Emergency Medicine Rotation Syllabus
advertisement
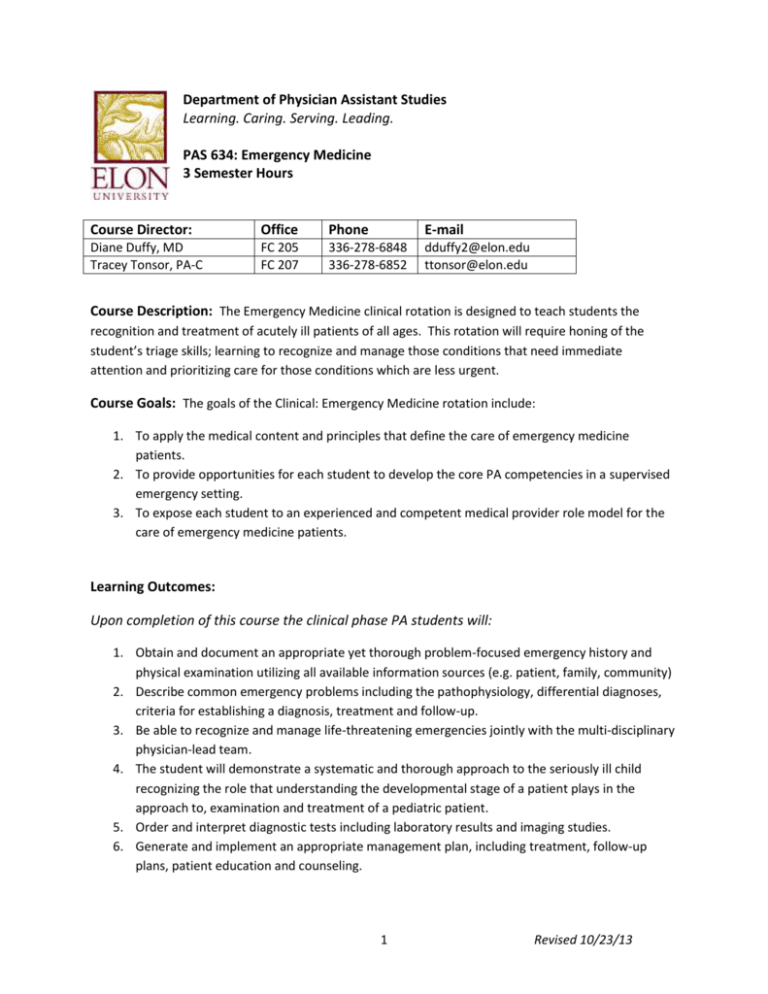
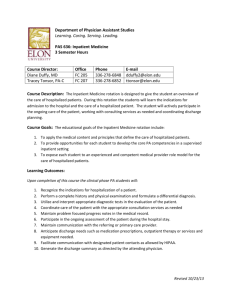
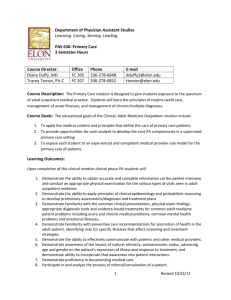
Department of Physician Assistant Studies Learning. Caring. Serving. Leading. PAS 634: Emergency Medicine 3 Semester Hours Course Director: Office Phone E-mail Diane Duffy, MD Tracey Tonsor, PA-C FC 205 FC 207 336-278-6848 336-278-6852 dduffy2@elon.edu ttonsor@elon.edu Course Description: The Emergency Medicine clinical rotation is designed to teach students the recognition and treatment of acutely ill patients of all ages. This rotation will require honing of the student’s triage skills; learning to recognize and manage those conditions that need immediate attention and prioritizing care for those conditions which are less urgent. Course Goals: The goals of the Clinical: Emergency Medicine rotation include: 1. To apply the medical content and principles that define the care of emergency medicine patients. 2. To provide opportunities for each student to develop the core PA competencies in a supervised emergency setting. 3. To expose each student to an experienced and competent medical provider role model for the care of emergency medicine patients. Learning Outcomes: Upon completion of this course the clinical phase PA students will: 1. Obtain and document an appropriate yet thorough problem-focused emergency history and physical examination utilizing all available information sources (e.g. patient, family, community) 2. Describe common emergency problems including the pathophysiology, differential diagnoses, criteria for establishing a diagnosis, treatment and follow-up. 3. Be able to recognize and manage life-threatening emergencies jointly with the multi-disciplinary physician-lead team. 4. The student will demonstrate a systematic and thorough approach to the seriously ill child recognizing the role that understanding the developmental stage of a patient plays in the approach to, examination and treatment of a pediatric patient. 5. Order and interpret diagnostic tests including laboratory results and imaging studies. 6. Generate and implement an appropriate management plan, including treatment, follow-up plans, patient education and counseling. 1 Revised 10/23/13 7. Discuss the appropriate use of medications in the emergency department related to such issues as dosage (taking into account considerations for pediatric, geriatric patients and women of reproductive age), indications, contraindications, interactions, complications and required monitoring. 8. Determine the proper IV therapy for specific emergency and acute situations. 9. Properly perform common emergency medicine procedures under the supervision of preceptor. 10. Be able to communicate in a medically professional manner, both orally and in writing to the patient, the family and with health care professionals. 11. Facilitate communication with the patient’s primary care physician to accomplish optimal transfer of care. 12. Be aware of and responsive to the emotional and psychological effects of emergency care on the patient and his/her support system. Teaching Methodologies: The content of this module will be presented through a variety of methods that include observation and participation at the clinical site, independent reading and participation in online activities developed to guide experiential learning. Accommodations: Students requiring academic accommodations must follow the “Academic Support” policy in the Elon University DPAS Student Handbook. Academic Honesty: All Elon PA students acknowledged their commitment to abide by the Elon Honor Code by signing the Honor Pledge during orientation. Students will sign an Honor Pledge (electronically or manually) each time an assignment is turned in or an examination is started to reaffirm their complete understanding of the Honor Code of Elon University and their affirmation that their work abides by that Code. Required Textbooks: 1. All first-year required textbooks. 2. Emergency Medicine – A Comprehensive Study Guide, Companion Handbook by Cline, 5th Ed. Library Resources: 1. Textbooks, reference books, journals, online electronic databases. Other Resources: 1. *Moodle: Please check the course site frequently for new announcements, updated schedules, assignments and other course communication. 2. Practicing physician assistants, physicians, allied health care providers and laboratory teaching aids 2 Revised 10/23/13 TOPIC LIST Cardiology Chest Pain Palpitations Dyspnea on exertion Orthopnea Edema Syncope Conduction disorders* Hypertensive emergencies Hypotension~ Heart failure Coronary heart disease⌃ Vascular disease Valvular disease Acute/Subacute bacterial endocarditis Pericardial effusion Musculoskeletal Pain Swelling/deformity Ecchymosis/erythema Fractures/dislocations (shoulder, forearm/wrist/ hand/, hip, knee, ankle/foot) Soft tissue injury Back strain/sprain Low back pain Cauda equina Herniated disk Osteomyleitis Septic arthritis EENT Vision loss Nasal congestion Sore throat Ear pain Vertigo Blepharitis Conjunctivitis Blow-out fracture Corneal abrasion/ulcer Dacryoadenitis Foreign body (eye, ear, nose) Glaucoma (acute angle closure) Hyphema Macular degeneration Optic neuritis Orbital cellulitis Papilledema Retinal detachment Retinal vein occlusion Otitis externa Acute otitis media Trauma/hematoma external ear Barotrauma/TM perforation Labyrinthitis Mastoiditis Acute sinusitis Epistaxis Acute pharyngitis (viral, Bacterial) Peritonsillar abscess Dental abscess Acute laryngitis Epiglottitis 3 Hematology Easy bruising Fatigue Aplastic anemia Hemolytic anemia Sickle anemia/crisis Clotting factor disorders Hypercoagulable states Thrombocytopenia Acute leukemia Neurology Vertigo Seizure Numbness/paresthesias Weakness/paralysis Loss of consciousness/ change in mental status Loss of memory Loss of coordination/ataxia Headache (migraine/cluster tension) Meningitis Encephalitis Transient ischemic attack Stroke Subarachnoid hemorrhage/ cerebral aneurysm Intracerebral hemorrhage Altered level of consciousness /coma Epidural/subdural hematoma Seizure disorders Status epilepticus Syncope Guillain-Barré syndrome Spinal cord injury Revised 10/23/13 TOPICS (cont’d) Gastrointestinal Abdominal pain Anorexia Nausea/vomiting Heartburn Jaundice Hematemesis Melena; bleeding per rectum Change in bowel habits/ diarrhea/constipation Esophagitis Mallory-Weiss tear Peptic ulcer disease Acute cholecystitis Cholangitis Acute hepatitis Acute pancreatitis Acute appendicitis Diverticular disease Ischemic bowel disease Inflammatory bowel disease/ toxic megacolon Obstruction (small bowel, large bowel, volvulus) Anal fissure Hemorrhoids Hernia (incarcerated/ Strangulated) Infectious diarrhea Dermatology Itching Rash Discharge Dermatitis (eczema, contact) Drug eruptions Stevens-Johnson syndrome Toxic epidermal necrolysis Bullous pemphigoid Lice Scabies Spider bites Viral exanthems Herpes zoster Cellulitis Erysipelas Impetigo Burns Urticaria Pilonidal disease Pressure sores Psychiatry Thought disorder Changes in mood Hallucinations Suicidal/homicidal ideations Depression Generalized anxiety disorder Panic disorder Post-traumatic stress disorder Substance abuse disorders Domestic violence Suicide Women’s Health Vaginal discharge Pelvic pain/dysmenorrhea Amenorrhea Dysfunctional uterine Bleeding Endometriosis Ovarian cysts Vaginitis Pelvic inflammatory disease Mastitis/breast abscess Spontaneous abortion Ectopic pregnancy Placenta previa Premature rupture of membranes Fetal distress Genitourinary Dysuria Hematuria Suprapubic/flank pain Incontinence Nephrolithiasis Testicular torsion Cystitis Epidiymitis Orchitis Prostatitis Pyelonephritis Urethritis Acute renal failure Glomerulonephritis Fluid and electrolyte disorders Acid/base disorders * Atrial fibrillation/flutter, supraventricular tachycardia, bundle branch block, ventricular tachycardia/fibrillation, premature beats ~ Cardiogenic shock, orthostatic hypotension ⌃ Acute MI, (non-ST/ST segment elevation), angina pectoris, unstable angina, Prinzmetal/variant angina) Aortic aneurysm/dissection, arterial occlusion/thrombosis, phlebitis Aortic stenosis, aortic regurgitation, mitral stenosis, mitral regurgitation 4 Revised 10/23/13 Assessment Activities: End of rotation exam (25%), Preceptor Evaluation (65%), Professionalism (10%). Grade Scale and Grade Points Percentage 89.50-100 85.50-89.49 79.50-85.49 75.50-79.49 69.50-75.49 Below 69.50 There is no rounding of grades. Letter Grade A B+ B C+ C U Grade points 4.0 3.3 3.0 2.3 2.0 0 Note: For further information regarding academic standing in the Department of Physician Assistant Studies, please see the Student Handbook. Grading Criteria: 1. Demonstrate acquisition of a strong basic science and medical science knowledge base as demonstrated on the written examination/quizzes. 2. Demonstrate satisfactory self-directed learning skills, clinical reasoning skills, commitment to patient-centered care and professionalism as evidenced by satisfactory performance on the preceptor evaluation. 3. Demonstrate a commitment to learning and professionalism by actively participating in all clinical activities and exceeding the professional behavior standards and minimum requirements for clinical rotations available in the Elon PA Student Handbook. Instructional Objectives: 1. Clinical Skills: a. Elicit an appropriate complete or partial history from the patient or third party should the patient be a child or unable to supply a complete history. b. Perform a methodical, rapid, comprehensive, and accurate immediate assessment of patients presenting to the emergency department with life threatening emergencies. c. Perform a methodical, rapid, comprehensive, and accurate secondary assessment of patients presenting to the emergency department. 2. Given a patient or appropriate historical, physical or laboratory data and considering variables such as patient age, pregnancy and other factors that would alter the approach to or treatment 5 Revised 10/23/13 3. 4. 5. 6. 7. 8. 9. 10. 11. of a patient, be able to diagnose and initiate treatment for the presentations and/or diagnoses listed in the Topic List. Communicate with the supervising physician regarding the patient’s emergency status as soon as possible Apply basic techniques of CPR a. Establish and airway b. Initiate or sustain effective ventilation c. Perform external cardiac massage Be trained in ACLS and able to assist the medical team with cases in which advance life support is required. Know the indications and complications associated with individual ACLS protocols. Understand the indications and use of standard emergency medications and recommend appropriate administration recognizing situations in which dosing regimens are modified based on individual patient characteristics as in pediatric and geriatric patients and women of reproductive age. Be familiar with triage procedures in mass casualty situations. Perform the following procedures: a. Initiate IV therapy using sterile technique and universal precautions b. Insert and remove a nasogastric tube c. Insert and remove a urinary bladder catheter d. Obtain bacteriologic, viral, fungal and antigen detection cultures e. Participate in the placement of a central catheter Perform and interpret the following laboratory procedures a. Venipuncture for complete blood count, chemistry panels b. Arteriopuncture for arterial blood gases c. 12 lead EKG For each of the following procedures be able to discuss the indications, contraindications, complications, equipment needed, and proper technique a. Defibrillation b. Chest tube insertion c. Venous cutdown d. Thoracentesis e. Paracentesis f. Lumbar puncture g. Joint aspirations h. Tracheostomy i. Cast and splint application j. Endotracheal intubation k. Intra-osseous (I/O) access Perform the following clinical procedures under responsible physician supervision a. Cleansing and debridement of wounds b. Administration of local infiltrative anesthesia, or digital blocks as appropriate c. Determination of major vessel, nerve or tendon involvement d. Proper suturing of the laceration including using sterile technique and observing universal precautions e. Use of steri-strips or Dermabond f. Drainage of abscesses g. Application/changing of surgical dressings h. Removal of sutures and staples 6 Revised 10/23/13 i. Assess for need to administer tetanus booster 12. Given a patient or simulated model demonstrate the correct manner to splint a fracture or soft tissue injury 13. Be able to recognize the following for the given radiologic study: a. AP/Lateral view of bone: fracture, dislocations, osteolytic and osteoblastic lesions, osteoporosis, degenerative changes b. Flat plate and upright of abdomen: free intraperitoneal air, air/fluid levels within the bowel, intra-abdominal calcification, psoas shadows, nonspecific abdomen, dilated intestine c. Chest PA/Lateral: pulmonary infiltrates, pulmonary nodules, atelectasis, cardiomegaly, rib fractures, widened mediastinum, pleural effusions, normal chest x-ray. 14. Present to the physician a brief synopsis of the patient’s present illness, pertinent positive and negative findings and the diagnostic and therapeutic regimen recommended. 15. Counsel patient and family regarding the health problem including incorporating the patient and family’s perspective with the medical explanation of the disease process, therapy and its rationale, therapeutic options, prognosis and health care services available. 16. Document the patient visit in an problem oriented manner to include a. Presentation and history of present illness b. Pertinent past and family medical history c. Medications and allergies d. Physical examination findings e. Lab and diagnostic study results/interpretation f. Assessment and management plan g. Follow-up plans/appointments 17. Arrange for discharge or transfer from the emergency department 18. Communicate effectively with the patient, the attending physician and the receiving health professional assuring a smooth and complete transfer of care. 7 Revised 10/23/13