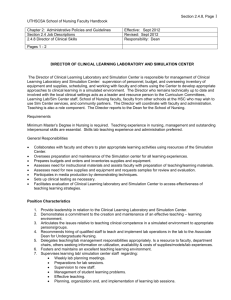
Date accepted: - National League for Nursing
advertisement
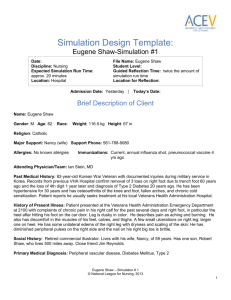
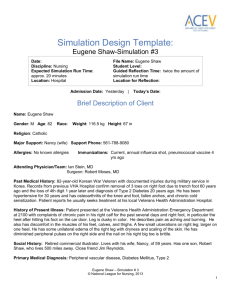
Simulation Design Template: Eugene Shaw-Simulation #2 Date: Discipline: Nursing Expected Simulation Run Time: approx. 20 minutes Location: Hospital File Name: Eugene Shaw Student Level: Guided Reflection Time: twice the amount of simulation run time Location for Reflection: Admission Date: Yesterday | Today’s Date: Brief Description of Client Name: Eugene Shaw Gender: M Age: 82 Race: Weight: 116.5 kg Height: 67 in Religion: Catholic Major Support: Nancy (wife) Support Phone: 561-788-9080 Allergies: No known allergies Immunizations: Current, annual influenza shot, pneumococcal vaccine 4 yrs ago Attending Physician/Team: Ian Stein, MD Surgeon: Robert Moses, MD Past Medical History: 82-year-old Korean War Veteran with documented injuries during military service in Korea. Records from previous VHA Hospital confirm removal of 3 toes on right foot due to trench foot 60 years ago and the loss of 4th digit 1 year later and diagnosis of Type 2 Diabetes 20 years ago. He has been hypertensive for 30 years and has osteoarthritis of the knee and foot, fallen arches, and chronic cold sensitization. Patient reports he usually seeks treatment at his local Veterans Health Administration Hospital. History of Present Illness: Patient presented at the Veterans Health Administration Emergency Department at 2100 with complaints of chronic pain in his right calf for the past several days and right foot, in particular the heel after hitting his foot on the car door. Leg is dusky in color. He describes pain as aching and burning. He also has discomfort in the muscles of his feet, calves, and thighs. A few small ulcerations on right leg; larger one on heel. He has some unilateral edema of the right leg with dryness and scaling of the skin. He has diminished peripheral pulses on the right side and the nail on his right big toe is brittle. Social History: Retired commercial illustrator. Lives with his wife, Nancy, of 59 years. Has one son, Robert Shaw, who lives 500 miles away. Close friend Jim Reynolds. Primary Medical Diagnosis: Peripheral vascular disease, Diabetes Mellitus, Type 2 Eugene Shaw – Simulation # 2 © National League for Nursing, 2013 1 Surgeries/Procedures & Dates: Surgical removal of 3 toes on right foot 60 years ago, subsequent loss of 4th digit on right foot 1 year later Nursing Diagnoses: Acute pain related to tissue injury; risk for impaired skin integrity related to poor circulation; activity intolerance related to pain; risk for injury related to poor control of diabetes Psychomotor Skills Required Prior to Simulation Basic assessment skills IV drug administration Blood glucose monitoring Cognitive Activities Required Prior to Simulation [i.e. independent reading (R), video review (V), computer simulations (CS), lecture (L)] Readings in textbook on care of the patient with peripheral vascular disease. Type 2 Diabetes and care of the pre-operative patient (R) Simulation Learning Objectives General Objectives 1. Practice standard precautions throughout the exam. 2. Employ effective strategies to reduce risk of harm to the client. 3. Assume the role of team leader or member. 4. Perform a focused physical assessment noting abnormal findings. 5. Recognize changes in patient symptoms and/or signs of patient compromise. 6. Perform priority nursing actions based on clinical data. 7. Reassess/monitor patient status following nursing interventions. 8. Perform within scope of practice. 9. Demonstrate knowledge of legal and ethical obligations. 10. Communicate with client in a manner that illustrates caring for his/her overall well-being. 11. Communicate appropriately with physician and/or other healthcare team members in a timely, organized, patient-specific manner. 12. Apply the nursing process to initiate care of the pre-operative patient. Simulation Scenario Objectives 1. Prepare patient for surgery. 2. Administer pre-operative IV medication. Eugene Shaw – Simulation # 2 © National League for Nursing, 2013 2 3. Conduct pre-op teaching. 4. Respond to patient-specific physical and emotional needs related to surgical prodecure. References, Evidence-Based Practice Guidelines, Protocols, or Algorithms Used for This Scenario: American Diabetes Association. (2012). Standards of medical care in diabetes-2012. Diabetes Care 35(Supp 1), s11-s63. doi: 10.2337.dc12-s011 Cole, C. A. (2012). Implied consent and nursing practice: Ethical or convenient? Nursing Ethics, 19(4), 550557. doi: 10.1177/0969733011436028 Lee, C.-K., & Lee, I. F. K. (2012). Preoperative patient teaching: The practice and perceptions among surgical ward nurses. Journal of Clinical Nursing, n/a-n/a. doi: 10.1111/j.1365-2702.2012.04345.x Lovell, M., Myers, K., Forbes, T. L., Dresser, G., & Weiss, E. (2011). Peripheral arterial disease: Application of the chronic care model. Journal of Vascular Nursing, 29(4), 147-152. Websites: The Korean War Veteran's Association Home Page: www.kwva.org The Korean War Project website: www.koreanwar.org Fidelity (choose all that apply to this simulation) Setting/Environment: ER Med-Surg Peds ICU OR / PACU Women’s Center Behavioral Health Home Health Pre-Hospital Other: Medications and Fluids: IV Fluids: Oral Meds: IVPB: see chart IV Push: IM or SC: Diagnostics Available: Labs X-rays (Images) chest 12-Lead EKG Other: Simulator Manikin/s Needed: Standardized patient, moderate or high fidelity Documentation Forms: manikin. Right leg has bluish skin tone and Physician Orders Eugene Shaw – Simulation # 2 © National League for Nursing, 2013 3 ulceration on heel. Moulage to simulate missing toes on right foot. Can tape picture or drawing to foot. (Note: some manikins have pedal pulses in both feet that can be regulated to be diminished/absent in right leg, but since schools may not have a manikin with this capability, we are providing neurovascular assessment information in the nurse’s report.) Props: Foley catheter inserted into manikin; draining clear yellow urine. Equipment Attached to Manikin: IV tubing with primary line Lactated Ringers running at 125 mL/hr Secondary IV line IV pump Foley catheter 100 mL output PCA pump running IVPB with running at mL/hr 02 Monitor attached ID band Other: Equipment Available in Room: Bedpan/Urinal Foley kit Straight Catheter Kit Incentive Spirometer Fluids IV start kit IV tubing IVPB Tubing IV Pump Feeding Pump Pressure Bag 02 delivery device (type) Crash cart with airway devices and emergency medications Defibrillator/Pacer Admit Orders Flow sheet Medication Administration Record Kardex Graphic Record Shift Assessment Triage Forms Code Record Anesthesia / PACU Record Standing (Protocol) Orders Transfer Orders Other: see chart Recommended Mode for Simulation: (i.e. manual, programmed, etc.) Mode will not change for this scenario. Simulator may be set manually or programmed or this simulation may be conducted with a standardized patient. Student Information Needed Prior to Scenario: Has been oriented to simulator Understands guidelines /expectations for scenario Has accomplished all pre-simulation requirements All participants understand their assigned roles Has been given time frame expectations Other: Provide student with a blank pre-op checklist. Eugene Shaw – Simulation # 2 © National League for Nursing, 2013 4 Suction Other: Roles/Guidelines for Roles: Primary Nurse Secondary Nurse Clinical Instructor Family Member #1 Wife, Nancy Family Member #2 Observer/s Recorder Physician/Advanced Practice Nurse Respiratory Therapy Anesthesia Pharmacy Lab Imaging Social Services Clergy Unlicensed Assistive Personnel Code Team Other: Important Information Related to Roles: Report Students Will Receive Before Simulation Time: 0630 Monday morning Situation: Mr. Eugene Shaw, age 82, came to the ER on Saturday at 2100 with complaints of pain and a burning sensation in his right leg. He has some small ulcerations of the skin, especially on the heel, with bluish discoloration of his right foot and some ankle edema. He was admitted to our unit Sunday morning at 0600. The surgeon evaluated him and said his angiogram revealed a clot in the artery just below the right knee. He reluctantly agreed to surgery and is scheduled for a femoral-popliteal bypass this morning at 0800. The plan is to discharge him about 2-5 days post-op. Physical therapy will evaluate him to develop a post-op plan of care. Background: Mr. Shaw has a 30-year history of hypertension, osteoarthritis of the knee and foot, fallen arches and chronic cold sensitization. For the past 40 years he has had nocturnal pain in lower limbs and hands. He was diagnosed with Type 2 Diabetes 20 years ago. He admits that he does not stick to his diet and the doctor put him on Simvastatin to prevent his cholesterol from going up. Mr. Shaw insists that he takes his medications regularly. He says he stopped smoking at home over 50 years ago when his son was born, but still sneaks a few cigarettes when out with friends at the local bar. Eugene Shaw – Simulation # 2 © National League for Nursing, 2013 5 Assessment: At 0600 hours his vitals were stable with temperature of 98.6 F (37 C), BP 128/70, heart rate 88, respirations 16, SpO2 96% on room air, and pain at 7 on a scale of zero to ten. He has continued to complain of burning pain in his right leg and has been medicated with Vicodin for pain about every 3 hours. His last dose was at 0500. Mr. Shaw’s blood glucose was 130 mg/dL at 0600. Our neurovascular checks remain the same - a popliteal pulse but no pedal pulse. Pulses in the other limbs are normal. He has a left antecubital IV with Lactated Ringers running at 125 mL/hr. We inserted a Foley at 0600 in preparation for surgery. He is alert and orientated to person, place and time. He and his wife finally did a durable power of attorney last night. Recommendation: He is due for vitals and a pain assessment. Complete the pre-op checklist and give him his pre-op antibiotic. The blood type and crossmatch were sent directly to the OR. Significant Lab Values: refer to chart Physician Orders: refer to chart Home Medications: refer to chart Scenario Progression Outline Timing (approx.) 0-5 min Manikin Actions Expected Interventions May Use the Following Cues Resting in bed with right foot elevated on a pillow. Wash hands and introduce selves. Check patient ID. Perform initial assessment including vital signs. Assess pain. Role member providing cue: Patient Cue: If asked to describe and rate pain, Gene will say it continues to burn and ache, but he had medication recently and it’s only about 2 out of 10 now. Check output in Foley bag. Assess IV and administer IV medication. Role member providing cue: Patient Cue: If student does not tell Eugene that she is giving an “Is it time to go to the OR?” 5-10 min Answers questions appropriately. If students ask questions about how he lost his toes, he will reply, “Don’t look at my foot, it’s real ugly and I think that you might Eugene Shaw – Simulation # 2 © National League for Nursing, 2013 6 be scared to see how deformed it looks.” 10-15 min “Some doc I never met before tells me we have to have this operation. What if it doesn’t work? I lost 4 toes before ’cause of that darn war. It was so cold over there in Korea that my toes just turned black. After going over there my feet were always cold. It was tough to lose a part of your body especially ’cause I was so young. Will I lose my leg now because of what happened back then? I don’t know how I could manage if that happened.” antibiotic and explain its purpose, Gene will say, “What is that medication you’re giving me?” Complete pre-op check list. Teach about peripheral vascular disease; explain why physician is recommending that he have the femoral-popliteal bypass surgery; review consent form with Gene. Role member providing cue: Cue: Provide emotional support. Role member providing cue: Cue: “What will happen tomorrow – before and after the surgery?” 15-20 min “I did a durable power of attorney last night. The doctor and the nurses all said I should. Does that mean there’s a good chance I could die?” “Nancy is really upset. I told her not to come today – just to talk to the doctor about how the surgery went.” Eugene Shaw – Simulation # 2 © National League for Nursing, 2013 7 Debriefing/Guided Reflection Questions for This Simulation (Remember to identify important concepts or curricular threads that are specific to your program) 1. How did you feel throughout the simulation experience? 2. Describe the objectives you were able to achieve. 3. Which ones were you unable to achieve (if any)? 4. Did you have the knowledge and skills to meet objectives? 5. Were you satisfied with your ability to work through the simulation? 6. To Observer: Could the nurses have handled any aspects of the simulation differently? 7. Have you ever served in the military, or do you know someone who has? If so, how did your personal experience with these individuals influence your participation in the scenario? 8. If you were able to do this again, how could you have handled the situation differently? 9. What did the group do well? 10. What did the team feel was the primary nursing diagnosis? 11. How were physical and mental health aspects interrelated in this case? 12. What were the key assessments and interventions? 13. Is there anything else you would like to discuss? Specific Debriefing Questions for this Scenario: 1. What were Gene’s specific nursing care needs related to preparation for his femoral-popliteal bypass surgery? 2. Think about Gene and his situation; what did you think about the fears he expressed? 3. What potential problems might Gene encounter after surgery? Consider his medical diagnoses, lifestyle and any other factors, as well as the challenges presented by his surgery. Eugene Shaw – Simulation # 2 © National League for Nursing, 2013 8