Katie A Overview

KATIE A. VS. BONTA: MENTAL HEALTH SERVICES FOR FOSTER
CHILDREN
The 2011 settlement of the class action case Katie A. vs. Douglas (previously Katie A. vs. Bonta) mandates the provision of intensive in-home and community-based mental health services for
California children who are in foster care or at imminent risk of removal from their families.
This settlement will alter existing policies and practices in counties, by promoting mental health assessments for children involved in foster care, as well as provision of community-based services rather than services provided at large facilities or group homes. The agreement requires the California Department of Social Services (CDSS) and the California Department of Health
Care Services (CDHCS) to provide coordinated, comprehensive, community-based services to children at risk of out-of-home-placement or in foster care and their families. CDSS and
CDHCS will develop a Core Practice Model (CPM), a guiding framework for intensive care coordination, intensive home-based mental health services, therapeutic foster care, and the establishment of child and family teams. Counties will participate in the development and implementation of the CPM.
Background
The Katie A. vs. Bontá case was first filed in July of 2002 as a class action suit on behalf of children who were not given proper services by both the child protective system and the mental health system in California. It was originally filed against the Los Angeles County Department of Children and Family Services (DCFS); Anita Bock, Director of DCFS; Diana Bonta (then
Director of the California Department of Health Services); and Rita Saenz (then Director of the
California Department of Social Services).
When the class action suit was filed, LA County’s foster care system was the largest in the U.S.
Gould, Townsend and Welch (2006) reported that the Little Hoover Commission estimated that
70% of children in foster care in California would experience a mental health problem at some point in their lives (p.7). The authors also reported that CDSS acknowledged that “many children have been caught in a revolving door of inappropriate placements,” and that the “typical child in group care has experienced an average of five different placements before being put in a group home.” (p. 8).
The plaintiff, Katie A., was a 14-year old Caucasian girl in 2002. She was removed from her home at age four and had been in foster care for 10 years. At age five, assessments of Katie indicated that she was a victim of trauma and needed intensive trauma treatment and supportive services for her caregiver. From the age of eight, Katie was placed almost solely in congregate
1
care facilities despite the fact that multiple assessments and recommendations from mental health professionals showed that she responded best to one-on-one attention, and had difficulty with peer relations. She was moved through 37 different placements, including four group homes, 19 different stays at psychiatric hospitals, a two-year stay at Metropolitan State Hospital, and seven different stays at MacLaren Children’s Center. She never received trauma treatment or other individualized outpatient mental health services. The lawsuit alleged that these experiences led to her emotional and educational deterioration.
The other children who were plaintiffs in the case had similar stories: several had experienced multiple psychiatric hospitalizations but never had comprehensive psychiatric assessments, and never received regular counseling. They all had numerous placements (ranging from 12 to 28).
Several also had physical disabilities that were not taken into account or addressed properly. A group of public interest law firms filed on behalf of a class of children in California who were:
(1) in foster care or were at imminent risk of foster care placement, (2) had a mental illness or condition documented through assessments, and (3) needed individualized mental health services. DCFS settled the lawsuit against it in 2003, agreeing to close McLaren Children’s
Center, its children’s shelter that had been the target of multiple grand jury investigations, and to institute family-based wraparound services for children with emotional disorders. The LA
County Katie A. settlement plan was finalized in 2008 and includes a core practice model for
DCFS with joint training for their staff and staff of LA Department of Mental Health Children’s
Services. CDSS and CDHCS continued to appeal court findings until 2009 when they entered into a settlement process facilitated by a Special Master appointed by the U.S. District Court.
The agreement was approved by the District Court in December, 2011 and the parties have begun to develop an implementation plan. Full implementation is expected by 2014.
The California settlement agreement ( Katie A. et al v. Diana Bontá et al) identifies inclusion criteria for children, service objectives and lays out specific actions that will further the implementation of the settlement.
Criteria for Inclusion
Eligible children and youth are those who are full-scope Medi-Cal, meet medical necessity for treatment, have an open child welfare services case, and meet either of the following criteria:
Currently in or being considered for: Wraparound, therapeutic foster care or other intensive services, therapeutic behavioral services, specialized care rate due to behavioral health needs or crisis stabilization/intervention;
Currently in or being considered for a group home, a psychiatric hospital or 24 hour mental health treatment facility, or has experienced his/her 3 rd
or more placement within 24 months due to behavioral health needs.
2
Objective of services
The settlement delineates the objective of the services to be provided:
1.
Facilitate the provision of an array of services delivered in a coordinated, comprehensive, community-based format that allows for service access, planning, delivery, and transition into a coherent, all-inclusive approach;
2.
Support the development and delivery of a service structure involving standards and methods to achieve quality oversight, and training and education that support the practice and fiscal models;
3.
Address the need for certain foster children or children at imminent risk with more intensive needs to receive medically necessary mental health services in their own home, a family setting, or the most homelike setting appropriate to their needs, in order to facilitate reunification, and to meet their needs for safety, permanence and well-being.
Implementation Planning
The settlement also outlines the broad process for planning and implementation:
As the majority of the children in this class are eligible for Medi-Cal, the state agencies, in collaboration with a negotiation work group and other stakeholders, will develop and disseminate a Medi-Cal Specialty Mental Health Documentation
Manual that will inform and instruct providers on two arrays of service: Intensive
Care Coordination, and Intensive Mental Health Home Based Services, as well as evidence-based practices in Therapeutic Foster Care (e.g. Multidimensional
Treatment Foster Care, Intensive Treatment Foster Care)
CDMH (and now the Department of Health Care Services due to the imminent closure of CDMH) and CDSS are to “establish a shared management structure, develop a shared vision and mission statement, policy and program direction. They should have clear and consistent guidance and outcomes, and accountability measures consistent with the Core Practice Model” (CPM)
They will also develop models for local agencies to work more effectively together, and to assist in integration of departments and services. CDMH and CDSS will conduct a statewide readiness assessment of counties and select at least three counties (large, medium, small) to develop and model child welfare and mental health service delivery systems that can be successful in implanting the CPM. CPM establishes and adheres to a prescribed set of family-centered values and principles that are driven by a definable process. The process for all Katie A. class members requires engaging families, assessment, service planning and implementation, monitoring and adapting, and transition. It is expected that a subset of Katie A.-
3
eligible children and youth will need a more intensive approach and service delivery, and would best be served through a formally organized Child and Family Team.
Issues for Discussion
Additional information from the settlement about CPM and its key elements is in Appendix A.
The settlement requires collaboration and teamwork at all levels of the child welfare and mental health systems to ensure that children in the child welfare system who have mental health problems have early and consistent access to high-quality treatment services. Collaborative program strategies are already in place in many counties (e.g. Wraparound, Team Decision-
Making, and Multi-Disciplinary Teams) and the core competencies for this work are fundamental to social work education and practice.
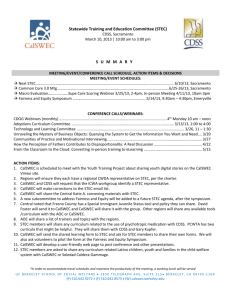
CalSWEC has begun laying the foundation for working with our partners on settlement implementation. CalSWEC staff recently has formed a small workgroup to coordinate and collaborate on our internal efforts. CalSWEC and CDSS co-chair the Statewide Training and
Education Committee (STEC), a collaboration of multiple organizations dedicated to public child welfare training and staff development in California. STEC develops and/or recommends standard for statewide public child welfare training and coordinates their implementation.
Accordingly, the settlement directs CDSS to initiate a request to STEC to develop a process and timeline for development of cross-system curriculum and training materials. These materials are intended to train county child welfare and mental health staff, and are intended to develop and promote teaming strategies at all levels (e.g. Team Decision Making meetings, Child and Family
Teams, Interagency Placement Review Teams, Departmental Leadership Team Meetings, etc.)
In addition, in 2010 the CalSWEC Mental Health Program developed and disseminated a curriculum module focused on child welfare and mental health collaboration for MSW programs.
Actions for discussion:
(1) The Child Welfare and Mental Health Initiative Committees consider a recommendation to the Board for CalSWEC staff to continue internal and external activities to successfully implement in-service and MSW training for collaborative, community-based services for children in foster care with mental health problems.
(2) The Committees also consider recommending that the Board communicate to the
Department of Health Services (DHCS) that collaboration on the settlement with CDSS must remain a high priority for DHCS, even though the Department of Mental Health will no longer be able to meet the settlement requirements.
4
Appendix A – Information on the Core Practice Model
5
Appendix A – Information on the Core Practice Model
6
Appendix A – Information on the Core Practice Model
7
Appendix A – Information on the Core Practice Model
8
Appendix A – Information on the Core Practice Model
9
Appendix A – Information on the Core Practice Model
References
Bazelon Center for Mental Health Law (2006). “Suit against Nation’s Largest Child Welfare
System Settled with Commitment to Reform.” Press release. Retrieved from http://bazelon.org.gravitatehosting.com/LinkClick.aspx?fileticket=PbwJ16pejlo%3d&tabid=328
Gould, Robyn, Townsend, Laura, Welch, Leecia. Landmark Decision for California’s Most
Vulnerable Children. Youth Law News, 27-2, 7-9.
Katie A. et al v. Diana Bontá Settlement Agreement (2011).
10