Zincofer/Iberet 1/1 od (with counseling)
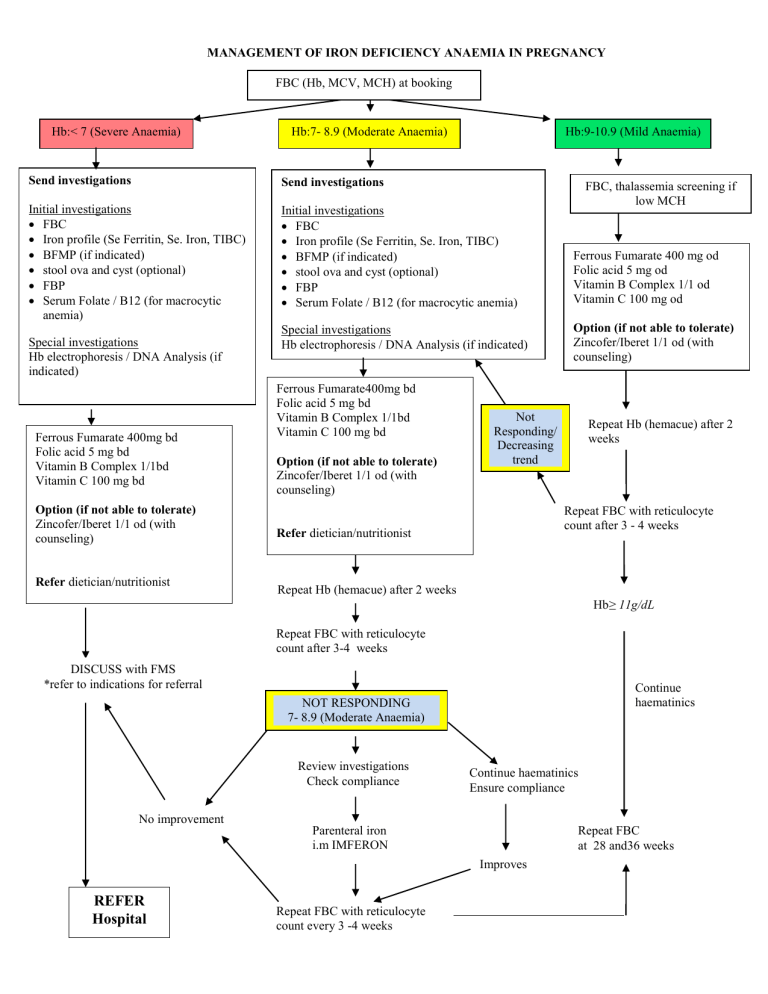
MANAGEMENT OF IRON DEFICIENCY ANAEMIA IN PREGNANCY
FBC (Hb, MCV, MCH) at booking
Hb:< 7 (Severe Anaemia)
Send investigations
Initial investigations
FBC
Iron profile (Se Ferritin, Se. Iron, TIBC)
BFMP (if indicated)
stool ova and cyst (optional)
FBP
Serum Folate / B12 (for macrocytic anemia)
Special investigations
Hb electrophoresis / DNA Analysis (if indicated)
Hb:7- 8.9 (Moderate Anaemia)
Send investigations
Initial investigations
FBC
Iron profile (Se Ferritin, Se. Iron, TIBC)
BFMP (if indicated)
stool ova and cyst (optional)
FBP
Serum Folate / B12 (for macrocytic anemia)
Special investigations
Hb electrophoresis / DNA Analysis (if indicated)
Ferrous Fumarate 400mg bd
Folic acid 5 mg bd
Vitamin B Complex 1/1bd
Vitamin C 100 mg bd
Ferrous Fumarate400mg bd
Folic acid 5 mg bd
Vitamin B Complex 1/1bd
Vitamin C 100 mg bd
Option (if not able to tolerate)
Zincofer/Iberet 1/1 od (with counseling)
Zincofer/Iberet 1/1 od (with counseling)
Refer dietician/nutritionist
Refer dietician/nutritionist
Repeat Hb (hemacue) after 2 weeks
DISCUSS with FMS
*refer to indications for referral
Repeat FBC with reticulocyte count after 3-4 weeks
NOT RESPONDING
7- 8.9 (Moderate Anaemia)
No improvement
Check compliance
Parenteral iron i.m IMFERON
REFER
Hospital
Repeat FBC with reticulocyte count every 3 -4 weeks
Not
Responding/
Decreasing trend
7- 8.9
(Moderate
Anaemia)
Repeat Hb (hemacue) after 2 weeks
Repeat FBC with reticulocyte count after 3 - 4 weeks
Ensure compliance
Improves
Hb:9-10.9 (Mild Anaemia)
FBC, thalassemia screening if low MCH
Ferrous Fumarate 400 mg od
Folic acid 5 mg od
Vitamin B Complex 1/1 od
Vitamin C 100 mg od
Option (if not able to tolerate)
Zincofer/Iberet 1/1 od (with counseling)
Hb ≥ 11g/dL
Continue haematinics
Repeat FBC at 28 and36 weeks
Definition (WHO): Hb< 11g/dl
In moderate to severe anaemia, monitor for IUGR by serial symphysiofundal height and serial ultrasound scan monthly plotted on the growth chart.
Discuss with FMS
1. Thalasemia cases
2. Severe Anaemia Cases
3. Cases not responding to treatment
4. Cases that needs referral to hospital
INDICATIONS FOR REFERRAL TO HOSPITAL
1) Severe anaemia (Hb< 7g/dl) more than 32 weeks gestation
2) Moderate anaemia (Hb 7 -8.9) with symptoms and signs of cardiovascular decompensatione,.g. reduced effort tolerance, breathlessness
3) Asymptomatic moderate anaemia (Hb 7 -8.9) in the third trimester with risk of postpartum haemorrhage (if poor response to initial management)
Grandmultiparity
Multiple pregnancy
Past history of PPH
Polyhydramnios
4) Thalassaemia not responding to haematinics. (Consider prenatal diagnosis in early pregnancy for cases with concordant husband’s status).
5) Evidence of IUGR
Notes:
At least 180mg/day of elemental iron is required for therapeutic treatment.
Obimin (1tablet) = 30 mg elemental iron
= 36mg elemental iron Ferrous Sulphate (300mg)
Ferrous Fumarate (200mg)
Iberet (1 tablet)
Zincofer (1 tablet)
= 66mg elemental iron
= 105mg elemental iron
= 115 mg elemental iron
Medication and dietary advise
1. Dietary advice should include good preparation of foods.
haem-iron are more readily absorbed ( source e.g. meat, poultry)
Folate (and other vitamins) in vegetable sources are easily destroyed by heat (do not overcook)
2. Counseling for iron intake :
compliance
best taken on empty stomach
avoid taking together with substances which can inhibit iron absorption (tea, coffee, egg yolk, phytates in grains , cereals, legumes).
iron absorption is enhanced by citrus.
advise on measures to avoid constipation when taking haematinics
3. Continue iron supplements until at least 3 months after delivery and advise on suitable contraceptive methods
Parenteral iron supplement
1) Indications - i) unable to tolerate oral haematinics
ii) poor compliance
iii) poor absorption of oral haematinics
2) Refer to Imferon Dose regime from HKL
3) Continue oral intake of Vitamin B-co, Vitamin C and Folic acid
4) Thalassaemia must be excluded first before administration of imferon
PRACTICAL TIPS OF MANAGEMENT
NOT COST EFFECTIVE to religiously investigate mild anemia
Our resources and facilities are limited
A known fact : Iron deficiency anemia is the most common type of anemia and a FULL
BLOOD COUNT will reveal reduced MCV, MCHC and MCH.
These patients can be empirically treated with therapeutic dosage of iron supplementations.
A full blood picture is NOT routinely required to confirm a hypochromic microcytic anemia unless the classical features of iron deficiency anemia are absent.
Is it NOT COST EFFECTIVE to perform a battery of investigations for all anemia cases (eg
FBP, Se Ferritin, TIBC, stool ova & cyst, HB electrophoresis, Hb analysis).
Be SELECTIVE in your approach
WHEN DO WE NEED TO INVESTIGATE FURTHER
All moderate or severe anemia needs to be investigated (Hb<9g/dl)-refer to flow chart
If compliance in not an issue but there is no response to iron supplementations after at least 3 weeks of treatment (haemoglobin increases by 0.3g/week), that is indication for further investigations
WHEN DO WE NEED TO INVESTIGATE FOR THALASSAEMIA
1. In patients who have a significant family history of thalassemia
2. MCH is the most important screening parameter for thalassaemia. i.e low MCH < 27pq
3. Even with a normal haemoglobin levels but low MCH is an indication to screen for thalasemia.
4. Iron deficiency anemia which does not respond to iron supplementations.
TREATMENT FOR MEGALOBLASTIC ANAEMIA
FOLATE DEFICIENCY
Treatment with 1 mg of folic acid administered orally each day typically produces an appropriate response
VITAMIN B12 DEFICIENCY
A single dose of 1000ug of IM B12 should lead to a reticulocyte response within 3-7 days
Weekly injections should be employed until anemia resolves and lifelong replacement is often required
SUMMARY OF RECOMMENDATIONS FROM:
1. THE UK GUIDELINES ON THE MANAGEMENT OF IRON DEFICIENCY IN PREGNANCY
2. THE MALAYSIAN CPG 2007: MANAGEMENT OF ANEMIA IN PREGNANCY AND
CHRONIC KIDNEY DISEASE
SUMMARY OF RECOMMENDATIONS FROM THE UK GUIDELINES ON THE
MANAGEMENT OF IRON DEFICIENCY IN PREGNANCY
Full blood count should be assessed at booking and at 28 weeks (1A).
A trial of oral iron should be considered as the first line diagnostic test for normocytic or microcytic anaemia. An increase in Hb must be demonstrated at 2 weeks, otherwise further tests are needed (1B).
Women with a Hb<110 g/l before 12 weeks or <105 g/l beyond 12 weeks are anaemic and should be offered a trial of therapeutic iron replacement, unless they are known to have a haemoglobinopathy (1B).
The serum ferritin level is the most useful and easily available parameter for assessing iron deficiency. Levels below 15 μg/l are diagnostic of established iron deficiency. A level below
30 μg/l in pregnancy should prompt treatment (2A).
Treatment should start promptly in the community and referral to secondary care should be considered if anaemia is severe (Hb<70 g/l) and/or associated with significant symptoms or advanced gestation (>34 weeks) (2B). In these cases the starting dose should be 200mg elemental iron daily.
Repeat Hb testing is required 2 weeks after commencing treatment for established anaemia, to assess compliance, correct administration and response to treatment (1B).
If response to oral iron replacement is poor, concomitant causes which may be contributing to the anaemia, such as folate deficiency or anaemia of chronic disease, need to be excluded and the patient referred to secondary care (1A).
Dietary changes alone are insufficient to correct iron deficiency anaemia and iron supplements are necessary. Ferrous iron salts are the preparation of choice. The oral dose for iron deficiency anaemia should be 100-200mg of elemental iron daily (1A).
Women should be counselled as to how to take oral iron supplements correctly. This should be on an empty stomach, 1 hour before meals, with a source of vitamin C (ascorbic acid) such as orange juice to maximize absorption. Other medications or antacids should not be taken at the same time (1A).
Parenteral iron should be considered from the 2nd trimester onwards and post partum period in women with iron deficiency anaemia who fail to respond to or are intolerant of oral iron (1A).
SUMMARY OF RECOMMENDATIONS FROM THE MALAYSIAN CPG 2007 :
MANAGEMENT OF ANEMIA IN PREGNANCY AND CHRONIC KIDNEY DISEASE
1. Iron supplementation during pregnancy
The W.H.O. recommends universal oral iron supplementation for pregnant women (60 mg of elemental iron and 5 mg of folic acid once or twice daily) for:
•
•
6 months in pregnancy in countries with a prevalence of anemia <40%
An additional 3 months post-partum in countries where the prevalence is >40%.
(Evidence level B)
S t o l t z fu s R,Dreyf us s M L.
G ui de li nes for t he useo f iro n s up p lemen t s t o p re v e n t a nd treat iro n deficiency a n e mia. G e n e v a: I N A GG , WH O, UNICEF , 1 998 .
The studies show improved maternal and prenatal outcome by routine iron supplementation during pregnancy.
(Evidence level A)
Mary E.C. et al. Iron supplementation during pregnancy, anemia, and birth weight: a randomized controlled trial. Am J ClinNutr 2003;78:773-81.
Mahomed K.Routine iron supplementation during pregnancy.(Cochrane Review).The
Cochrane Library, Issue 2. Oxford; Update Software: 2005.
2. Management of Iron Deficiency Anaemia
Oral iron: l) IDA should be treated with iron supplementation in all trimesters.
The clinical severity of the anemia from the haemoglobin levels and symptoms; and the stage of gestation of the pregnancy are factors that guide therapy.
If oral iron is not tolerated due to nausea and vomiting, supplementation before bedtime or other routes of iron supplementation should be considered. ii) For prophylaxis, 100 mg of elemental iron with 5 mg folic acid is recommended. iii) For treatment 180 mg of elemental iron with 5 mg of folic acid is recommended.
(Evidence level A)
Mahomed K.Routine iron supplementation during pregnancy.(Cochrane Review).The
Cochrane Library, Issue 2. Oxford; Update Software: 2005.
iv) Patient's response to 180 mg elemental iron per day is fast:
• Significant increase in reticulocyte count within 5 - 10 days of start of oral therapy.
• Haemoglobin rises from 0.3 9 to 1.0 9 per week
3. Prevention of iron deficiency
Prevention of iron deficiency in pregnancy include the following:
Prophylaxis of non-pregnant women to replenish iron stores
Mahomed K.Routine iron supplementation during pregnancy.(Cochrane Review).The
Cochrane Library, Issue 2. Oxford; Update Software: 2005.
Improvement of dietary habits and improving the bioavailability of food-iron (not to overcook as vitamin C is destroyed).
Social factors: improvement of sanitation, personal hygiene, better education especially for women, alleviation of poverty.
Food fortification
(Evidence level C)
4. Treatment of hookworm infestation
Oral antihelminthic treatment is safe to be given to pregnant and lactating women.
Single albendazole (400 mg) or mebendazole (100 mg) doses twice daily for 3 days.
(Evidence level B)
Sh ar m a J B, Ar o r a BS , Kuma r S , Ga e l S, Dh am i j a A.
Helminth a n d pr oto zo a n i nt es t ina l infecton s: an i m p o rta n t cau se f o r a nemia Inp r e g n ant w o men inDe l h i , In d ia . J
Obs t e tG ynecol l nd 2 0 0 1 : 5 1( 6 ) : 5861 .
A tu korala T ,deS il v a L D , D e cher ingWH , Da ssen ai k e T S , Per e r aRS .E
va lu at i o nof e ff e c t i v eness o f iro n f olate s u ppl e m e n ta ti o n a n d a n ti-h e lm i nth i c t he r ap y agai n s t a n e m i a i n p r e g na n cy - s tu dy i n t h e p la n ta ti o n se c t o r of S riL a n k a .
A m J Cli n N u t r1 9 9 4 ; 60: 2 86 - 2 9 2 .
5. Blood Transfusion
• Blood transfusion does not correct the underlying iron deficiency
• Parenteral iron therapy is preferred to avoid blood transfusion if possible delay in delivery beyond two weeks.
• Risk of transmitting infection should be weighed against the benefit of blood transfusion.
• Patients who refuse blood transfusion (for religious reasons) - iron deficiency should be corrected with oral iron, and human recombinant erythropoietin (rhEPO) .
Medical care should be optimised to minimize the blood loss.
(Evidence level D)
E m ma n u e l.
Ke t a l. T rip l et preg n ancy i n a J eh o v a h ' s W itn ess: reco mb i n a n t h uman e r y t hr o p o i e tin and i r on su pp lem e n ta ti o n for minimizing th e r i s k s of exce ss i ve blo od l oss.
Br J O bstet Gya n eco I 2 002 ; 1 0 9:723 -725.
C h ri s t i an S r e ym a n n e t al , R eco m b i na nt H u ma n e r yt hr o p o i e t i n a n d p a r en te r a l ir o n i n t he t r e a t m e nt o f p r eg nan cy ane m i a : a p ilo t s t u d y . J . P e rinat.Med. 2 3 ( 199 5 ) 89 98
Only judicious use of blood transfusions is indicated. Anemia due to iron deficiency do not require transfusions unless there are symptoms of decompensation and otherwise debilitated.
(Evidence level C)
Gui delin e fo r R atio n a l U s e o f B l oo d Prod u c t s, 1 9 93pag e 9, M edica l Co nse ns u s Deve l o pm e nt
Pan e l , M i ni s try of H e a l t h and Acad emy of M e dici n e








