Statement of Dr. Caspari
advertisement

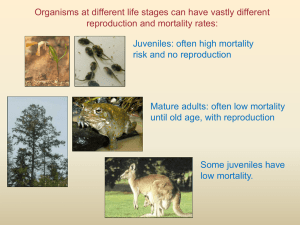
The scars of human evolution: Recent longevity and its consequences Rachel Caspari Central Michigan University Abstract My research addresses a fundamental reason that the scars of human evolution have not been eliminated by natural selection: many of the scars discussed in this dialog are expressed in older adults and older adults were rare until very recently. These scars include the orthopedic problems associated with bipedalism, pelvic organ prolapse and urinary incontinence (also a by-product of bipedalism), chronic degenerative diseases, and even the negative consequences of metabolic and dietary adaptations such as late onset diabetes. For most of human evolution, survivorship to older adulthood was a rarity and few individuals were affected by these conditions. Only in the last 30,000 years or so, did large numbers of humans live into older adulthood. The demographic consequences of this made modern humans among the most evolutionarily successful mammals on the planet, but also resulted in unfortunate consequences that only became apparent in older individuals. There are also negative tradeoffs of the demographic shift itself, including many of the infectious diseases that plague humans today. Thus, many of the scars of human evolution are directly or indirectly associated with an increase in longevity. Statement Over a century ago the Croatian paleontologist Dragutin Gorjanovic-Kramberger excavated and described Neandertal fossils from a rock shelter near Krapina, a small town about 40 km northwest of Zagreb. Although the fossils from the site are fragmentary, they represent the remains of perhaps as many as 70 individuals, most found within the same stratigraphic layer, with U-series and ESR dates of about 130,000 years BP. Because of the number and proximity of the fossils, because the sediments at the site accumulated rapidly over a short period of time, and because many of the bones share unique genetic features, paleoanthropologists believe that the remains from Krapina approximate a population. Therefore Krapina is one of the few hominid sites amenable to demographic analysis. Assessing the age at death of fossil remains is the key to reconstructing the demography of a prehistoric population. As with the fossil record in general, the best preserved remains at Krapina are dental because of the dense mineral structure of teeth. Fortunately, teeth are also one of the best skeletal elements for assessing age at death, through analysis of dental wear (attrition) and changes in the internal structure of dental roots, in particular secondary dentin deposition in the pulp chamber. My colleagues and I have reconstructed the demography at Krapina, using age estimates based on attrition and secondary dentin deposition, evaluated using high resolution micro-CT imaging. We recently published the death distribution for the Krapina fossils, transformed into a survivorship curve by estimating the number of missing infants based on statistics from more recent archeological samples.1 The figure below compares the Krapina population with a large skeletal population from Libben, a demographically known site from Ohio more than 1000 years old, which, like other sites of its age, shows high adult mortality. The curve indicates what proportion of the sample survived to the ages indicated on the x axis; the steep decline indicates that Krapina, as a population, would have had remarkably high mortality rates, even compared to Libben. Virtually no one survived past age 30. As surprising as this is, Krapina is not unique: the few other fossil sites with large samples, such as Sima de los Huesos, an earlier fossil site from Atapuerca, Spain, show similar distributions. At Atapuerca, like Krapina, there are very high levels of juvenile and young adult mortality, with very few individuals surviving to age 35. It is possible that these distributions reflect the peculiarities of specific sites - taphonomic or catastrophic occurrences that somehow selected against the preservation of older individuals. However, our research focusing on the human fossil record more broadly suggests that such high mortality levels were not exceptional; rather, they reflect an archaic life history pattern characterized by high young adult mortality. Survivorship (percent surviving to age interval) 70 60 50 40 Krapina lx 30 Libben 20 10 0 5 10 15 20 25 Age in years 30 35 40 Libben Krapina lx 45 50 A few years ago, Sang-Hee Lee of the University of California at Riverside and I examined the question of whether there were changes in longevity over the course of human evolution.2 There are many problems associated with such a task: most of the fossils do not come from sites like Krapina that could even remotely be considered reflective of populations, age assessments are less precise as a result, individual sample sizes are generally very small, demographic profiles are dependent on knowledge of infant mortality which becomes more difficult to estimate as samples become more distant from modern humans, and by comparing fossils from different species and time periods, there are problems inherent in comparing samples with potentially different maturation rates. In order to deal with these problems, we effectively changed the question to one that was very broad and more easily addressed by the fossil record; instead of attempting to construct life tables by asking how long individuals lived, we asked, how many individuals lived to be old? We assessed what proportion of several large samples, representing different fossil groups and time periods, survived to older adulthood. This approach circumvented many of the problems associated with paleodemography, yet allowed us to test evolutionary hypotheses. We found that there was a clear distinction between what could be called an archaic pattern of survivorship and a more modern one. For example, the ratio of older:younger adults (OY ratio) in our Neandertal sample was about 0.4, representing an archaic pattern. This means that for every 10 young adults between the ages of 15-30 in the death distribution, there were only 4 older adults (those over 30). In contrast, the European Upper Paleolithic represents a modern pattern: for every 10 young adults in the Upper Paleolithic record, there were 20 older adults, an OY ratio of 2.0. OY ratios of 2.0 reflect a modern pattern – it is present in archaeological samples such as Libben, and even reflects the mortality statistics known for some living Hunter/Gatherer groups. With OY ratios of 2.0 there are a significant number of people surviving to be grandparents, with far reaching demographic implications. The major conclusion to emerge from this study was that adult survivorship increased dramatically quite late in human evolution. In a subsequent study3, we further concluded that cultural causes, rather than phylogenetic or ecological variables, were likely responsible for this increase in survivorship. We suggested that longevity increased due to social factors promoting the survivorship of older adults whose experience and economic support benefited their kin groups in the harsh conditions of Upper Pleistocene Europe. Increased adult survivorship had selective advantages on many levels. However, like other adaptations, it also has its scars. Many orthopedic problems, including the back and ankle problems discussed by DeSilva and Latimer in this symposium, are the negative consequences of bipedalism. Although these may affect people of all ages, risk increases significantly with age. Pelvic organ prolapse is another negative consequence of our bipedal adaptations, coupled with the obstetric dilemma discussed by Rosenberg in this symposium. Pelvic organ prolapse occurs when the muscles and ligaments supporting the pelvic floor weaken, allowing various pelvic organs (bladder, uterus, small bowel or rectum) to protrude into the vaginal wall. Prolapse is associated both with childbirth and with age; the risk of all forms of prolapse doubles with each decade of life, and currently it affects more than 50% of women over age 45. Urinary incontinence is another agerelated consequence of weakened pelvic floor architecture, coupled with age-related decrease in striated muscle fibers of the urethra walls; it has been suggested that individuals may lose up to 65% of these fibers over the course of their lives.4 Many conditions are a product of the aging process itself and while there are behavioral and genetic risk factors associated with them, they are often expressed simply because we live longer. Frequencies of chronic degenerative skeletal conditions such as osteoporosis and osteoarthritis are clearly associated with age. Osteoporosis is defined by having bone mineral density (BMD) more that 2.5 SD below the adult mean. It is caused by the bone loss that occurs throughout adult life, often coupled with the period of greatly accelerated bone loss immediately following menopause. Therefore, it is more prevalent in women. This condition was unlikely to plague our Paleolithic ancestors because of their shorter lives, and also may have been less prevalent in longer-lived human populations with high peak bone mineral density in young adulthood. Models by Hernandez and colleagues5 suggest that failure to gain bone during development and maturation may be the most important factor in the development of osteoporosis later in life, potentially extending the onset of osteoporosis by as much as a decade. However, because of recent aging trends, it is currently a major problem in populations worldwide. Finally, chronic non-communicative diseases are the most common causes of death world-wide: heart disease, stroke, chronic respiratory disease, and diabetes are the leading causes of mortality in the world, accounting for 63% of global deaths. According to the World Health Organization, less than 25% of these deaths occur in people under 60 years of age, and of these younger deaths, the vast majority occurs in societies with low mean household incomes. In addition to the diseases of older adulthood that naturally become more prevalent as people live longer, there are negative consequences associated with increased population size, a demographic implication of increased longevity itself. Increased adult survivorship causes increases in population size for several reasons. First, increased survivorship implies greater lifetime fertility for the individuals who are living longer. According to models developed by Adam Van Arsdale at Wellesley College, in order to survive, total fertility rates for populations with OY ratios of 0.4 would need to be 20% higher than populations with OY ratios of 2.0. If the fertility rates remained constant, with a decrease in mortality, populations will increase in size. Moreover, the investment of older folks in their children’s families increases their inclusive fitness. It is likely, that in the Upper Paleolithic, adult survivorship was beneficial to social groups as a whole, promoting intergenerational transfer of a variety of economic and cultural resources. In humans, as in other social species, there is transfer of resources among individuals which contributes to the inclusive fitness of a kin group. Intergenerational transfer is particularly important for humans, where it extends over several generations, in what has been called the Grandmother effect. As discussed by many workers, perhaps primarily by Kristen Hawkes of the University of Utah and her colleagues, grandparents routinely contribute economic and social resources to their descendents, increasing the fertility of their children and the survivorship of their grandchildren. These factors promote population increase and genetic and archeological evidence suggests that the Upper Paleolithic was associated with the beginning of a population expansion that has continued until the present. There are numerous negative consequences associated with increased population sizes and population densities, including the evolution of infectious diseases that emerged or became prevalent during the Neolithic. These diseases remained the leading cause of death in humans until the epidemiological transitions of the 20th century, and they remain major causes of mortality in many parts of the world. We have adapted to the rise of infectious diseases with modern medicine, and consequently, life expectancy continues to increase dramatically. Populations of the 20th and 21st centuries, especially in industrialized countries, may have OY ratios well over one hundred (think of the ages of people buried in a modern middle class American cemetery). The implications are that many of the scars of human evolution will be expressed in higher frequencies than ever before. 1 Wolpoff M and R Caspari 2006 Does Krapina reflect early Neandertal paleodemography?. Periodicum Biologorum 108 (4): 425-432. 2 Caspari R and SH Lee 2004 Older age becomes common late in human evolution. Proc. Natl. Acad Sci. USA 101:10895-10900. 3 Caspari R and SH Lee 2006 Is human longevity a consequence of cultural change or modern human biology? American Journal of Physical Anthropology 129:512-517. 4 DeLancey, JO and JA Ashton-Miller 2007 Functional Anatomy of the female pelvic floor Ann. N.Y. Acad. Sci. 1101: 266–296. 5 Hernandez , GS Beaupre and DS Carter 2003 A relative analysis of peak BMS, age related bone loss, and menopause on the development of osteoporosis. Osteoporosis Int. 14:843-847