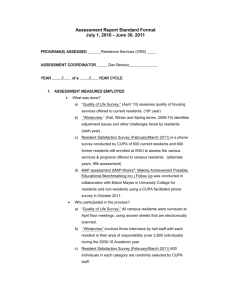
CompetencyBasedCurriculum
advertisement

Contents A. General Information a. PGY 1 Year b. PGY 2 Year c. PGY 3 Year B. Curriculum a. Cardiology b. Critical Care c. Endocrinology d. Gastroenterology e. General Medicine f. Geriatrics / Palliative Care g. Hematology h. Infectious Diseases i. Oncology j. Pulmonary k. Renal l. Rheumatology C. Rotation Information a. Emergency Room A. General Information 1. Organization and Structure a. The Department of Medicine at the University of North Carolina at Chapel Hill provides an integrated, progressive experience for residents in their 36- month training period. The goal of our curriculum is to prepare residents to be welltrained general internists. We believe this type of training not only prepares our residents for careers in General Internal Medicine but also provides the necessary foundations for further training as a subspecialist. The curriculum in the Department of Medicine changes greatly from the PGY 1 year to the PGY 3 year. The PGY 1 year consist of 9 months of inpatient rotations and 3 months of ambulatory medicine. During the second and third years, residents spend an increasing amount of time in the outpatient setting. The curriculum will be specifically described for each of the 3 year of training. The PGY 1 Year Each PGY 1 resident must develop competence in the following categories: Patient Care Medical Knowledge Practice Base Learning and Improvement Interpersonal and Communication Skills Professionalism System Based Practice In the context of monthly rotations, competency is defined for each of the categories. Patient Care- medical interviews, physical examinations, review of data, procedural skills, diagnostic and therapeutic decision making Medical Knowledge- basic and clinical science, evidence- based medicine, literature searching Practice Based Learning and Improvement- evaluation of own performance, incorporation of feedback, use of technology for patient care and self improvement Interpersonal and Communication Skills- establishment of relationships with patients and families, education and counseling of patients, team skills with colleagues Professionalism- demonstration of respect, compassion, integrity, and honesty, commitment to self assessment, acknowledges errors, considers needs of patients and colleagues System Based Practice- ability to utilize resources, use a systematic approach to reduce errors and improve patient care These competencies are reviewed with all residents and the faculty and serve as the foundation for monthly evaluation. The evaluation tool includes a description of each of the core competencies and a scale of evaluation for each from 1-9. A copy of the evaluation took is included in Section ___. ------------------The PGY 1 curriculum consists of a series of monthly rotations linked with a number of Departmental teaching conferences. The monthly inpatient rotations for each PGY 1 resident are as follows: Cardiology/MICU- 2 months Inpatient General Medicine Ward- 2months Inpatient Subspecialty Wards- 5months On all inpatient rotations the role of the PGY 1 resident is to serve as the primary physician for all of his/her patients. In this role the PGY1 resident: 1. Performs a history and physical examination on each new patient 2. Enters all orders 3. Communicates with the patient and ward team regarding daily progress 4. Enters a history and physical and daily progress notes into the patient record 5. Develops a diagnostic and therapeutic plan for each patient 6. Enters a discharge summary in to the patient record Cardiology -consists of 32 beds covered by four teams. Each team is made up of one upper level resident and one PGY 1 resident. One faculty member and one subspecialty fellow are assigned to each team to assist in patient management and to conduct teaching rounds. Didactic teaching rounds and bedside teaching occur daily. Also, there is a weekly core curriculum lecture series that is case- based. A copy of the Cardiology Curriculum is included in Section 2. Common diagnoses of patients admitted to the cardiology service included myocardial infarction, arrhythmias, and chronic heart failure. Residents follow patients in the CCU (12 beds) and the general floor (20 beds). Residents on service place central lines including Swan Ganz catheters and perform arterial blood gases and thoracenteses. ICU- Consist of 19 beds in a MICU. There are 4 teams, each team consisting of one upper level resident and one PGY 1 resident. One faculty member serves as the attending in the MICU. There is also a Critical Care Fellow. Teaching rounds include didactic presentations (30 min/day, 6 days/week), bedside teaching(2hours/day, 7days/week), and x-ray teaching (30 minutes/day,6days/week). There is a designated curriculum (Section 2). Patients admitted commonly have the following diagnoses: GI bleeding, septic shock, drug overdose, s/p cardiopulmonary arrest, DIC, COPD exacerbation, cystic fibrosis exacerbation, rejection s/p lung transplant, and acute renal failure. Residents perform all procedures. Inpatient General Internal Medicine - consists of 2 general medicine services. For each service, there is one attending, one upper level resident, and two PGY 1 residents. Teaching rounds occur for one hour, five times per week covering a number of topics described in the Inpatient General Medicine curriculum (see Section 2). Patients admitted have a variety of problems including: community acquired pneumonia, COPD exacerbation, diabetic complications, and lupus complications. Residents perform all procedures. Also, residents rotate at Wake Hospital, a community hospital in Raleigh, NC. There are four teams consisting of one attending, one upper level resident, and one PGY 1 resident. Teaching rounds occur for one hour five times per week covering topics in General Internal Medicine. Residents perform all procedures. Inpatient Subspecialty WardsService Medicine A-Geriatrics Medicine B- Nephrology 20 Medicine E- Hematology/Oncology Medicine G- Pulmonary Medicine K- Infectious Disease #beds 20 40 20 20 For each service there is one attending, one upper level resident, and two PGY 1 residents. Each of these services has daily work rounds and attending rounds. Each service has designated reaching time occurring at a minimum of five hours per week. During teaching time a series of topics pertinent to each service are reviewed. A copy of each curriculum is included in Section 2. Residents perform all procedures on these services. The PGY 1 Curriculum also includes the following rotations: Emergency Medicine- 1 month Same Day Clininc-1 month Continuity Care/Ambulatory Elective- 1 month Emergency Room – faculty from the Department of Emergency Medicine supervise PGY 1 residents. PGY 1 residents have a generic experience seeing medical, surgical, and obstetrics/gynecology patients. There are four hours of didactic teaching per week, which cover a wide variety of topics. Examples of monthly topics are included in Section 3. Same Day Clinic- This is a walk in clinic for the established IM patients and also serves as an Urgent Care clinic. Faculty in the Division of General Internal Medicine supervise PGY 1 residents. A variety of outpatient problems are encountered. Didactic teaching takes place daily for 30 minutes. Subjects covered in the curriculum are included in Section 3. Continuity Care/Ambulatory Elective- PGY 1 residents spend one month in the General Medicine clinics working with Faculty from the Division of General Medicine. Some of the modules include enhanced care in anticoagulation, diabetes, pain management, and travel medicine. Each resident also undertakes a CQI project. PGY 1 residents may also rotate on a subspecialty service of the Department of Medicine. Consultations are done on inpatients and outpatients and patients are also seen in subspecialty clinics. Division faculty provide supervision. Curricula for each rotation are included in Section 3. Teaching Conferences PGY1 residents attend a series of Departmental Conferences. The daily work schedule is set up to allow PGY 1 residents to attend the conferences (Table 1). Table 1 UNC Department of Medicine- Schedule of Daily Activities Time 0700 0745 0830 Monday Pre Rounds Residents Report Tuesday Pre Rounds Residents Report Wednesday Pre rounds Residents Report Thursday Pre Rounds Residents Report Friday Pre Rounds Residents Report 0830 1030 1100 (flexible) Work Rounds Attending Rounds Work Rounds Attending Rounds Work Rounds Attending Rounds Work Rounds Attending Rounds Work Rounds Attending Rounds 1200 Core Curriculum Core Curriculum Intern Conference Grand Rounds/ Morbidity and Mortality Conference EBM Conference Residents are expected to attend all conferences. The conferences are as follows: Monday- Resident Core Curriculum Conference 1 hour Tuesday- Resident Core Curriculum Conference 1 hour Wednesday- Interns Conference 1 hour Thursday- Grand Rounds 1 hour Friday – EBM Conference 1 hour The content of some of these conferences is briefly described. Lecture topics are included in Section 4. Monday and Tuesday- Residents Conference- Faculty in the Department of Medicine presents a series of lectures covering focused topics. Wednesday- Interns Conference- A lecture series o f Emergency Medicine Topics mixed with case based group discussion. Thursday- Grand Rounds Thursday- Mortality and Morbidity- The morbidity and mortality conference centers on a subject relating to patient care in the department. The Vice Chair of the department conducts this lecture. Friday- Evidence Based Medicine Conference- An evidence based medicine discussion of selected literature by both faculty and residents. The PGY 2 Year Each PGY 2 resident must demonstrate competence in the following: Patient Care Medical Knowledge Practice Based Learning and Improvement Interpersonal and Communication Skills Professionalism System Based Practice Competency is defined as outlined above for PGY 1 residents and is used for monthly evaluations of PGY 2 residents The PGY 2 year is composed of a series of monthly rotations coupled with Departmental teaching conferences. The monthly inpatient rotations for a PGY 2 resident are as follows: 1. MICU- 1month 2. 3. 4. 5. Cardiology- 2months UNC inpatient Medicine Ward- 2-3 months Wake Med- 1 month Night Float- 2-3 2 week blocks On inpatient rotations the role of the PGY 2 resident is to be in charge of the ward team. In this role the PGY 2 resident: 1. 2. 3. 4. 5. Performs a history and physical examination on each new patient Reviews the treatment plan for each new patient with the PGY 1 resident Reviews the performance of MS 3 students Conducts daily work rounds Supervises all procedures On night float the PGY 2 resident reports at 7pm and until 7 am. They are responsible for the primary evaluation and management of all non-intensive care patients admitted to the Department of Medicine. At 7am the care of those patients goes to the incoming team on call. The Attending Physician of the service provides supervision. Cardiology/ICU/Inpatient General Medicine Wards/Inpatient Subspecialty Wards - These have been previously described under the PGY 1 resident. The role of the PGY 2 resident on these services is supervisory. The PGY 2 resident evaluates all patients on service and the PGY 2 resident is integral in constructing a plan of care, which is carried out by the PGY 1 resident. Another major responsibility is teaching. The PGY 2 resident teaches and supervises medical students on these services. The PGY 2 curriculum also includes the following rotations: Ambulatory General Internal Medicine- 2-3 months Subspecialty Consultation- 2-3 months Ambulatory General Internal Medicine – PGY 2 residents can choose from several month blocks focusing on outpatient skills of the generalist. Some of the choices are: Wake Hospital Ambulatory Rotation Siler City- PGY 2 residents spend the month in a community setting supervised by general internists. Subspecialty Consultation- PGY 2 residents can choose among any subspecialty in the Department of Medicine. Consultations are done on inpatients. Patients are also seen in subspecialty clinics. Division faculty provides supervision. Curricula for each rotation are included in Section 3. Teaching Conferences Like PGY 1 residents, PGY 2 residents attend a series of conferences, which are integrated with the daily work schedule. Some have been described previously including Monday Resident Core Curriculum, Tuesday Core Curriculum, Thursday Grand Rounds and Friday Evidence Based Medicine. In addition, PGY 2 residents attend Morning report. This is case- based with residents presenting unknown patients to their peers. The presenting resident completes his /her presentation with a review of a particular subject. This review like all presentations is posted on the internet so that residents may review these at their leisure. These conferences are coordinated by the Chief Residents. The curriculum is set by the chief residents; a list of topics discussed is included in Section 4. The PGY 3 Year ACGME Competencies Each PGY 3 resident must develop competency in the following: Patient Care Medical Knowledge Practice Based Learning and Improvement Interpersonal and Communication Skills Professionalism Systems Based Practice Competency is defined as outlined above for the PGY 1 and PGY 2 residents and is used in monthly evaluation. In many ways the PGY 3 year is similar to the PGY 2 year in that the residents function as described previously under the PGY 2 year, include teaching conferences. The rotations however, are different and are as follows: 1. 2. 3. 4. 5. 6. 7. 8. Wake Med- 1 month UNC Internal Medicine Wards- 1-2 months Same Day Clinic- 1 month Ambulatory General Internal Medicine- 2-3 months Subspecialty Consultations 2-3 months Special electives – 1 month MICU or Cardiology- 1-month Night Float- 2-3 2 week blocks Inpatient General Internal Medicine Wards/ Inpatient Subspecialty Ward- The role of the PGY 3 resident is identical to that described previously for the PGY 2 resident. Same Day Clinic- The role of the PGY 3 resident is identical to that of the PGY 1 resident Ambulatory General Internal Medicine- PGY 3 residents can choose from several month blocks including those described for PGY 2 residents. There are additional choices as follows: General Medicine Consults/Hospitalist Service- PGY 3 residents see patients on other services, providing General Medicine Consultations. Also a small number of inpatients are cared for. Supervision is provided by faculty from the Division of General Internal Medicine Hospitalist group. Geriatric Medicine- PGY 3 residents are exposed to management of this population. Faculty trained in Geriatrics provide supervision Subspecialty Consultations- The role of the PGY 3 resident is the same as described for the PGY 2 resident on those rotations. Special Electives- These rotations are designed to enhance individual training. Residents pick a faculty mentor to conduct clinical or basic research. Rotations at other institutions or international rotations can also be done. COMPETENCY BASED CURRICULUM General Each inpatient service has designated teaching time, previously described in Section 1. It is the responsibility of the division faculty when on service to review a series of topics during the monthly rotation. The division faculty generates these topics with input from residents as well as data supplied to each division from preceding In-Training Examination. A dominant theme for these conferences is to review material a general internist must know about each discipline. The curricular goal for each resident is to have a working knowledge of these subjects. Cardiology Curriculum UNC Internal Medicine Training Program Cardiology Rotation Competency-based Goals and Objectives Teaching site: 3 Anderson Goals: The goal of this experience will be for the residents to gain experience in the inpatient evaluation and management of patients with a broad spectrum of cardiac diseases. 1. Objectives • Medical knowledge Describe the epidemiology, genetics, natural history, clinical expression of the cardiac diseases encountered in the inpatient setting. Describe structure and function of the cardiovascular system Summarize an approach to the evaluation of common cardiac presentations (chest pain, shock, failure) Distinguish non-cardiac chest pain from cardiac chest pain Interpret diagnostic tests used in the evaluation of inpatients with suspected cardiac disease, successfully risk stratify and treat Demonstrate ability to critically appraise and cite literature pertinent to the evaluation of inpatients with cardiac disorders. • Patient care Effectively perform a comprehensive history and complete physical examination in patients with cardiac symptoms Appropriately select and interpret laboratory, imaging, and pathologic studies used in the evaluation of cardiovascular disorders Gain experience in procedures including central and arterial line placement, swan ganz catheter indications and placement Construct a comprehensive treatment plan and assess response to therapy. Counsel patients concerning their diagnosis, planned diagnostic testing and recommended therapies. Utilize validated instruments in the assessment of pain, function, and quality of life to monitor and adjust therapy. • Practice-based learning and improvement Effectively use technology to manage information, support patient care decisions, and enhance both patient and physician education. Integrate and apply knowledge obtained from multiple sources to the care of inpatients Demonstrate ability to critically assess the scientific literature Set and assess individualized learning goals Analyze clinical experience and employ a systematic methodology for improvement Develop and maintain a willingness to learn from errors, and use errors to improve the system or processes of care • Systems-based practice Discuss how the health care system affects the management of inpatients with cardiac diseases. Demonstrate effective collaboration with other health care providers, including nursing staff, respiratory therapy, cardiac surgeons, and consult services in the care of patients with cardiac diseases Determine cost-effectiveness of alternative proposed interventions. Design cost-effective plans based on knowledge of best practices Demonstrate awareness of the impact of diagnostic and therapeutic recommendations on the health care system, cost of the procedure, insurance coverage, and resources utilized • Interpersonal skills and communication Apply empathy in all patient encounters Demonstrate effective skills of listening and speaking with patients, families and other members of the health care team Reliably and accurately communicate the patient's and his/her family's views and concerns to the attending Compose clear and timely admission and progress reports and interval notes/letters, including a precise diagnosis whenever possible, differential diagnosis when appropriate, and recommend follow up or additional studies Counsel patients, families and colleagues regarding side effects and appropriate use of specific medications, providing written documentation when appropriate • Professionalism Be prompt and prepared for rounds Recognize the importance of patient primacy, patient privacy, patient autonomy, informed consent, and equitable respect and care to all Respect patients and their families, staff and colleagues Model ethical behavior by reporting back to the attending and referring providers any key clinical findings, following through on clinical questions, laboratory testing and other patient care issues, and recognizing potential conflicts of interest Demonstrate integrity, honesty and openness in discussion of therapeutic options with patients and respect for patient’s preferences and multicultural differences Respond to phone calls, pages and/or messages in a timely manner Critical Care Curriculum UNC Internal Medicine Training Program Medical ICU Rotation Competency-based Goals and Objectives Teaching site: UNC Memorial Hospital Medical Intensive Care Unit Goals: The goal of this experience will be for the residents to gain experience in evaluation and management of patients requiring critical care medicine. 1. Objectives • Medical knowledge Describe the epidemiology, genetics, natural history, clinical presentation of conditions commonly treated in the intensive care unit Demonstrate knowledge of mechanical ventilation and demonstrate knowledge indications for initiation of mechanical ventilation and extubation. Demonstrate competency in evaluation of blood gases and ventilator management. Summarize an approach to the evaluation and treatment of common conditions treatied in the intensive care unit (sepsis, respiratory failure, drug overdoses) Demonstrate ability to critically appraise and cite literature pertinent to the evaluation of inpatients with critical illness. Demonstrate a knowledge of the indications for common procedures, and a competency in performing common procedures used in the intesive care unit, including central line placement, arterial line placement, thoracentesis, paracentesis, and lumbar puncture • Patient care Effectively perform a comprehensive history and complete physical examination in patients requiring treatment in the intensive care unit Appropriately select and interpret laboratory, imaging, and pathologic studies used in the evaluation Construct a comprehensive treatment plan and assess response to therapy. Counsel patients concerning their diagnosis, planned diagnostic testing and recommended therapies. Utilize validated instruments in the assessment of function and quality of life to monitor and adjust therapy. just therapy. • Practice-based learning and improvement Effectively use technology to manage information, support patient care decisions, and enhance both patient and physician education. Integrate and apply knowledge obtained from multiple sources to the care of ICU patients Demonstrate ability to critically assess the scientific literature Set and assess individualized learning goals Analyze clinical experience and employ a systematic methodology for improvement Develop and maintain a willingness to learn from errors, and use errors to improve the system or processes of care • Systems-based practice Discuss how the health care system affects the management of inpatients with endocrine diseases. Demonstrate effective collaboration with other health care providers, including nursing staff, diabetes educators, head and neck as well as neurosurgeons, and consult services in the care of patients with endocrine diseases Determine cost-effectiveness of alternative proposed interventions. Design cost-effective plans based on knowledge of best practices Demonstrate awareness of the impact of diagnostic and therapeutic recommendations on the health care system, cost of the procedure, insurance coverage, and resources utilized • Interpersonal skills and communication Apply empathy in all patient encounters Demonstrate effective skills of listening and speaking with patients, families and other members of the health care team Reliably and accurately communicate the patient's and his/her family's views and concerns to the attending Demonstrate competency in documentation including appropriate history and physical, progress, and discharge notes Counsel patients, families and colleagues regarding side effects and appropriate use of specific medications, providing written documentation when appropriate • Professionalism Be prompt and prepared for rounds and/or clinic Recognize the importance of patient primacy, patient privacy, patient autonomy, informed consent, and equitable respect and care to all Respect patients and their families, staff and colleagues Model ethical behavior by reporting back to the attending and referring providers any key clinical findings, following through on clinical questions, laboratory testing and other patient care issues, and recognizing potential conflicts of interest Demonstrate integrity, honesty and openness in discussion of therapeutic options with patients and respect for patient’s preferences and multicultural differences Respond to phone calls, pages and/or messages in a timely manner Core Topics in Critical Care Resuscitation BCLS and ACLS Shock: Causes, assessments, and treatment Early goal directed therapy for septic shock Pulmonary Respiratory failure: Hypoxemic and hypercapnic Intubation criteria, oral/nasal/tracheostomy complications Mechanical ventilator modes, monitors and complications Weaning criteria and techniques, daily spontaneous breathing trials ARDS: Causes, physiology, therapy and complications Asthma and COPD Pulmonary embolism Pulmonary hemorrhage Cardiology Shock: Differential diagnosis and initial treatment Acute MI: Diagnosis, treatment and complications Arrhythmias Pericarditis, Tamponade, and Constrictive pericarditis CHF and Pulmonary edema Pulmonary artery catheter: indications, placement, and interpretation Inotropic drugs Nephrology Acute renal failure: causes and treatment Renal replacement therapy: continuous and intermittent Electrolyte abnormalities: Na+,K+, C1Acid based disturbances and compensations Metabolic acidosis: increased and normal anion gap Urine electrolytes Metabolism Nutrition: assessment, requirements, enteral feeding, TPN Diabetic ketoacidosis and non-ketotic hyperosmolar coma Adrenal crisis and steroid therapy Gastrointestinal Upper GI hemorrhage Lower GI hemorrhage Liver disease: alcoholic, viral, other Pancreatitis The acute abdomen: causes and assessment Poisons Initial assessment and treatment options Acetaminophen Anti depressants Salicylates Alcohols Infections Pneumonias Aspiration pneumonitis Central line related bloodstream infections: prevention and management Tuberculosis Immunocompromised patients and opportunistic infections Hematology Anemia and transfusions Thrombocytopenia, coagulopathy DIC Hemolysis Sickle cell disease Administration and/Ethics Admission and discharge criteria Illness severity scores and prognoses Advance directives Use/limitation of life sustaining treatments Practice and system based improvements: protocols and data monitoring The Endocrine Rotation Residents will work on a daily basis with the endocrinology team to include an attending (Dr. O’Connell and/or Dr. DeCherney), an endocrine fellow, an endocrine nurse practitioner and possibly a diabetes educator during their rotation. Other attendings with special interest will be invited to rounds periodically when interesting cases are seen( i.e. Dr. Sharpless for interesting pituitary cases, Dr. Rubin for interesting bone cases, etc.) The resident will participate in the care of a wide variety of endocrine disorders seen in the hospital. Inpatient diabetes management will be a major focus. The residents will see patients one half day per week (usually Tuesday mornings, but days are flexible) in the endocrine outpatient clinic (High gate Specialty Center off of 54 near Southpoint) under the supervision of an attending. The residents will learn from their interactions with the team members, managing complex endocrine patients and from teaching while at the bedside. The endocrine curriculum will be provided and topics selected for teaching on a daily/weekly basis reflecting the patient material encountered. We will coordinate these teaching activities with the General Medicine Inpatient and Outpatient curriculum. Additionally, the residents should attend the Endocrine Division’s weekly conferences held Thursday afternoons from 3-5:30 in 2020 Bondurant. These sessions include a 3-4 pm didactic lecture given on an array of topics by attendings from multiple departments (nuclear medicine, pathology, ophthalmology, Endocrine, ect.) From 4-5 is journal club or a research presentation and from 5-5:30 is a case presentation by one of the fellows. The goal of the inpatient endocrine service is to improve care of admitted patients with endocrine disease. It is the hope of the Endocrine Division that the medicine residents will find this rotation an enjoyable and educational experience and that after the rotation, they will be better prepared to manage endocrine patients in both the inpatient and outpatient settings. Endocrinology Curriculum UNC Internal Medicine Training Program Endocrinology Rotation Competency-based Goals and Objectives Teaching site: Consult Service: UNC Memorial Hospital Clinic (1-2 half days per week): Highgate Subspecialty Clinic, 5316 Highgate Dr #125, Durham Goals: The goal of this experience will be for the residents to gain experience in both the inpatient and outpatient evaluation and management of patients with a broad spectrum of endocrine disorders. 1. Objectives • Medical knowledge Describe the epidemiology, genetics, natural history, clinical expression of the endocrine disorders encountered in the inpatient and outpatient setting. Describe function of the endocrine systems Summarize an approach to the evaluation of common endocrine presentations Interpret diagnostic tests used in the evaluation of in and outpatients with suspected endocrine disease Demonstrate ability to critically appraise and cite literature pertinent to the evaluation of inpatients with endocrine disorders. • Patient care Effectively perform a comprehensive history and complete physical examination in patients with endocrine symptoms Appropriately select and interpret laboratory, imaging, and pathologic studies used in the evaluation of endocrine disorders Construct a comprehensive treatment plan and assess response to therapy. Counsel patients concerning their diagnosis, planned diagnostic testing and recommended therapies. Utilize validated instruments in the assessment of function and quality of life to monitor and adjust therapy. • Practice-based learning and improvement Effectively use technology to manage information, support patient care decisions, and enhance both patient and physician education. Integrate and apply knowledge obtained from multiple sources to the care of inpatients and outpatients Demonstrate ability to critically assess the scientific literature Set and assess individualized learning goals Analyze clinical experience and employ a systematic methodology for improvement Develop and maintain a willingness to learn from errors, and use errors to improve the system or processes of care • Systems-based practice Discuss how the health care system affects the management of inpatients with endocrine diseases. Demonstrate effective collaboration with other health care providers, including nursing staff, diabetes educators, head and neck as well as neurosurgeons, and consult services in the care of patients with endocrine diseases Determine cost-effectiveness of alternative proposed interventions. Design cost-effective plans based on knowledge of best practices Demonstrate awareness of the impact of diagnostic and therapeutic recommendations on the health care system, cost of the procedure, insurance coverage, and resources utilized • Interpersonal skills and communication Apply empathy in all patient encounters Demonstrate effective skills of listening and speaking with patients, families and other members of the health care team Reliably and accurately communicate the patient's and his/her family's views and concerns to the attending Compose clear and timely consult and clinic notes as well as interval notes/letters, including a precise diagnosis whenever possible, differential diagnosis when appropriate, and recommend follow up or additional studies Counsel patients, families and colleagues regarding side effects and appropriate use of specific medications, providing written documentation when appropriate • Professionalism Be prompt and prepared for rounds and/or clinic Recognize the importance of patient primacy, patient privacy, patient autonomy, informed consent, and equitable respect and care to all Respect patients and their families, staff and colleagues Model ethical behavior by reporting back to the attending and referring providers any key clinical findings, following through on clinical questions, laboratory testing and other patient care issues, and recognizing potential conflicts of interest Demonstrate integrity, honesty and openness in discussion of therapeutic options with patients and respect for patient’s preferences and multicultural differences Respond to phone calls, pages and/or messages in a timely manner Goals and Objectives When possible, residents should participate in the care of patients with the following disorders. Reading should be geared towards patients encountered as well as disorders missed while on rotation. At the close of the endocrine rotation, residents should exhibit proficiency in the evaluation and treatment of the disorders listed in the curriculum below. 1. Diabetes Mellitus Diagnosis and Classification Treatment Complications Hypoglycemia in Non-diabetics 2. Disorders of the Pituitary Gland Hypothalamic Disease Hypopituitarism Pituitary Tumors Posterior Pituitary Deficiency and Excess Pregnancy and Pituitary Disease 3. Disorders of the Thyroid Gland Thyroid Physiology Evaluation of Thyroid Function Functional Thyroid Gland Disorders Structural Diseases of the Thyroid Gland Approach to the Thyroid Nodule Medications that alter thyroid function Effects of Non-Thyroidal Illness on Thyroid Function Tests Thyroid Function and Disease in Pregnancy Thyroid Emergencies 4. Disorders of the Adrenal Gland Adrenal Insufficiency Cushing Syndrome Adrenal Incidentaloma Pheochromocytoma Primary Hypoaldosteronism Adrenocortical Carcinoma 5. Reproductive Disorders Basic Concepts and Common Features Physiology of Male Reproduction Female Reproductive Physiology 6. Calcium and Bone Disorders Calcium Metabolism Hypercalcemia Hypocalcemia Metabolic Bone Disease Gastroenterology Curriculum UNC Internal Medicine Training Program Gastroenterology Rotation Competency-based Goals and Objectives Teaching site: UNC Memorial Hospital Instructions: Following morning report on your first day on service, page the fellow on call for your consult service (Luminal or Hepatology). Tell them the days that you will be on service and which days you have clinic or alternate coverage responsibilities. Goals: The goal of this experience will be for the residents to gain experience in the inpatient evaluation and management of patients with a broad spectrum of GI diseases. 1. Objectives • Medical knowledge Describe the epidemiology, genetics, natural history, clinical expression of the GI illness encountered in the inpatient setting. Describe structure and function of GI tract, liver and biliary systems Summarize an approach to the evaluation of the common presentations of GI illness (GI bleed, diarrhea, jaundice / transaminitis, etc) Distinguish patients with functional bowel disorders from those with other "organic" bowel diseases Interpret diagnostic tests used in the evaluation of outpatients with suspected GI Illness Demonstrate ability to critically appraise and cite literature pertinent to the evaluation of outpatients with GI disorders. • Patient care Effectively perform a comprehensive history and complete physical examination in patients with GI symptoms, abnormal liver function tests, or acute or chronic GI disorders Construct an appropriate differential diagnosis Appropriately select and interpret laboratory, imaging, and pathologic studies used in the evaluation of GI disorders Construct a comprehensive treatment plan and assess response to therapy. Counsel patients concerning their diagnosis, planned diagnostic testing and recommended therapies. Describe the appropriate use of validated instruments in the assessment of pain, function, and quality of life to monitor and adjust therapy. • Practice-based learning and improvement Effectively use technology to manage information, support patient care decisions, and enhance both patient and physician education. Integrate and apply knowledge obtained from multiple sources to the care of inpatients Demonstrate ability to critically assess the scientific literature Set and assess individualized learning goals Analyze clinical experience and employ a systematic methodology for improvement Develop and maintain a willingness to learn from errors, and use errors to improve the system or processes of care • Systems-based practice Discuss how the health care system affects the management of outpatients with GI diseases. Demonstrate effective collaboration with other health care providers, including nutritionists and GI surgeons, in the care of patients with GI illness Determine cost-effectiveness of alternative proposed interventions. Design cost-effective plans based on knowledge of best practices Demonstrate awareness of the impact of diagnostic and therapeutic recommendations on the health care system, cost of the procedure, insurance coverage, and resources utilized • Interpersonal skills and communication Approach patients with an empathetic and understandable manner Demonstrate effective skills of listening and speaking with patients, families and other members of the health care team Reliably and accurately communicate the patient's and his/her family's views and concerns to the attending Compose clear and timely consultation reports and interval notes/letters, including a precise diagnosis whenever possible, differential diagnosis when appropriate, and recommend follow up or additional studies Counsel patients, families and colleagues regarding side effects and appropriate use of specific medications, providing written documentation when appropriate • Professionalism Exhibit punctuality for all assigned duties Incorporate the principles of patient primacy, patient privacy, patient autonomy, informed consent, and equitable respect in the care of patients Demonstrate respect for patients and their families, staff and colleagues Model ethical behavior by reporting back to the attending and referring providers key clinical findings, following through on clinical questions, laboratory testing and other patient care issues, and recognizing potential conflicts of interest Demonstrate integrity, honesty and openness in discussion of therapeutic options with patients and respect for patient’s preferences and multicultural differences Respond to phone calls, pages and/or messages in a timely manner GI Core Topics 1. Evaluation and treatment of diarrhea 2. Evaluation and treatment of jaundice 3. Inflammatory bowel diseases 4. Hepatitis - viral and non-viral 5. Diagnosis and management of peptic ulcer disease 6. Nutritional support - enteral and intravenous 7. Colonoscopy - indication and screening 8. Diagnosis and management of pancreatitis 9. Diagnosis of esophageal motility disorders 10. Evaluation and treatment of abdominal pain 11. Diagnosis and management of cirrhosis 12. Liver transplantation - indicators and outcomes 13. Diagnosis and management of GI bleeding 14. Appropriate use of radiologic studies of the gastrointestinal system 15. Evaluation and management of gallstones/gallbladder diseases General Medicine Curriculum UNC Internal Medicine Training Program General Medicine Rotation Competency-based Goals and Objectives Teaching site: UNC Memorial Hospital (Ward Teams U and W) Goals: The goal of this experience will be for the residents to gain experience in the inpatient and outpatient evaluation and management of patients with a broad spectrum of general medicine disorders. 1. Objectives • Medical knowledge Become familiar with the epidemiology, diagnosis, and management of patients with common medical conditions encountered on a general medicine service Demonstrate competence in performing common procedures use on a general medicine service, including paracentesis, thoracentesis, and lumbar puncture Demonstrate ability to critically appraise and cite literature pertinent to the evaluation of inpatients on a general medicine ward service • Patient care Effectively perform a comprehensive history and complete physical examination Appropriately select and interpret laboratory, imaging, and pathologic studies used in the evaluation of patients on a general medicine ward service Construct a comprehensive treatment plan and assess response to therapy Counsel patients concerning their diagnosis, planned diagnostic testing and recommended therapies. Utilize validated instruments in the assessment of function and quality of life to monitor and adjust therapy Demonstrate competency in documentation including appropriate history and physical, progress, and discharge notes • Practice-based learning and improvement Effectively use technology to manage information, support patient care decisions, and enhance both patient and physician education. Integrate and apply knowledge obtained from multiple sources to the care of inpatients and outpatients Demonstrate ability to critically assess the scientific literature Set and assess individualized learning goals Analyze clinical experience and employ a systematic methodology for improvement Develop and maintain a willingness to learn from errors, and use errors to improve the system or processes of care • Systems-based practice Describe how the health care system affects the management of inpatients on a general medicine service Demonstrate effective collaboration with other health care providers, particularly subspecialty consultants Determine cost-effectiveness of alternative proposed interventions. Design cost-effective plans based on knowledge of best practices Demonstrate awareness of the impact of diagnostic and therapeutic recommendations on the health care system, cost of the procedure, insurance coverage, and resources utilized • Interpersonal skills and communication Apply empathy in all patient encounters Demonstrate effective skills of listening and speaking with patients, families and other members of the health care team Reliably and accurately communicate the patient's and his/her family's views and concerns to the attending Counsel patients, families and colleagues regarding side effects and appropriate use of specific medications, providing written documentation when appropriate • Professionalism Be prompt and prepared for rounds and/or clinic Recognize the importance of patient primacy, patient privacy, patient autonomy, informed consent, and equitable respect and care to all Respect patients and their families, staff and colleagues Model ethical behavior by reporting back to the attending and referring providers any key clinical findings, following through on clinical questions, laboratory testing and other patient care issues, and recognizing potential conflicts of interest Demonstrate integrity, honesty and openness in discussion of therapeutic options with patients and respect for patient’s preferences and multicultural differences Respond to phone calls, pages and/or messages in a timely manner General Medicine Core Topics Likelihood Ratios; testing Community Acquired Pneumonia Pulmonary Emboli Chest Pain Evaluation; CAD Diabetic ketoacidosis, complications Meningitis Venous Stasis Ulcers Peripheral Vascular Disease W/U of Diarrhea COPD, acute exacerbation Depression, mood disorders Stroke, endarterectomy Hypertension Emergencies Common Biliary tract diseases, cholecystitis, cholangitis Dementia Delirium Diverticulitis Avitaminoses Peripheral Neuropathy Cellulitis Pulmonary Nodule Anemia of chronic disease, liver disease Pancreatitis Poisonings- ethylene glycol, arsenic Geriatrics Geriatrics Curriculum for Internal Medicine Residency Program Updated 7/2011 Debra L. Bynum, MD Program Director, Geriatric Fellowship Assistant Director for Education, Geriatric Division of Medicine Current requirements from the Residency Review Committee for Internal Medicine, as outlined by the Accreditation Council for Graduate Medical Education, specify that “Residents must have formal instruction and assigned clinical experience in geriatric medicine. The curriculum and clinical experience should be directed by an ABMS- certified geriatrician. These experiences may occur at one or more specifically designated geriatric inpatient units, geriatric consultation services, long-term facilities, geriatric ambulatory clinics,, and/ or in home care settings.” The Department of Medicine at the University of North Carolina at Chapel Hill currently has a separate Division of Geriatric Medicine with faculty and fellows in graduate medical training who are dedicated to the education of medical students and residents. Currently residents receive training in the care of geriatric patients in both inpatient and outpatient settings. In addition to the core competencies of training as defined for all Internal Medicine Residents by the ACGME, the American Geriatrics Society in working with the American Medical Association, the American Board of Family Medicine, and the Society of General Internal Medicine have developed a set of 26 geriatric competencies in 7 domains (Transitions of Care; Hospital Patient Safety; Cognitive, Affective and Behavioral Health; Complex or Chronic Illness; Medication Management; Ambulatory Care; and Palliative and End of Life Care). MINIMUM GERIATRIC COMPETENCIES for IM-FM Residents The graduating IM or FM resident, in the context of a specific older patient scenario (real or simulated), must be able to: MEDICATION MANAGEMENT 1 Prescribe appropriate drugs and dosages considering: (a) age-related changes in renal and hepatic function, body composition, and CNS sensitivity; (b) common side effects in light of patient’s comorbidities, functional status, and other medications; and (c) drug-drug interactions. 2 When prescribing drugs which present high risk for adverse events and interactions (these medications include, but are not limited to, coumadin, NSAID’s, opioids, digoxin, insulin, strongly anticholinergic drugs, and psychotropic drugs), discuss and document the rationale for their use, alternatives, and ways to decrease side effects. 3 Periodically review patient’s medications (including meds prescribed by other physicians, OTC and CAM) with the patient and/or caregiver to assess adherence, eliminate ineffective, duplicate and unnecessary medications, and assure that all medically indicated pharmacotherapy is prescribed. COGNITIVE, AFFECTIVE, AND BEHAVIORAL HEALTH 4 Appropriately administer and interpret the results of at least one validated screening tool for each of the following: delirium, dementia, depression, and substance abuse. 5 Recognize delirium as a medical urgency, promptly evaluate and treat underlying problem. 6 Evaluate and formulate a differential diagnosis and workup for patients with changes in affect, cognition, and behavior (agitation, psychosis, anxiety, apathy). 7 In patients with dementia and/or depression, initiate treatment and/or refer as appropriate. COMPLEX OR CHRONIC ILLNESS(ES) IN OLDER ADULTS 8 Identify and assess barriers to communication such as hearing and/or sight impairments, speech difficulties, aphasia, limited health literacy, and cognitive disorders. When present, demonstrate ability to use adaptive equipment and alternative methods to communicate (e.g., with the aid of family/friend, caregiver). 9 Determine whether an older patient has sufficient capacity to give an accurate history, make decisions and participate in developing the plan of care. 10 In evaluating adults with undifferentiated illness, generate differential diagnoses that include diseases that often present atypically in older adults (e.g., acute coronary syndromes, the acute abdomen, urinary tract infection, and pneumonia). 11 Consider adverse reactions to medication in the differential diagnosis of new symptoms or geriatric syndromes (e.g., cognitive impairment, constipation, falls, incontinence). 12 Demonstrate understanding of the major age-related changes in physical and laboratory findings during diagnostic reasoning (e.g., S4 does not reflect CHF, pulse increase less common with orthostasis, pO2 declines with age, abdominal pain may be less severe). 13 Discuss and document advance care planning and goals of care with all patients with chronic or complex illness, and/or their surrogates. 14 Develop a treatment plan that incorporates the patient’s and family’s goals of care, preserves function, and relieves symptoms. PALLIATIVE AND END OF LIFE CARE 15 In patients with life limiting or severe chronic illness, assess pain and distressing non-pain symptoms (dyspnea, nausea, vomiting, fatigue) at regular intervals and institute appropriate treatment based on their goals of care. 16 In patients with life limiting or severe chronic illness, identify with the patient, family and care team when goals of care and management should transition to primarily comfort care. HOSPITAL PATIENT SAFETY 17 As part of the daily physical exam of all hospitalized older patients, assess and document whether delirium is present. 18 In hospitalized medical and surgical patients, evaluate - on admission and on a regular basis - for fall risk, immobility, pressure ulcers, adequacy of oral intake, pain, new urinary incontinence, constipation, and inappropriate medication prescribing, and institute appropriate corrective measures. 19 In hospitalized patients with an indwelling bladder catheter, discontinue or document indication for use. 20 Before using or renewing physical or chemical restraints on geriatric patients, assess for and treat reversible causes of agitation (e.g., use of irritating tethers [including monitor leads, blood pressure cuff, pulse oximeter, intravenous lines and in-dwelling bladder catheters], untreated pain, alcohol withdrawal, delirium, ambient noise). Consider alternatives to restraints such as additional staffing, environmental modifications, and presence of family members. TRANSITIONS OF CARE 21 In planning hospital discharge, work in conjunction with other health care providers (e.g., social work, case management, nursing, physical therapy) to recommend appropriate services based on: the clinical needs, personal values and social and financial resources of the patients and their families (e.g., symptom and functional goals in the context of prognosis, care directives, home circumstances and financial resources); and the patient’s eligibility for community-based services (e.g., home health care, day care, assisted living, nursing home, rehabilitation, or hospice). 22 In transfers between the hospital and skilled nursing or extended care facilities, ensure that: for transfers to the hospital: the caretaking team has correct information on the acute events necessitating transfer, goals of transfer, medical history, medications, allergies, baseline cognitive and functional status, advance care plan and responsible PCP; and for transfers from the hospital: a written summary of hospital course be completed and transmitted to the patient and/or family caregivers as well as the receiving health care providers that accurately and concisely communicates evaluation and management, clinical status, discharge medications, current cognitive and functional status, advance directives, plan of care, scheduled or needed follow-up, and hospital physician contact information. AMBULATORY CARE 23 Yearly screen all ambulatory elders for falls or fear of falling. If positive, assess gait and balance instability, evaluate for potentially precipitating causes (medications, neuromuscular conditions, and medical illness), and implement interventions to decrease risk of falling. 24 Detect, evaluate and initiate management of bowel and bladder dysfunction in community dwelling older adults. 25 Identify older persons at high safety risk, including unsafe driving or elder abuse/neglect, and develop a plan for assessment or referral. 26 Individualize standard recommendations for screening tests and chemoprophylaxis in older patients based on life expectancy, functional status, patient preference and goals of care. Residents will work either on the Inpatient Medicine Service or in the Outpatient setting in order to achieve these competencies. During the Outpatient rotation, residents will work in the Geriatric Evaluation Clinic, Hospice/home visits, PMR, Geriatric Psychiatry, and Long Term Care settings. In addition to patient care activities that are under the direct supervision of a Geriatric Faculty member, the residents will be part of routine didactic sessions and have full access to our presentations and other resources available through the Fellowship Web site. Readings and other materials and resources can be found: http://www.med.unc.edu/aging/fellowship References: Williams B C, Warshaw G, Fabiny A R, Lundebjerg N, Sauvigne K, Schwartzberg J G, Leipzig R M. (2010). Medicine in the 21st century: Recommended essential geriatrics competencies for Internal Medicine and Family Medicine residents. Journal of Graduate Medical Education, 2(3), 373-383. Also available Hematology / "Coags" Curriculum UNC Internal Medicine Training Program Hematology Rotation Competency-based Goals and Objectives Teaching site: UNC Memorial Hospital Instructions: Following morning report on your first day on service, page the fellow on call for your consult service. Tell them the days that you will be on service and which days you have clinic or alternate coverage responsibilities. Goals: The goal of this experience will be for the residents to gain experience in the inpatient evaluation and management of patients with a broad spectrum of hematologic diseases. 1. Objectives • Medical knowledge Describe the epidemiology, genetics, natural history, clinical expression of the hematologic illness encountered in the inpatient setting. Describe the functions and interplay of factors related to hemostasis and bleeding Summarize an approach to the evaluation of the common presentations of hematologic illnesses (bleeding, clotting, cytopenias, etc) Interpret diagnostic tests used in the evaluation of inpatients with suspected hematologic disorders Demonstrate ability to critically appraise and cite literature pertinent to the evaluation of inpatients with hematologic disorders • Patient care Effectively perform a comprehensive history and complete physical examination in patients with hematologic symptoms, abnormal coagulation tests, or acute or chronic hematologic disorders Construct an appropriate differential diagnosis Appropriately select and interpret laboratory, imaging, and pathologic studies used in the evaluation of hematologic disorders Construct a comprehensive treatment plan and assess response to therapy. Counsel patients concerning their diagnosis, planned diagnostic testing and recommended therapies. Describe the appropriate use of validated instruments in the assessment of pain, function, and quality of life to monitor and adjust therapy. • Practice-based learning and improvement Effectively use technology to manage information, support patient care decisions, and enhance both patient and physician education. Integrate and apply knowledge obtained from multiple sources to the care of inpatients Demonstrate ability to critically assess the scientific literature Set and assess individualized learning goals Analyze clinical experience and employ a systematic methodology for improvement Develop and maintain a willingness to learn from errors, and use errors to improve the system or processes of care • Systems-based practice Discuss how the health care system affects the management of outpatients with hematologic disorders Demonstrate effective collaboration with other health care providers, including nursing, counselors and transfusion medicine, in the care of patients with hematologic disorders Determine cost-effectiveness of alternative proposed interventions. Design cost-effective plans based on knowledge of best practices Demonstrate awareness of the impact of diagnostic and therapeutic recommendations on the health care system, cost of the procedure, insurance coverage, and resources utilized • Interpersonal skills and communication Approach patients with an empathetic and understandable manner Demonstrate effective skills of listening and speaking with patients, families and other members of the health care team Reliably and accurately communicate the patient's and his/her family's views and concerns to the attending Compose clear and timely consultation reports and interval notes/letters, including a precise diagnosis whenever possible, differential diagnosis when appropriate, and recommend follow up or additional studies Counsel patients, families and colleagues regarding side effects and appropriate use of specific medications, providing written documentation when appropriate • Professionalism Exhibit punctuality for all assigned duties Incorporate the principles of patient primacy, patient privacy, patient autonomy, informed consent, and equitable respect in the care of patients Demonstrate respect for patients and their families, staff and colleagues Model ethical behavior by reporting back to the attending and referring providers key clinical findings, following through on clinical questions, laboratory testing and other patient care issues, and recognizing potential conflicts of interest Demonstrate integrity, honesty and openness in discussion of therapeutic options with patients and respect for patient’s preferences and multicultural differences Respond to phone calls, pages and/or messages in a timely manner Infectious Disease Curriculum UNC Internal Medicine Training Program Infectious Disease Rotation Competency-based Goals and Objectives Teaching site: UNC Memorial Hospital Instructions: Following morning report on your first day on service, page the fellow on call for your consult service. Tell them the days that you will be on service and which days you have clinic or alternate coverage responsibilities. Goals: The goal of this experience will be for the residents to gain experience in the inpatient evaluation and management of patients with a broad spectrum of infectious diseases. 1. Objectives • Medical knowledge Describe the epidemiology, genetics, natural history, clinical expression of the infectious diseases encountered in the inpatient setting. Describe the functions and interplay of factors related to host defense, microbial infection and treatment Summarize an approach to the evaluation of the common presentations of infectious diseases (HIV, pneumonia, urinary tract infections, sepsis, etc) Interpret diagnostic tests used in the evaluation of inpatients with suspected infectious diseases Demonstrate ability to critically appraise and cite literature pertinent to the evaluation of inpatients with infectious diseases • Patient care Effectively perform a comprehensive history and complete physical examination in patients with infectious symptoms or chronic infectious disease states Construct an appropriate differential diagnosis Appropriately select and interpret laboratory, imaging, and pathologic studies used in the evaluation of infectious diseases Construct a comprehensive treatment plan and assess response to therapy. Counsel patients concerning their diagnosis, planned diagnostic testing and recommended therapies. Describe the appropriate use of validated instruments in the assessment of pain, function, and quality of life to monitor and adjust therapy. • Practice-based learning and improvement Effectively use technology to manage information, support patient care decisions, and enhance both patient and physician education. Integrate and apply knowledge obtained from multiple sources to the care of inpatients Demonstrate ability to critically assess the scientific literature Set and assess individualized learning goals Analyze clinical experience and employ a systematic methodology for improvement Develop and maintain a willingness to learn from errors, and use errors to improve the system or processes of care • Systems-based practice Discuss how the health care system affects the management of outpatients with infectious diseases Demonstrate effective collaboration with other health care providers, including nursing, counselors and the Department of Health, in the care of patients with infectious diseases Determine cost-effectiveness of alternative proposed interventions. Design cost-effective plans based on knowledge of best practices Demonstrate awareness of the impact of diagnostic and therapeutic recommendations on the health care system, cost of the procedure, insurance coverage, and resources utilized • Interpersonal skills and communication Approach patients with an empathetic and understandable manner Demonstrate effective skills of listening and speaking with patients, families and other members of the health care team Reliably and accurately communicate the patient's and his/her family's views and concerns to the attending Compose clear and timely consultation reports and interval notes/letters, including a precise diagnosis whenever possible, differential diagnosis when appropriate, and recommend follow up or additional studies Counsel patients, families and colleagues regarding side effects and appropriate use of specific medications, providing written documentation when appropriate • Professionalism Exhibit punctuality for all assigned duties Incorporate the principles of patient primacy, patient privacy, patient autonomy, informed consent, and equitable respect in the care of patients Demonstrate respect for patients and their families, staff and colleagues Model ethical behavior by reporting back to the attending and referring providers key clinical findings, following through on clinical questions, laboratory testing and other patient care issues, and recognizing potential conflicts of interest Demonstrate integrity, honesty and openness in discussion of therapeutic options with patients and respect for patient’s preferences and multicultural differences Respond to phone calls, pages and/or messages in a timely manner Infectious Disease Core Topics Antibiotics I ( antibacterials) Antibiotics II ( antivirals and antifungals) HIV I HIV II Sepsis Endocarditis Skin and Soft Tissue Infection (Including osteomyelitits) Diarrhea Urinary Tract Infection FUO New and unusual infections, including Lyme disease and RMSF Oncology Curriculum UNC Internal Medicine Training Program Oncology Rotation Competency-based Goals and Objectives Inpatient Teaching site: UNC Cancer Hospital, 4th Floor Inpatient Unit Goals: The goal of this experience will be for the residents to gain experience in the inpatient setting and treatment of patients with a broad spectrum of cancers. 1. Objectives • Medical knowledge Describe the epidemiology, genetics, natural history, clinical expression of different types of cancers encountered in the inpatient setting. Summarize an approach to the evaluation of common cancer presentations Exhibit understanding of the epidemiology, pathology, clinical presentation, diagnosis and treatment of common complications of cancer, chemotherapy and radiation therapy, including but not limited to tumor lysis syndrome, leukostasis, cord compression, neutropenic fevers and pain crises. Interpret diagnostic tests used in the evaluation of inpatients with suspected cancer Demonstrate ability to critically appraise and cite literature pertinent to the evaluation of inpatients with cancer. • Patient care Effectively perform a comprehensive history and complete physical examination in patients with cancer and/or its complications Appropriately select and interpret laboratory, imaging, and pathologic studies used in the evaluation of cancer and/or its complications Construct a comprehensive treatment plan and assess response to therapy. Counsel patients concerning their diagnosis, planned diagnostic testing and recommended therapies. Utilize validated instruments in the assessment of function and quality of life to monitor and adjust therapy. • Practice-based learning and improvement Effectively use technology to manage information, support patient care decisions, and enhance both patient and physician education. Integrate and apply knowledge obtained from multiple sources to the care of inpatients Demonstrate ability to critically assess the scientific literature Set and assess individualized learning goals Analyze clinical experience and employ a systematic methodology for improvement Develop and maintain a willingness to learn from errors, and use errors to improve the system or processes of care • Systems-based practice Discuss how the health care system affects the management of inpatients with endocrine diseases. Demonstrate effective collaboration with other health care providers, including nursing staff, therapists, counselors, surgeons, and consult services in the care of patients with cancer Determine cost-effectiveness of alternative proposed interventions. Design cost-effective plans based on knowledge of best practices Demonstrate awareness of the impact of diagnostic and therapeutic recommendations on the health care system, cost of the procedure, insurance coverage, and resources utilized • Interpersonal skills and communication Apply empathy in all patient encounters Demonstrate effective skills of listening and speaking with patients, families and other members of the health care team Reliably and accurately communicate the patient's and his/her family's views and concerns to the attending Compose clear and timely consult and clinic notes as well as interval notes/letters, including a precise diagnosis whenever possible, differential diagnosis when appropriate, and recommend follow up or additional studies Counsel patients, families and colleagues regarding side effects and appropriate use of specific medications, providing written documentation when appropriate • Professionalism Be prompt and prepared for rounds and/or clinic Recognize the importance of patient primacy, patient privacy, patient autonomy, informed consent, and equitable respect and care to all Respect patients and their families, staff and colleagues Model ethical behavior by reporting back to the attending and referring providers any key clinical findings, following through on clinical questions, laboratory testing and other patient care issues, and recognizing potential conflicts of interest Demonstrate integrity, honesty and openness in discussion of therapeutic options with patients and respect for patient’s preferences and multicultural differences Respond to phone calls, pages and/or messages in a timely manner Pulmonary Curriculum UNC Internal Medicine Training Program Pulmonary Rotation Competency-based Goals and Objectives Teaching site: Consults: UNC Memorial Hospital Clinic: ACC Building Goals: The goal of this experience will be for the residents to gain experience in the inpatient evaluation and management of patients with a broad spectrum of pulmonary diseases. 1. Objectives • Medical knowledge Describe the epidemiology, genetics, natural history, clinical expression of the pulmonary disorders encountered in the inpatient and outpatient setting. Demonstrate competenence in performing common procedures use on a general medicine service, including paracentesis, thoracentesis, and lumbar puncture Summarize an approach to the evaluation of common pulmonary disease presentations Interpret diagnostic tests used in the evaluation of inpatients with suspected pulmonary disease Demonstrate ability to critically appraise and cite literature pertinent to the evaluation of inpatients (outpatients on the clinic rotation) with pulmonary diseases. • Patient care Effectively perform a comprehensive history and complete physical examination in patients with respiratory symptoms or known pulmonary diseases Appropriately select and interpret laboratory, imaging, and pathologic studies used in the evaluation of pulmonary diseases Construct a comprehensive treatment plan and assess response to therapy. Counsel patients concerning their diagnosis, planned diagnostic testing and recommended therapies. Utilize validated instruments in the assessment of function and quality of life to monitor and adjust therapy. • Practice-based learning and improvement Effectively use technology to manage information, support patient care decisions, and enhance both patient and physician education. Integrate and apply knowledge obtained from multiple sources to the care of inpatients with pulmonary diseases Demonstrate ability to critically assess the scientific literature Set and assess individualized learning goals Analyze clinical experience and employ a systematic methodology for improvement Develop and maintain a willingness to learn from errors, and use errors to improve the system or processes of care • Systems-based practice Discuss how the health care system affects the management of inpatients with pulmonary diseases. Demonstrate effective collaboration with other health care providers Determine cost-effectiveness of alternative proposed interventions. Design cost-effective plans based on knowledge of best practices Demonstrate awareness of the impact of diagnostic and therapeutic recommendations on the health care system, cost of the procedure, insurance coverage, and resources utilized • Interpersonal skills and communication Apply empathy in all patient encounters Demonstrate effective skills of listening and speaking with patients, families and other members of the health care team Reliably and accurately communicate the patient's and his/her family's views and concerns to the attending Demonstrate competency in documentation including appropriate history and physical, progress, and discharge notes Counsel patients, families and colleagues regarding side effects and appropriate use of specific medications, providing written documentation when appropriate • Professionalism Be prompt and prepared for rounds and/or clinic Recognize the importance of patient primacy, patient privacy, patient autonomy, informed consent, and equitable respect and care to all Respect patients and their families, staff and colleagues Model ethical behavior by reporting back to the attending and referring providers any key clinical findings, following through on clinical questions, laboratory testing and other patient care issues, and recognizing potential conflicts of interest Demonstrate integrity, honesty and openness in discussion of therapeutic options with patients and respect for patient’s preferences and multicultural differences Respond to phone calls, pages and/or messages in a timely manner Pulmonary Core Topics 1. Pulmonary Physiology a. Gas exchange b. Mechanics c. Measures of function i. Arterial blood gases ii. Lung volumes and DLCO iii. Imaging techniques 2. Obstructive Pulmonary ( Airway) Disease a. Chronic Bronchitis b. Emphysema i. Centrilbular ii. Panacinar c. Cystic Fibrosis d. Bronchiolitis i. Bronchiolitis obliterans ii. BOOP iii. Bronchiolitis obliterans associated with lung transplantation e. Bronchiectasis 3. Asthma a. Epidemiology and definition b. Classification i. “Intrinsic or nonallergic” ii. “Extrinsic or allergic” c. Pathogenesis d. Clinical manifestations and diagnosis e. Therapy 4. Respiratory Infections a. Community acquired pneumonias b. Infections in the immuncomprimised host i. . AIDS ii. Other causes of immunosuppression c. Tuberculosis and nontuberculous mycobacteria d. Anaerobic lung infections and aspiration e. Empyema 5. Interstitial Lung Disease a. Idiopathic pulmonary fibrosis b. Drug induced c. Connective tissue disease d. Sarcoidosis e. Esoinophillic granuloma 6. Lung Neoplasma a. Carcinomas b. Mesotheliomas c. Benign tumors d. Staging evaluation e. Resectability 7. Lung transplantation a. Indications b. Common diseases transplanted c. Single versus double lung transplants d. Survival e. Complications 8. Pulmonary Vascular Sisease a. Pulmonary thromboemboli b. Pulmonary hypertension c. Pulmonary vasculitits d. Alveolar hemorrhage/hemoptysis 9. Miscellaneous a. Pleural disease i. Effusions ii. Pneumothorax b. Occupational Lung disease c. Sleep disorders d. Lymphangioleiomyomatosis Nephrology Curriculum UNC Internal Medicine Training Program Nephrology Rotation Competency-based Goals and Objectives Teaching site: UNC Memorial Hospital Instructions: Following morning report on your first day on service, page the fellow on call for your consult service. Tell them the days that you will be on service and which days you have clinic or alternate coverage responsibilities. Goals: The goal of this experience will be for the residents to gain experience in the inpatient evaluation and management of patients with a broad spectrum of renal disorders. 1. Objectives • Medical knowledge Describe the epidemiology, genetics, natural history, clinical expression of the renal disorders encountered in the inpatient setting. Describe the structure and function of the kidneys Summarize an approach to the evaluation of the common presentations of renal disorders Interpret diagnostic tests used in the evaluation of inpatients with suspected renal disorders Demonstrate ability to critically appraise and cite literature pertinent to the evaluation of inpatients with renal disorders • Patient care Effectively perform a comprehensive history and complete physical examination in patients with renal symptoms, abnormal creatinine clearnce, or acute or chronic renal disorders Construct an appropriate differential diagnosis Appropriately select and interpret laboratory, imaging, and pathologic studies used in the evaluation of renal disorders Construct a comprehensive treatment plan and assess response to therapy. Counsel patients concerning their diagnosis, planned diagnostic testing and recommended therapies. Describe the appropriate use of validated instruments in the assessment of pain, function, and quality of life to monitor and adjust therapy. • Practice-based learning and improvement Effectively use technology to manage information, support patient care decisions, and enhance both patient and physician education. Integrate and apply knowledge obtained from multiple sources to the care of inpatients Demonstrate ability to critically assess the scientific literature Set and assess individualized learning goals Analyze clinical experience and employ a systematic methodology for improvement Develop and maintain a willingness to learn from errors, and use errors to improve the system or processes of care • Systems-based practice Discuss how the health care system affects the management of outpatients with renal disorders Demonstrate effective collaboration with other health care providers, including nursing, counselors and dialysis centers, in the care of patients with renal disorders Determine cost-effectiveness of alternative proposed interventions. Design cost-effective plans based on knowledge of best practices Demonstrate awareness of the impact of diagnostic and therapeutic recommendations on the health care system, cost of the procedure, insurance coverage, and resources utilized • Interpersonal skills and communication Approach patients with an empathetic and understandable manner Demonstrate effective skills of listening and speaking with patients, families and other members of the health care team Reliably and accurately communicate the patient's and his/her family's views and concerns to the attending Compose clear and timely consultation reports and interval notes/letters, including a precise diagnosis whenever possible, differential diagnosis when appropriate, and recommend follow up or additional studies Counsel patients, families and colleagues regarding side effects and appropriate use of specific medications, providing written documentation when appropriate • Professionalism Exhibit punctuality for all assigned duties Incorporate the principles of patient primacy, patient privacy, patient autonomy, informed consent, and equitable respect in the care of patients Demonstrate respect for patients and their families, staff and colleagues Model ethical behavior by reporting back to the attending and referring providers key clinical findings, following through on clinical questions, laboratory testing and other patient care issues, and recognizing potential conflicts of interest Demonstrate integrity, honesty and openness in discussion of therapeutic options with patients and respect for patient’s preferences and multicultural differences Respond to phone calls, pages and/or messages in a timely manner Renal Core Topics 1. Teaching materials a. Reading material : selected articles and publications from journals and nephrology data base 2. Topics to be discussed during Rounds: a. Hemodialysis and peritoneal dialysis: techniques b. Hemodialysis and peritoneal dialysis: dialysis prescription c. Evaluation of kidney structure and function 1. Urinalysis 2. Measurement of GFR 3. Evaluation of proteinuria 4. Measurement of urinary electrolytes 5. Renal imaging techniques d. Chronic Kidney disease e. Acute Kidney injury f. Metabolic acidosis g. Metabolic alkalosis h. Disorders of water metabolism ( hyponatremia and hypernatremia) i. Disorders of potassium and magnesium metabolism j. Disorders of calcium, phosphorus and bone metabolism k. Overview of evaluation and treatment of hypertension l. Glomerular syndromes 1. Nephritic syndrome 2. Nephrotic syndrome m. Diabetic nephropathy n. Principles of kidney transplantation Rheumatology Dear Residents: Welcome to your rotation in Rheumatology. We are delighted that you will be joining us and look forward to a productive experience. The rotation is designed to give you maximum exposure to outpatient rheumatology. Interested residents may elect to spend time on the inpatient consultation service. All rheumatology clinics are held at Carolina Pointe II 3rd floor. Clinics begin at 8:30 am and are usually finished by 5:30 pm. You will be working with different attendings each day as listed below. If you will not be able to attend a clinic because of a conflict with your continuity clinic or if you have been pulled to cover another service, please let the attending know as soon as possible. The clinic phone number is 966-4191. Monday Fellows Clinic (Attendings rotate) Tuesday Dr. Mary Anne Dooley Dr. Beth Jonas Dr. Robert Roubey Wednesday Dr. Robert Berger Dr. Alfredo Rivadeneira Dr. Joanne Jordan Thursday Dr. Beth Jonas Dr. Alfredo Rivadeneira Dr. Robert Roubey Dr. Teresa Tarrant Friday Dr. Alfredo Rivadeneira Dr. Robert Berger Dr. Amanda Nelson Residents who wish to have exposure to outpatient Allergy/ Immunology should discuss this with Dr. Jonas prior to the rotation, so this can be scheduled. Rheumatology Grand Rounds are held on Friday at 8:30 am each week at the Thurston Arthritis Research Center (TARC) on the 3rd floor of the Thurston Building. All residents are expected to attend. Each week the conference is followed by case discussions with the faculty and fellows. The conference is usually over at about 10 am and then the residents can attend the clinic. Once monthly there is a radiology conference (in place of GR) which is held in the Radiology Conference Room in the basement of the Women’s Hospital. You will get the schedule when you start your rotation. Rheum/Allergy/Immunology Journal Club is held on Wednesdays at 1pm in the 3rd floor conference room at TARC. This conference is optional. Residents are expected to augment their clinical learning with reading. Prior to the beginning of the rotation, residents are STRONGLY ENCOURAGED to read Kelley’s Textbook of Rheumatology Chapter 35: “History and Physical Examination of the Musculoskeletal System”. The book is available in electronic format on the MD Consult section in the Health Sciences Library website. In addition to Kelley’s textbook, other good sources for reading include the Primer on the Rheumatic Diseases 13th Edition, Harrison’s Rheumatology 2nd Edition and MKSAP 15 Rheumatology. A reading list is available of good review papers of topics in rheumatology. If you are having trouble locating resources, please discuss this with Dr. Jonas or any faculty member. Please contact Dr. Jonas if you have any questions. 216-2664, phone 966-0560. Contact information bjonas@med.unc.edu, pager We look forward to working with you. Beth L. Jonas, MD Director, Rheumatology Fellowship Training Program Thurston Arthritis Research Center UNC- Chapel Hill Rheumatology Curriculum UNC Internal Medicine Training Program Rheumatology Rotation Competency-based Goals and Objectives Contact: Dr. Beth Jonas pager 216-2664 Teaching site: Carolina Pointe II 3rd floor clinic Goals: The goal of this experience will be for the residents to gain experience in the outpatient evaluation and management of patients with a broad spectrum of musculoskeletal and rheumatic diseases. 1. Objectives • Medical knowledge Describe the epidemiology, genetics, natural history, clinical expression of the rheumatic diseases encountered in the outpatient setting. Describe structure and function of musculoskeletal tissues and joints Summarize an approach to the evaluation of multi-organ inflammatory disorders Distinguish non-rheumatic disorders from rheumatic diseases Interpret diagnostic tests used in the evaluation of outpatients with suspected rheumatic and musculoskeletal diseases Demonstrate ability to critically appraise and cite literature pertinent to the evaluation of outpatients with rheumatic disorders. • Patient care Effectively perform a comprehensive history and complete physical examination in patients with rheumatic symptoms or abnormal immunologic tests Appropriately select and interpret laboratory, imaging, and pathologic studies used in the evaluation of rheumatic disorders Gain experience in procedures including arthrocentesis and injections, compensated polarized microscopy, and synovial fluid analysis Construct a comprehensive treatment plan and assess response to therapy. Counsel patients concerning their diagnosis, planned diagnostic testing and recommended therapies. Utilize validated instruments in the assessment of pain, function, and quality of life to monitor and adjust therapy. • Practice-based learning and improvement Effectively use technology to manage information, support patient care decisions, and enhance both patient and physician education. Integrate and apply knowledge obtained from multiple sources to the care of outpatients Demonstrate ability to critically assess the scientific literature Set and assess individualized learning goals Analyze clinical experience and employ a systematic methodology for improvement Develop and maintain a willingness to learn from errors, and use errors to improve the system or processes of care • Systems-based practice Discuss how the health care system affects the management of outpatients with rheumatic diseases. Demonstrate effective collaboration with other health care providers, including physical and occupational therapists and orthopedic surgeons, in the care of patients with rheumatic diseases Determine cost-effectiveness of alternative proposed interventions. Design cost-effective plans based on knowledge of best practices Demonstrate awareness of the impact of diagnostic and therapeutic recommendations on the health care system, cost of the procedure, insurance coverage, and resources utilized • Interpersonal skills and communication Approach patients with an empathetic and understandable manner Demonstrate effective skills of listening and speaking with patients, families and other members of the health care team Reliably and accurately communicate the patient's and his/her family's views and concerns to the attending Compose clear and timely consultation reports and interval notes/letters, including a precise diagnosis whenever possible, differential diagnosis when appropriate, and recommend follow up or additional studies Counsel patients, families and colleagues regarding side effects and appropriate use of specific medications, providing written documentation when appropriate • Professionalism Be prompt and prepared for clinic Recognize the importance of patient primacy, patient privacy, patient autonomy, informed consent, and equitable respect and care to all Respect patients and their families, staff and colleagues Model ethical behavior by reporting back to the attending and referring providers key clinical findings, following through on clinical questions, laboratory testing and other patient care issues, and recognizing potential conflicts of interest Demonstrate integrity, honesty and openness in discussion of therapeutic options with patients and respect for patient’s preferences and multicultural differences Respond to phone calls, pages and/or messages in a timely manner 2. Learning activities / methods Competency SCE DID SDL DEM Patient Care (PC) x x x x Medical Knowledge x x x x Practice Based Learning and Improvement x x x x Personal and Communication Skills x Professionalism x x x x x Systems Based Practice x x x SCE - supervised clinical experience DID – didactics – case conferences, lectures, meetings SDL – self directed learning DEM – demonstrations, e.g. joint injection, infusion of biologics 3. Assessment tools Arthrocentesis logs Supervised clinical experience Formative evaluation Summative evaluation Emergency Medicine Curriculum UNC Department of Emergency Medicine The Emergency Department (ED) attendings work 8 hour shifts, 7a-3:00p, 1p-9p, 10 a-6p, 3p-11p, 6p-2a, and 11p-7a. Two attendings are on duty, with the exception of the time period from 2a to 10a when one attending is on duty. The ED has 3 main areas. The Acute Care area has 24 beds including 2 cardiac rooms and 3 trauma rooms. Team C is an adjacent area with 8 beds. Team C is open 9a to midnight daily. Pediatric Acute Care is a separate unit staffed by Pediatric attending and residents. Pediatric Acute Care is open from 9a-2a daily. After those hours, pediatric patients (age 15 and below) are treated in the main ED. During your rotation, you will be assigned shifts in both the Acute Care area of the ED and the Minor Trauma area. Guidelines for House officers Introduction and General Principles Welcome to the Department of Emergency Medicine! During this rotation, you will learn skills that are essential to your medical education. You will be supervised by faculty members who are Board Certified or Board Eligible in Emergency Medicine. Our faculty have practiced in a variety of institutions and settings, and thus, your experience here will be enhanced by exposure to different styles of practice. Emergency Medicine differs in many respects from the inpatient and clinic settings. During this rotation, you will see a broad spectrum of illnesses ranging from the most trivial complaints to life-threatening diseases. It is important to remember that all patients come to the ED for a reason. Many present to the ED early in the course of their illness, therefore a serious disease may initially present to you as an apparently benign compliant. Many may present with complaints that could be handled elsewhere. It is our role to ensure our patients receive our best efforts to guide them through the increasing complex healthcare system as well as to diagnose and treat acute care conditions. Remember the Emergency Department is an important portal of entry into the hospital and provides a strong impression of the institution to patients, their families, and referring physicians from other medical centers. House Officer Requirements for Successful Completion of Emergency Medicine Rotation 1. Completion of the Online Orientation Module Each house officer must complete the online orientation course and exam before starting their Emergency Medicine rotation. The orientation module is available online at www.med.unc.edu/wrkunits/2depts/emergmed. 2. Assigned shifts in the Emergency Department Be prompt for your assigned shifts. If you are ill or must miss an assigned shift, you need to contact: a. Your Chief Resident. Chief Residents from each rotating department will be responsible for providing replacement coverage for their individual department residents who are unable to fill an assigned shift. b. The ED attending physician working at the time your shift begins( 966-4721) In order to successfully complete the ED rotation as required by your residency, you must complete all assigned shifts. Illnesses are only excused if verified by your personal physician (not a resident physician) or your residency director. 3. Resident Conferences In order for the Department of Emergency Medicine, Medicine, Surgery, Family Medicine and OB/GYN to meet the requirements of the Residency Review Committee, weekly attendance at our Emergency Medicine Conferences is MANDATORY. These conferences are held on Wednesday mornings from 7a to noon. The schedule of topics is available monthly. Emergency Medicine interns/residents are required to attend conferences 5 hours per week. Off service interns/residents are required attend 3 hours per week. During your rotation, you will likely be scheduled in the ED on one or more Wednesday mornings. On these mornings you should attend sign out rounds and check in with the ED attending prior to departing for conference. When you are not scheduled to work in the ED, you should attend at least part of the Wednesday morning conference. Attendance will be taken at these conferences and reported to individual residency directors at the end of each rotation along with your final evaluation. If you have questions or concerns, please feel free to contact: Kevin Biese, MD Assistant Professor Education Director 966-6440 Important Items to Keep in Mind: 1. Although you will be quiet busy at times, make sure you speak to any family members or visitors who may be in the waiting room after you have finished your evaluation. It is important to let them know how well the patient is doing and give them an estimate of the anticipated length of stay. Always overestimate the length of stay. Things may take longer than you think. 2. Laboratory studies and X-Rays are ordered only if they impact on acute treatment, immediate decision making, or are essential for the provision of follow up care. The Emergency Department is not the place to begin an extensive workup of non-critical problems. 3. Every patient should be given instructions for follow up care and referred to a follow up physician, no matter how trivial the problem may seem. ( see documentation and charting guidelines) 4. You should be able to arrive at a reasonable clinical diagnosis on most patients. If you lack a definitive diagnosis, you must have formulated a clear differential diagnosis and have ruled out all possible life treating conditions before the patient can be discharged safely. 5. Information concerning patients seen or discussed in the ED is confidential. It should not be discussed anywhere else, other than medical conference setting. This means you must not discuss patient information in the hallways, nor elevators, nor in downtown restaurants, etc. You are a professional and must conduct yourself as such. 6. All patients who are seen in the Emergency Department are the ultimate responsibility of the attending emergency physician. Consequently, THE EMERGENCY DEPARTMENT ATTENDING MUST SEE EVERY PATIENT AND SIGN EVERY CHART PRIOR TO THE PATIENTS DISCHARGE, ADMISSION OR TRANSFER. 7. Some patients have such serious illness at the time of presentation that they may decompensate in a very short period of time. Because of this, there are certain circumstances when it is vital for you to notify the attending physician of the patient’s condition IMMEDIATELY AND POSSIBLY BEFORE YOU HAVE FINISHED YOUR INTIAL EVALUATION. (You will find a list of these circumstances attached in this handout.) If you think a particular patient is unstable, alert the attending on duty. 8. T System: All ED patients are tracked on a computer system called T System. When you arrive in the ED, you will be instructed how to use this system to sign up as the provider for the patients you are evaluating. In order to access this system, you must have a valid UNC Hospital code and password. 9. As patients enter the Emergency Department, they are triaged by the nursing staff. The triage designations are : ESI-1 ESI-2 ESI-3 ESI-4 ESI-5 Stability of vital functions Unstable Stable Stable Stable Stable Life-threat or organthreat Obvious Reasonably likely Unlikely (possible) No No Severe pain or severe distress Immediately Sometimes Seldom No No Expected resource intensity Maximum: staff at bedside continuously; mobilization of outside resources High: multiple, often complex diagnostic studies; frequent consultation; continuous (remote) monitoring Medium: multiple diagnostic studies; or brief observation; or complex procedure Low: one Low: simple exam diagnostic only study; or simple procedure Med/staff response Immediate team effort Minutes Up to 1 hr Could be delayed Could be delayed Expected time to disposition 1.5 hr 4 hr 6 hr 2 hr 1 hr Examples Cardiac arrest, intubated/hypotensive trauma patient, acute (<3 hr) MI or stroke Most chest pain, stable trauma (MOI concerning), elderly pneumonia patient, altered mental status, behavioral disturbance Most abdominal pain, dehydration, esophageal food impaction, hip fracture Closed extremity trauma, simple lac, simple cystitis, typical migraine Sore throat, minor burn, recheck In general, patients should be seen in the order in which they arrive in the ED, however patients triaged as “1” or “2” should be evaluated before those designated “3-4-5”. If you are unsure which patient you should evaluate next, ask the attending or a senior resident to direct you. SCHEDULE Housestaff will be assigned to one section of the department and will report ONLY to the attending staffing that section. RESPONSIBILITIES Role of the Emergency Department Attending The ED attending is primarily responsible for patient flow and consultation. The ED attending will be responsible for the supervision of all medical students and house officers. Housestaff cannot sign student orders. Role of the PGY-III Resident The PGY-III Emergency Medicine Resident has three main responsibilities in the ED: 1. Directly evaluate patients as the primary physician, with particular attention to critically ill or injured patients. 2. Ensure that patient flow in the ED is maintained. 3. Supervise one or more PGY-I residents who are working in the ED. 4. Perform or supervise procedures required for patient care. 5. At times, these residents may take a turn at being “in charge” of the ED under the supervision of the attending. . Role of the PGY-I and PGY-II Residents and Medical Students The PGY-I resident and medical student are primarily responsible for patient evaluation and management. Remember that you are here to learn and that specific questions are expected. It is better to ask and ask early! PATIENT CARE AND CASE PRESENTATION It will be the responsibility of the EM PGY-III resident, all PGY-I residents, and medical students to pick up new patients as they are added to the board by the triage nurse. Patients are to be seen according to their time of entry into the ED unless another patient with a potentially life-threatening complaint has not yet been evaluated. Patients with life-threatening complaints are designated by a triage classification of “1” (in red) and should be seen promptly. If you are not certain whether a particular patient is to be seen, ask the attending physician or triage nurse. The residents will see and evaluate the majority of patients. This initial evaluation is to consist of a history and physical examination, which may be “directed” if the patient has an obviously isolated problem (such as a minor extremity injury). All other patients should have a complete history and physical examination including social and family history, medications and allergies. This evaluation should take no longer than 5 to 10 minutes to complete. ANY PATIENT WITH A CONDITION WHICH MAY DETERIORATE PRECIPITOUSLY MUST BE CALLED TO THE ATTENTION OF THE ED ATTENDING IMMEDIATELY, EVEN IF THE INITIAL EVALUATION IS NOT COMPLETED. A list of such conditions is listed in this handout. After formulating a differential diagnosis and treatment plan, but before writing orders, the intern is to present the patient to the ED attending. At that time, an evaluation and treatment plan can be formulated and orders written. No verbal orders are acceptable. After all ancillary studies have been completed; the house officer is to present the case to the ED attending again, this time noting the results of laboratory values, X-rays, etc. At this time a disposition will be made and the patient will be either be discharged, admitted or transferred to a different institution. TYPES OF PATIENTS SEEN Adult patients with a wide variety of complaints are seen in the Acute Care area of the ED. In addition to evaluating and treating patients with general medical and surgical problems, you will gain experience with patients whose complaints include the following: Psychiatric - Our responsibility is medical clearance; be especially careful with elderly patients or those with confounding medical problems; some psychiatric patients will be seen directly by the Psychiatric consultants. OB-Gyn - Women at 20 weeks or greater gestation are transferred directly to Labor and Delivery. The exceptions to this are if they have any type of trauma or a complaint totally unrelated to pregnancy. All women between ages10-60 should be assumed to be pregnant until proven otherwise by a negative urine or serum pregnancy test. Trauma - Major trauma patients, as determined by criteria, are seen by the Trauma team, EM Attending and Senior Emergency Medicine Residents. Patients with lesser trauma are evaluated and treated by the general ED staff. Pediatrics (ages 15 and below) - These patients are seen directly by a Pediatric resident, either in Pediatric Acute Care (9a-11p) or in the Acute Care ED at other times. ANCILLARY SERVICES Laboratory Studies 1. Laboratory studies are ordered in writing on the order sheet. 2. Laboratory reports results can be obtained on the computer. Be sure to check the computer frequently for results so the patient can receive disposition in a timely manner 3. All laboratory studies must be documented on the chart, including those that are pending at the time of disposition. Radiologic Studies 1. If a patient needs an X-ray or other imaging study, write the order on the order sheet and give the order sheet to the clerk. You need to write a reason for the X-ray study, i.e. chest pain or SOB. The X-ray orders are entered into the computer by the nursing staff. 2. Look at the patient’s X-rays even though the radiologist’s interpretation is available. Remember that you have the advantage of knowing the patient’s clinical presentation and thus may notice something the radiologist might have misses. 3. If you have any questions regarding the interpretation of a particular radiograph, you may consult the radiology attending or resident by dialing 68850. 4. All radiologic studies must be documented on the chart! MEALS Housestaff are encouraged to briefly leave the ED for nutrition breaks as patient flow permits, but only after notifying the attending that they are leaving. DOCUMENTATION STANDARDS It is your responsibility to see that these standards are met on every chart. Charts will be returned to you for completion if documentation standards are not met. DISCHARGE INSTRUCTIONS AND FOLLOW-UP All patients are to receive a discharge instruction sheet prior to leaving the Emergency Department. There are specific items that must be included on the discharge form. PATIENTS LEAVING THE EMERGENCY DEPARTMENT AGAINST MEDICAL ADVICE (AMA) All patients who threaten to leave the Emergency Department against medical advice (AMA) must be seen by the ED attending immediately. The patient is required to sign an AMA form on the back of the chart and must be properly informed of the risks of departing AMA. SECURITY AND PARKING Escorts to the parking decks are available 24 hours a day. USE THEM!! Use the Point to Point Service (962-7867) or have hospital security accompany you! You cannot park in the ED patient parking lot. DRESS CODE AND IDENTIFICATION Name badges must be worn at all times. Housestaff are expected to look and act like professionals at all times. Scrub suits are acceptable for wear in the Emergency Department provided they are clean and in good condition. Jeans, shorts, sweats and T-shirts are not permitted. WHEN YOUR SHIFT ENDS You must turn your patients over to an intern or resident on duty in the ED. If your patient is nearing completion of their evaluation – please fill out the chart completely including the discharge form if appropriate. If the evaluation is in progress, please have a clear plan to pass on to the next doctor. Medical Conditions Requiring Immediate Attending Physician Notification The following is a list of conditions that require immediate notification of the Emergency Department attending physician, regardless of your level of training. This list does not cover all possible situations, and you should feel free to notify the attending immediately if you have a patient you feel may deteriorate precipitously or if you are uncomfortable given your present level of training. 1. Any patient who presents with or develops acute cardiopulmonary arrest. 2. Any patient with a complete or partially obstructed airway. 3. Any patient who presents with or develops a significant cardiac arrhythmia, whether stable or not. 4. Any patient with acute onset Alteration of Mental Status (AOMS). This includes any patient presenting with this as the chief complaint or any patient whose mental status deteriorates while in the ED. 5. Any patient with significant hypotension or hypertension. For these purposes, significant hypotension will be defined as blood pressure of less than 100 mmHg systolic and significant hypertension will be defined as a blood pressure of greater than or equal to 180 mmHg systolic or hypertension associated with acute alteration of mental status. 6. Any patient with severe respiratory distress. For these purposes, significant respiratory distress will be defined as a respiratory rate greater than 30 breaths/minute, any patient with a pulse oximeter reading of less than or equal to 90 mmHg, any patient with an acute elevation of pCO2 greater than or equal to 60 mm Hg, any patient with a complaint of shortness of breath accompanied by diaphoresis, use of accessory muscles of respiration, cyanosis, alteration of mental status, bradycardia, or any other signs consistent with imminent respiratory failure. 7. Any patient with significant tachycardia or bradycardia. For these purposes, significant tachycardia is defined as a heart rate greater than or equal to 150 beats/minute and significant bradycardia is defined as a heart rate less than or equal to 60 beats/minute. 8. Any patient with a significant cardiac arrhythmia. 9. Any patient with either clinical or EKG evidence of acute myocardial infarction. 10. Any patient with a fever greater than 105 degrees Fahrenheit, any patient with significant alteration of mental status associated with a fever, or any patient with a fever and a potentially immunocompromised state (e.g. HIV disease, cancer patients, transplant patients, etc.) 11. Any patient with significant hypothermia. For these purposes, significant hypothermia is defined as a rectal temperature less than or equal to 95 degrees Fahrenheit. 12. Any patient with severe abdominal pain or abdominal pain associated with peritoneal signs. 13. Any female with abdominal pain and a positive pregnancy test. 14. Any patient with significant upper or lower GI bleeding (whether hypotensive or not). 15. Any patient who develops seizure activity while in the Emergency Department. 16. Any patient with significant abnormality of any laboratory value (e.g. hypo/hypernatremia, hypo/hyperkalemia, symptomatic hypercalcemia, hematocrit less than 28, etc.). 17. Any patient with a history of significant trauma. 18. Any patient with a pregnancy and sign/symptoms of a precipitous delivery. 19. Any patient with an overdose of prescription or over-the-counter medications. 20. Any patient or visitor who gives evidence of becoming significantly agitated, violent, or suicidal. 21. Any patient with a blood sugar of less than 70 mg/dL. 22. Any patient with a snake bite. 23. Any patient with significant bleeding, or bleeding associated with hemophilia (blood dyscrasias). 24. Any patient with a significant allergic reaction. 25. ANY PATIENT WHO YOU FEEL IS BEYOND YOUR PRESENT CAPABILITIES AS A RESIDENT, OR WHO YOU THINK MAY DETERIORATE SUDDENLY. Documentation Standards The following information is required on all charts for all Emergency Department patients for legal and billing purposes. Please review this in conjunction with the copy of the chart included in this packet. 1. The Emergency Department uses the T System for charting. Please complete the T System training module before starting your first shift. 2. For all patient charts, documentation should reach a “level 5” by the standards of the T System Documentation System. Please confirm this before signing your chart. 3. It is important to write a short summary of your assessment and plan in each chart.. Based on the differential problem list that you have established, it should be obvious by reviewing the chart how you distinguished among the possibilities and came to your final diagnosis. Some examples: GI cocktail given, patient with complete relief; Phenergan 25mg IV given, nausea relieved and patient tolerating PO well. If you make a clinical diagnosis without any work-up, you need to explain that. For example: 20 year old white female with reproducible chest wall pain, no risk factors for CAD and no associated symptoms, likelihood of cardiopulmonary disease as the underlying etiology is very low. We will treat her with NSAID’s. Patient knows to return if symptoms change or worsen. 4. You need to list the medications the patient is taking and any drug allergies the patient has. 5. If the patient is in the Emergency Room for a significant length of time waiting for disposition or a bed, you need to make note that you reevaluated the patient during this time. For example: 2:45 pm Patient now afebrile and tolerating oral fluids well. Many conditions such as respiratory distress, chest pain and abdominal pain require frequent reevaluation, and you need to document it. 6. If you call a consultant to see the patient, record the time and who you talked with. For example: 6 pm Discussed case with Dr. Smith (General Surgery) who will evaluate patient. “Curbside” consultations are not official. If there is really a question, the patient must be seen by the consultant. 7. Record a procedure note for all procedures done on the patient including laceration repairs, lumbar punctures, central lines, etc . 8. Please select a disposition and diagnosis (often more than 1diagnosis) for each patient. DISCHARGE INSTRUCTIONS The T system has standard discharge instructions for many different diagnoses as well as medications Every discharged patient should receive 1 or more of these instruction sets. All patients should receive Follow-Up. Follow-up options include but are not limited to: 1. Follow-up with their own doctor (MUST BE NAMED) for a specific period of time. If the patient is unable to identify an MD, a referral should be given. 2. UNC Clinic Appointment: Options for obtaining this are: * You can call and get an appointment for the patient (Mon-Fri 8a-5p) * Fill out a clinic referral sheet available in the ED; these are faxed to a central office where appointments are made, * You can give the patient the phone number for a specific clinic (listed in the T system discharge instructions) BUT, keep in mind, it may be several months before a patient can get an appointment. Welcome! From the Nurses in the Emergency Department The following handout details survival skills for your emergency department rotation. We hope that it may be helpful to you. The ED is divided into several sections: 1. 2. 3. 4. Triage Acute Area Team C Pediatric Acute Care The nursing staff is assigned by “team.” One or two nurses are assigned to the triage area. These nurses are responsible for screening all patients and prioritizing their care. The Acute Area is divided into Team A and Team B. Two or more nurses are assigned to cover each of these teams. There are three trauma bays, including a pediatric resuscitation bay. There are two cardiac resuscitation rooms. The Acute Area is divided into the A and B teams which are each responsible for ½ the acute area of the department. Team C is a separate area that usually evaluates ESI score 4 and 5 patients (see above). A charge nurse is assigned to coordinate the care of the ED patients. At various times, the charge nurse will also have a patient care assignment. Two nurses are assigned to the trauma team. If there is a trauma in progress and the nurse assigned to a certain area becomes unavailable, refer all questions to the charge nurse. Remember, if you are busy, so is the nursing staff! This is a team-oriented department. Help us and each other! General Information It is mandatory that you wear your name tag! Familiarize yourself with the clean and dirty utility rooms on your first day. You will find this invaluable. Most of the equipment you need is located in these areas. Equipment is secured in the PYXIS. Tidy up after yourself after completing an exam or procedure. There are trash cans located at each patient care bedside. (This includes the lounge!) The ED staff is a life form in itself. The nursing assistants, clerks, nurses, and social worker can be great resources for the inside scoop on usual routines, community resources, etc. Clerks can help you with phone calls and paging. Clerks answer the phones, even if you have paged someone. Listen to the intercom for your name or the person you have paged. The key staff in the ED has assigned intercom cell phones. Nursing Assistants can perform the following: 1. 2. 3. 4. 5. 6. simple wound preps crutch set-up lab transport patient transport (excluding monitored patients) room set-up assist with procedures Remove all needles and sharps from trays and dispose of them in the sharps box! If a laceration needs sutures, anesthetize the wound prior to wound prep. The department’s infection rate has been consistently 0% because the NA’s do an excellent job. RN’s 1. Unless the patient is acutely ill, please allow the RN to triage the patient prior to beginning your exam or Gathering information . 2. ED nurses will assess the acuity of patients and institute treatment and diagnostic procedures prior to you seeing the patient. For example: monitoring, IV access. Orders still need to be written for the patient. Educational Conferences Emergency Medicine conferences are held Wednesday from 7:00 am to noon. All PGY1 residents assigned to the Emergency Department each month will be expected to attend. Scheduling in the Emergency Department PGY-1 Medicine Interns will work 12 hour shifts beginning at 7 am, 10 am, or 7pm. These times will rotate throughout the month.