. & Lee, J. H. High incidence of optic canal involvement in tuberculum sellae meningiomas: rationale for aggressive skull base approach. Surgical neurology 72, 118-123; discussion 123, doi:10.1016/j.surneu.2008.08.007 (2009). Fatemi, N., Dusick, J. R., de Paiva Neto, M. A., Malkasian, D. & Kelly, D. F. Endonasal versus supraorbital keyhole removal of craniopharyngiomas and tuberculum sellae meningiomas. Neurosurgery 64, 269-284; discussion 284-266, doi:10.1227/01.NEU.0000327857.22221.53 (2009). Ganna, A., Dehdashti, A. R., Karabatsou, K. & Gentili, F. Fronto-basal interhemispheric approach for tuberculum sellae meningiomas; long-term visual outcome. British journal of neurosurgery 23, 422-430, doi:10.1080/02688690902968836 (2009). Galal, A. et al. Determinants of postoperative visual recovery in suprasellar meningiomas. Acta neurochirurgica 152, 6977, doi:10.1007/s00701-009-0492-1 (2010). Li-Hua, C., Ling, C. & Li-Xu, L. Microsurgical management of tuberculum sellae meningiomas by the frontolateral approach: surgical technique and visual outcome. Clinical neurology and neurosurgery 113, 39-47, doi:10.1016/j.clineuro.2010.08.019 (2011). Mahmoud, M., Nader, R. & Al-Mefty, O. Optic canal involvement in tuberculum sellae meningiomas: influence on approach, recurrence, and visual recovery. Neurosurgery 67, ons108-118; discussion ons118-109, doi:10.1227/01.NEU.0000383153.75695.24 (2010). Landeiro, J. A. et al. Tuberculum sellae meningiomas: surgical considerations. Arquivos de neuro-psiquiatria 68, 424-429 (2010). Bowers, C. A., Altay, T. & Couldwell, W. T. Surgical decision-making strategies in tuberculum sellae meningioma resection. Neurosurgical focus 30, E1, doi:10.3171/2011.2.FOCUS1115 (2011). Chokyu, I., Goto, T., Ishibashi, K., Nagata, T. & Ohata, K. Bilateral subfrontal approach for tuberculum sellae meningiomas in long-term postoperative visual outcome. Journal of neurosurgery 115, 802-810, doi:10.3171/2011.5.JNS101812 (2011). Terasaka, S., Asaoka, K., Kobayashi, H. & Yamaguchi, S. Anterior interhemispheric approach for tuberculum sellae meningioma. Neurosurgery 68, 84-88; discussion 88-89, doi:10.1227/NEU.0b013e31820781e1 (2011). Jho, H. D. Endoscopic transsphenoidal surgery. Journal of neuro-oncology 54, 187-195 (2001). 82 83 84 85 86 87 88 89 90 91 92 93 Cook, S. W., Smith, Z. & Kelly, D. F. Endonasal transsphenoidal removal of tuberculum sellae meningiomas: technical note. Neurosurgery 55, 239-244; discussion 244-236 (2004). Laufer, I., Anand, V. K. & Schwartz, T. H. Endoscopic, endonasal extended transsphenoidal, transplanum transtuberculum approach for resection of suprasellar lesions. Journal of neurosurgery 106, 400-406, doi:10.3171/jns.2007.106.3.400 (2007). de Divitiis, E., Cavallo, L. M., Esposito, F., Stella, L. & Messina, A. Extended endoscopic transsphenoidal approach for tuberculum sellae meningiomas. Neurosurgery 61, 229-237; discussion 237-228, doi:10.1227/01.neu.0000303221.63016.f2 (2007). Wang, Q., Lu, X. J., Li, B., Ji, W. Y. & Chen, K. L. Extended endoscopic endonasal transsphenoidal removal of tuberculum sellae meningiomas: a preliminary report. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia 16, 889-893, doi:10.1016/j.jocn.2008.10.003 (2009). Van Gompel, J. J. et al. Expanded endonasal endoscopic resection of anterior fossa meningiomas: report of 13 cases and meta-analysis of the literature. Neurosurgical focus 30, E15, doi:10.3171/2011.1.FOCUS118 (2011). Liu, J. K., Christiano, L. D., Patel, S. K., Tubbs, R. S. & Eloy, J. A. Surgical nuances for removal of tuberculum sellae meningiomas with optic canal involvement using the endoscopic endonasal extended transsphenoidal transplanum transtuberculum approach. Neurosurgical focus 30, E2, doi:10.3171/2011.3.FOCUS115 (2011). Chowdhury, F. H., Haque, M. R., Goel, A. H. & Kawsar, K. A. Endoscopic endonasal extended transsphenoidal removal of tuberculum sellae meningioma (TSM): an experience of six cases. British journal of neurosurgery 26, 692-699, doi:10.3109/02688697.2012.673648 (2012). Colangelo, M., Ambrosio, A. & Ambrosio, C. Neurological and behavioral sequelae following different approaches to craniopharyngioma. Long-term follow-up review and therapeutic guidelines. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery 6, 379-382 (1990). Fischer, E. G., Welch, K., Shillito, J., Jr., Winston, K. R. & Tarbell, N. J. Craniopharyngiomas in children. Long-term effects of conservative surgical procedures combined with radiation therapy. Journal of neurosurgery 73, 534-540, doi:10.3171/jns.1990.73.4.0534 (1990). Yasargil, M. G. et al. Total removal of craniopharyngiomas. Approaches and long-term results in 144 patients. Journal of neurosurgery 73, 3-11, doi:10.3171/jns.1990.73.1.0003 (1990). Samii, M. & Bini, W. Surgical treatment of craniopharyngiomas. Zentralblatt fur Neurochirurgie 52, 17-23 (1991). Symon, L., Pell, M. F. & Habib, A. H. Radical excision of craniopharyngioma by the temporal route: a review of 50 patients. British journal of neurosurgery 5, 539-549 (1991). 94 95 96 97 98 99 100 101 102 103 104 105 106 107 Hoffman, H. J. et al. Aggressive surgical management of craniopharyngiomas in children. Journal of neurosurgery 76, 4752, doi:10.3171/jns.1992.76.1.0047 (1992). Tomita, T. & McLone, D. G. Radical resections of childhood craniopharyngiomas. Pediatric neurosurgery 19, 6-14 (1993). Pierre-Kahn, A., Sainte-Rose, C. & Renier, D. Surgical approach to children with craniopharyngiomas and severely impaired vision: special considerations. Pediatric neurosurgery 21 Suppl 1, 50-56 (1994). Maira, G., Anile, C., Rossi, G. F. & Colosimo, C. Surgical treatment of craniopharyngiomas: an evaluation of the transsphenoidal and pterional approaches. Neurosurgery 36, 715-724 (1995). Mark, R. J. et al. Craniopharyngioma: treatment in the CT and MR imaging era. Radiology 197, 195-198 (1995). De Vile, C. J. et al. Management of childhood craniopharyngioma: can the morbidity of radical surgery be predicted? Journal of neurosurgery 85, 73-81, doi:10.3171/jns.1996.85.1.0073 (1996). Shibuya, M., Takayasu, M., Suzuki, Y., Saito, K. & Sugita, K. Bifrontal basal interhemispheric approach to craniopharyngioma resection with or without division of the anterior communicating artery. Journal of neurosurgery 84, 951-956, doi:10.3171/jns.1996.84.6.0951 (1996). Bulow, B. et al. Postoperative prognosis in craniopharyngioma with respect to cardiovascular mortality, survival, and tumor recurrence. The Journal of clinical endocrinology and metabolism 83, 3897-3904 (1998). Fisher, P. G. et al. Outcomes and failure patterns in childhood craniopharyngiomas. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery 14, 558-563 (1998). Khafaga, Y. et al. Craniopharyngioma in children. International journal of radiation oncology, biology, physics 42, 601606 (1998). Fahlbusch, R., Honegger, J., Paulus, W., Huk, W. & Buchfelder, M. Surgical treatment of craniopharyngiomas: experience with 168 patients. Journal of neurosurgery 90, 237-250, doi:10.3171/jns.1999.90.2.0237 (1999). Kim, S. K. et al. Radical excision of pediatric craniopharyngioma: recurrence pattern and prognostic factors. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery 17, 531-536; discussion 537 (2001). Van Effenterre, R. & Boch, A. L. Craniopharyngioma in adults and children: a study of 122 surgical cases. Journal of neurosurgery 97, 3-11, doi:10.3171/jns.2002.97.1.0003 (2002). Chen, C., Okera, S., Davies, P. E., Selva, D. & Crompton, J. L. Craniopharyngioma: a review of long-term visual outcome. Clinical & experimental ophthalmology 31, 220-228 (2003). 108 109 110 111 112 113 114 115 116 117 118 Kalapurakal, J. A., Goldman, S., Hsieh, Y. C., Tomita, T. & Marymont, M. H. Clinical outcome in children with craniopharyngioma treated with primary surgery and radiotherapy deferred until relapse. Medical and pediatric oncology 40, 214-218, doi:10.1002/mpo.10247 (2003). Gonc, E. N., Yordam, N., Ozon, A., Alikasifoglu, A. & Kandemir, N. Endocrinological outcome of different treatment options in children with craniopharyngioma: a retrospective analysis of 66 cases. Pediatric neurosurgery 40, 112-119, doi:10.1159/000079852 (2004). Stripp, D. C. et al. Surgery with or without radiation therapy in the management of craniopharyngiomas in children and young adults. International journal of radiation oncology, biology, physics 58, 714-720, doi:10.1016/S03603016(03)01570-0 (2004). Albright, A. L. et al. Individualized treatment of pediatric craniopharyngiomas. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery 21, 649-654, doi:10.1007/s00381-005-1185-6 (2005). Ersahin, Y., Yurtseven, T., Ozgiray, E. & Mutluer, S. Craniopharyngiomas in children: Turkey experience. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery 21, 766-772, doi:10.1007/s00381005-1187-4 (2005). Karavitaki, N. et al. Craniopharyngiomas in children and adults: systematic analysis of 121 cases with long-term followup. Clinical endocrinology 62, 397-409, doi:10.1111/j.1365-2265.2005.02231.x (2005). Lena, G., Paz Paredes, A., Scavarda, D. & Giusiano, B. Craniopharyngioma in children: Marseille experience. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery 21, 778-784, doi:10.1007/s00381-005-1207-4 (2005). Minamida, Y., Mikami, T., Hashi, K. & Houkin, K. Surgical management of the recurrence and regrowth of craniopharyngiomas. Journal of neurosurgery 103, 224-232, doi:10.3171/jns.2005.103.2.0224 (2005). Mottolese, C., Szathmari, A., Berlier, P. & Hermier, M. Craniopharyngiomas: our experience in Lyon. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery 21, 790-798, doi:10.1007/s00381005-1242-1 (2005). Sainte-Rose, C. et al. Craniopharyngioma: the pendulum of surgical management. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery 21, 691-695, doi:10.1007/s00381-005-1209-2 (2005). Shirane, R., Hayashi, T. & Tominaga, T. Fronto-basal interhemispheric approach for craniopharyngiomas extending outside the suprasellar cistern. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery 21, 669-678, doi:10.1007/s00381-005-1206-5 (2005). 119 120 121 122 123 124 125 126 127 128 129 130 Sosa, I. J., Krieger, M. D. & McComb, J. G. Craniopharyngiomas of childhood: the CHLA experience. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery 21, 785-789, doi:10.1007/s00381-0051225-2 (2005). Thompson, D., Phipps, K. & Hayward, R. Craniopharyngioma in childhood: our evidence-based approach to management. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery 21, 660-668, doi:10.1007/s00381-005-1210-9 (2005). Tomita, T. & Bowman, R. M. Craniopharyngiomas in children: surgical experience at Children's Memorial Hospital. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery 21, 729-746, doi:10.1007/s00381-005-1202-9 (2005). Zuccaro, G. Radical resection of craniopharyngioma. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery 21, 679-690, doi:10.1007/s00381-005-1201-x (2005). Xu, J. G. et al. Microsurgical resection of craniopharyngioma of the third ventricle via an improved transventricular approach. Chinese medical journal 118, 806-811 (2005). Dhellemmes, P. & Vinchon, M. Radical resection for craniopharyngiomas in children: surgical technique and clinical results. Journal of pediatric endocrinology & metabolism : JPEM 19 Suppl 1, 329-335 (2006). Di Rocco, C., Caldarelli, M., Tamburrini, G. & Massimi, L. Surgical management of craniopharyngiomas--experience with a pediatric series. Journal of pediatric endocrinology & metabolism : JPEM 19 Suppl 1, 355-366 (2006). Gupta, D. K., Ojha, B. K., Sarkar, C., Mahapatra, A. K. & Mehta, V. S. Recurrence in craniopharyngiomas: analysis of clinical and histological features. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia 13, 438-442, doi:10.1016/j.jocn.2005.05.013 (2006). Hafez, M. A., ElMekkawy, S., AbdelBadie, H., Mohy, M. & Omar, M. Pediatric craniopharyngioma--rationale for multimodal management: the Egyptian experience. Journal of pediatric endocrinology & metabolism : JPEM 19 Suppl 1, 371-380 (2006). Puget, S. et al. Pediatric craniopharyngiomas: classification and treatment according to the degree of hypothalamic involvement. Journal of neurosurgery 106, 3-12, doi:10.3171/ped.2007.106.1.3 (2007). Lee, Y. Y. et al. Comparison of hypothalamopituitary axis dysfunction of intrasellar and third ventricular craniopharyngiomas in children. Brain & development 30, 189-194, doi:10.1016/j.braindev.2007.07.011 (2008). Shi, X. E., Wu, B., Fan, T., Zhou, Z. Q. & Zhang, Y. L. Craniopharyngioma: surgical experience of 309 cases in China. Clinical neurology and neurosurgery 110, 151-159, doi:10.1016/j.clineuro.2007.10.013 (2008). 131 132 133 134 135 136 137 138 139 140 141 142 143 Zhang, Y. Q., Ma, Z. Y., Wu, Z. B., Luo, S. Q. & Wang, Z. C. Radical resection of 202 pediatric craniopharyngiomas with special reference to the surgical approaches and hypothalamic protection. Pediatric neurosurgery 44, 435-443, doi:10.1159/000172965 (2008). Kawamata, T., Amano, K., Aihara, Y., Kubo, O. & Hori, T. Optimal treatment strategy for craniopharyngiomas based on long-term functional outcomes of recent and past treatment modalities. Neurosurgical review 33, 71-81, doi:10.1007/s10143-009-0220-6 (2010). Elliott, R. E., Jane, J. A., Jr. & Wisoff, J. H. Surgical management of craniopharyngiomas in children: meta-analysis and comparison of transcranial and transsphenoidal approaches. Neurosurgery 69, 630-643; discussion 643, doi:10.1227/NEU.0b013e31821a872d (2011). Jho, H. D. & Carrau, R. L. Endoscopic endonasal transsphenoidal surgery: experience with 50 patients. Journal of neurosurgery 87, 44-51, doi:10.3171/jns.1997.87.1.0044 (1997). Frank, G. et al. The endoscopic extended transsphenoidal approach for craniopharyngiomas. Neurosurgery 59, ONS7583; discussion ONS75-83, doi:10.1227/01.NEU.0000219897.98238.A3 (2006). de Divitiis, E. et al. Extended endoscopic transsphenoidal approach for extrasellar craniopharyngiomas. Neurosurgery 61, 219-227; discussion 228, doi:10.1227/01.neu.0000303220.55393.73 (2007). Cappabianca, P. et al. Extended endoscopic endonasal approach to the midline skull base: the evolving role of transsphenoidal surgery. Advances and technical standards in neurosurgery 33, 151-199 (2008). Cavallo, L. M. et al. The role of the endoscope in the transsphenoidal management of cystic lesions of the sellar region. Neurosurgical review 31, 55-64; discussion 64, doi:10.1007/s10143-007-0098-0 (2008). Gardner, P. A. et al. Outcomes following endoscopic, expanded endonasal resection of suprasellar craniopharyngiomas: a case series. Journal of neurosurgery 109, 6-16, doi:10.3171/JNS/2008/109/7/0006 (2008). Stamm, A. C., Vellutini, E., Harvey, R. J., Nogeira, J. F., Jr. & Herman, D. R. Endoscopic transnasal craniotomy and the resection of craniopharyngioma. The Laryngoscope 118, 1142-1148, doi:10.1097/MLG.0b013e318170b5dc (2008). Ceylan, S., Koc, K. & Anik, I. Extended endoscopic approaches for midline skull-base lesions. Neurosurgical review 32, 309-319; discussion 318-309, doi:10.1007/s10143-009-0201-9 (2009). Dehdashti, A. R., Ganna, A., Witterick, I. & Gentili, F. Expanded endoscopic endonasal approach for anterior cranial base and suprasellar lesions: indications and limitations. Neurosurgery 64, 677-687; discussion 687-679, doi:10.1227/01.NEU.0000339121.20101.85 (2009). Campbell, P. G. et al. Endocrinological and ophthalmological consequences of an initial endonasal endoscopic approach for resection of craniopharyngiomas. Neurosurgical focus 28, E8, doi:10.3171/2010.1.FOCUS09292 (2010). 144 145 146 147 148 149 150 151 152 153 154 155 156 Jane, J. A., Jr., Prevedello, D. M., Alden, T. D. & Laws, E. R., Jr. The transsphenoidal resection of pediatric craniopharyngiomas: a case series. Journal of neurosurgery. Pediatrics 5, 49-60, doi:10.3171/2009.7.PEDS09252 (2010). Gay, E. et al. Chordomas and chondrosarcomas of the cranial base: results and follow-up of 60 patients. Neurosurgery 36, 887-896; discussion 896-887 (1995). Goel, A. Chordoma and chondrosarcoma: relationship to the internal carotid artery. Acta neurochirurgica 133, 30-35 (1995). Carrabba, G., Dehdashti, A. R. & Gentili, F. Surgery for clival lesions: open resection versus the expanded endoscopic endonasal approach. Neurosurgical focus 25, E7, doi:10.3171/FOC.2008.25.12.E7 (2008). Miyagi, A., Maeda, K. & Sugawara, T. [Usefulness of neuroendoscopy and a neuronavigator for removal of clival chordoma]. No shinkei geka. Neurological surgery 26, 169-175 (1998). Jho, H. D. & Ha, H. G. Endoscopic endonasal skull base surgery: Part 3--The clivus and posterior fossa. Minimally invasive neurosurgery : MIN 47, 16-23, doi:10.1055/s-2004-818347 (2004). Solares, C. A., Fakhri, S., Batra, P. S., Lee, J. & Lanza, D. C. Transnasal endoscopic resection of lesions of the clivus: a preliminary report. The Laryngoscope 115, 1917-1922, doi:10.1097/01.mlg.0000172070.93173.92 (2005). Rudnik, A. et al. Endoscopic transnasal transsphenoidal treatment of pathology of the sellar region. Minimally invasive neurosurgery : MIN 48, 101-107, doi:10.1055/s-2004-830185 (2005). Frank, G. et al. The endoscopic transnasal transsphenoidal approach for the treatment of cranial base chordomas and chondrosarcomas. Neurosurgery 59, ONS50-57; discussion ONS50-57, doi:10.1227/01.NEU.0000219914.17221.55 (2006). Hwang, P. Y. & Ho, C. L. Neuronavigation using an image-guided endoscopic transnasal-sphenoethmoidal approach to clival chordomas. Neurosurgery 61, 212-217; discussion 217-218, doi:10.1227/01.neu.0000303219.55393.fe (2007). Pirris, S. M. et al. Corridor surgery: the current paradigm for skull base surgery. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery 23, 377-384, doi:10.1007/s00381-006-0281-6 (2007). Dehdashti, A. R., Karabatsou, K., Ganna, A., Witterick, I. & Gentili, F. Expanded endoscopic endonasal approach for treatment of clival chordomas: early results in 12 patients. Neurosurgery 63, 299-307; discussion 307-299, doi:10.1227/01.NEU.0000316414.20247.32 (2008). Zhang, Q., Kong, F., Yan, B., Ni, Z. & Liu, H. Endoscopic endonasal surgery for clival chordoma and chondrosarcoma. ORL; journal for oto-rhino-laryngology and its related specialties 70, 124-129, doi:10.1159/000114536 (2008). 157 158 159 160 161 162 Hong Jiang, W. et al. Endoscopic resection of chordomas in different clival regions. Acta oto-laryngologica 129, 71-83, doi:10.1080/00016480801995404 (2009). Stippler, M. et al. Endoscopic endonasal approach for clival chordomas. Neurosurgery 64, 268-277; discussion 277-268, doi:10.1227/01.NEU.0000338071.01241.E2 (2009). Fraser, J. F., Nyquist, G. G., Moore, N., Anand, V. K. & Schwartz, T. H. Endoscopic endonasal transclival resection of chordomas: operative technique, clinical outcome, and review of the literature. Journal of neurosurgery 112, 10611069, doi:10.3171/2009.7.JNS081504 (2010). Fraser, J. F., Nyquist, G. G., Moore, N., Anand, V. K. & Schwartz, T. H. Endoscopic endonasal minimal access approach to the clivus: case series and technical nuances. Neurosurgery 67, ons150-158; discussion ons158, doi:10.1227/01.NEU.0000383130.80179.41 (2010). Alexander, H., Robinson, S., Wickremesekera, A. & Wormald, P. J. Endoscopic transsphenoidal resection of a mid-clival meningioma. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia 17, 374-376, doi:10.1016/j.jocn.2009.06.037 (2010). Holzmann, D., Reisch, R., Krayenbuhl, N., Hug, E. & Bernays, R. L. The transnasal transclival approach for clivus chordoma. Minimally invasive neurosurgery : MIN 53, 211-217, doi:10.1055/s-0030-1267929 (2010).