Primary Care Rotation Syllabus
advertisement

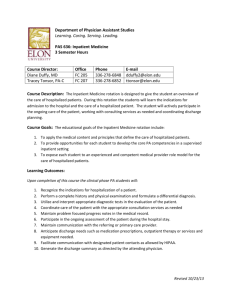
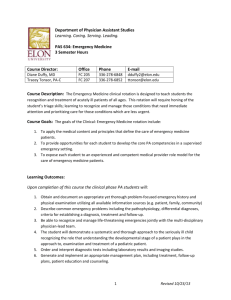
Department of Physician Assistant Studies Learning. Caring. Serving. Leading. PAS 630: Primary Care 3 Semester Hours Course Director: Diane Duffy, MD Tracey Tonsor, PA-C Office FC 205 FC 207 Phone 336-278-6848 336-278-6852 E-mail dduffy2@elon.edu ttonsor@elon.edu Course Description: The Primary Care rotation is designed to give students exposure to the spectrum of adult outpatient medical practice. Students will learn the principles of routine (well) care, management of acute illnesses, and management of chronic/multiple diagnoses. Course Goals: The educational goals of the Clinical: Adult Medicine Outpatient rotation include: 1. To apply the medical content and principles that define the care of primary care patients. 2. To provide opportunities for each student to develop the core PA competencies in a supervised primary care setting 3. To expose each student to an experienced and competent medical provider role model for the primary care of patients. Learning Outcomes: Upon completion of this clinical rotation clinical phase PA students will: 1. Demonstrate the ability to obtain accurate and complete information via the patient interview and conduct an appropriate physical examination for the various types of visits seen in adult outpatient medicine. 2. Demonstrate the ability to apply principles of clinical epidemiology and probabilistic reasoning to develop preliminary assessments/diagnoses and treatment plans. 3. Demonstrate familiarity with the common clinical presentations, physical exam findings, appropriate diagnostic tools and evidence-based treatments for common adult medicine patient problems including acute and chronic medical problems, common mental health problems and emotional illnesses. 4. Demonstrate familiarity with preventive care recommendations for promotion of health in the adult patient, identifying risks for specific illnesses that affect screening and treatment strategies. 5. Demonstrate the ability to effectively communicate with patients and other medical providers. 6. Demonstrate awareness of the impact of culture, ethnicity, socioeconomic status, advancing age and gender on the patient’s expression of illness and response to treatment, and demonstrate ability to incorporate that awareness into patient interactions. 7. Demonstrate proficiency in documenting medical care 8. Participate in and analyze the process of referral/consultation of a patient. 1 Revised 10/23/13 9. Recognize clinical processes established to improve performance of a clinical site. Teaching Methodologies: The content of this module will be presented through a variety of methods that include observation and participation at the clinical site, independent reading and participation in online activities developed to guide experiential learning. Accommodations: Students requiring academic accommodations must follow the “Academic Support” policy in the Elon University DPAS Student Handbook. Academic Honesty: All Elon PA students acknowledged their commitment to abide by the Elon Honor Code by signing the Honor Pledge during orientation. Students will sign an Honor Pledge (electronically or manually) each time an assignment is turned in or an examination is started to reaffirm their complete understanding of the Honor Code of Elon University and their affirmation that their work abides by that Code. Required Textbooks: 1. All required first year text books 2. Clinician’s Pocket Reference, 11th Edition (Paperback) 3. The Washington Manual of Medical Therapeutics, 33rd Edition (Paperback) Other Resources: 1. *Moodle: Please check the course site frequently for new announcements, updated schedules, assignments and other course communication. 2. Practicing physician assistants, physicians, allied health care providers and laboratory teaching aids. 2 Revised 10/23/13 TOPICS LIST Urgent Care Respiratory failure/arrest Deteriorating mental status/ unconscious patient Allergic reaction/anaphylaxis Acute abdomen Burns Third trimester bleeding Bites/stings Foreign body aspiration Cardiac failure/arrest Fractures/dislocations Sprains/strains Myocardial infarction Hypertensive crisis Pulmonary embolus Pneumothorax Ingesting harmful substances (poisoning) Orbital cellulitis Pulmonary Asthma Bronchitis COPD Pneumonia Tuberculosis Lung cancer Sleep disorders Tobacco use/dependence Cardiovascular Hypertension Coronary artery disease Peripheral vascular disease Arrhythmias Endocarditis Hyperlipidemia Hypertriglyceridemia Angina Congestive heart failure Chest pain Valvular disease Dermatology Dermatitis (eczema/ seborrhea) Nummular eczema Dyshidrosis Lichen simplex chronicus Drug eruptions Lichen planus Pityriasis rosea Psoriasis Erythema multiforme Stevens-Johnson syndrome Toxic epidermal necrolysis Bullous pemphigoid Acne vulgaris Rosacea Actinic keratosis Seborrheic keratosis Lice Scabies Spider bites Basal cell carcinoma Kaposi sarcoma Melanoma Alopecia Onychomycosis Paronychia Condyloma acuminatum Exanthems Molluscum contagiosum Verrucae Cellulitis Erysipelas Impetigo Acanthosis nigricans Hidradenitis suppurativa Lipomas/epithelial inclusion cysts Melasma Pilonidal disease Pressure ulcers 3 Dermatology (cont’d) Urticaria Vitiligo Folliculitis Tinea infections Tinea versicolor EENT Pharyngitis/tonsillitis Acute/chronic sinusitis Aphthous ulcers Blepharitis Conjunctivitis Dacryocystitis Hordeolum Labyrinthitis Tinnitus Laryngitis Otitis externa Otitis media Tympanic membrane perforation Ectropion Entropion Corneal abrasion Corneal ulcer Glaucoma Hyphema Macular degeneration Papilledema Pterygium Retinal detachment Retinopathy Cholesteatoma Ménière disease Allergic rhinitis Epistaxis Nasal polyps Peritonsillar abscess Paritotis Sialadenitis Revised 10/23/13 TOPICS LIST (cont’d) Infectious diseases Mononucleosis Lyme disease HIV Influenza Meningitis Salmonellosis Shigellosis Gastrointestinal Colorectal cancer/ colonic polyps Anal fissure Peptic ulcer disease Gastritis Gastroenteritis Diarrhea/constipation Pancreatitis Inflammatory bowel disease Appendicitis Gastrointestinal bleeding Hemorrhoids Bowel obstruction Viral hepatitis Jaundice Cholecystitis/cholelithiasis Cirrhosis Giardiasis and other parasitic Infections Hiatal hernia Gastroesophageal reflux disease Irritable bowel syndrome Esophagitis Hematology Anemia Leukemia Thrombocytopenia Clotting disorders Lymphomas Polycythemia Genitourinary Hernias Cystitis Pyelonephritis Glomerulonephritis Nephrolithiasis Benign prostatic hypertrophy Prostatitis Epididymitis Gonorrhea Chlamydia Urethritis Orchitis Balanitis Testicular cancer Reproductive system Dysmenorrhea Dysfunctional uterine bleeding Vaginitis Pelvic inflammatory disease Breast mass Breast cancer Cystocele Rectocele Menopause Intrauterine pregnancy Contraception Cervical cancer Spontaneous abortions Endocrinology Diabetes mellitus Adrenal insufficiency Cushing disease Hyperthyroidism Hypothyroidism Musculoskeletal/ Rheumatology Acute and chronic lower back pain Costochondritis 4 Musculo/Rheum (cont’d) Rheumatoid Arthritis Reactive arthritis Osteoarthritis Gout Sprains/strains Ganglion cysts Systemic lupus erythematosus Osteoporosis Fibromyalgia Plantar fasciitis Overuse syndrome Bursitis/tendonitis Neurology Dizziness Vertigo Syncope Seizure disorders Transient ischemic attack Cerebral vascular accident Alzheimer’s disease Parkinson’s disease Essential tremor Bell’s Palsy Dementia Delirium Headaches (cluster, migraine tension) Psychiatry/Behavioral Science Depression Generalized anxiety disorder Panic disorder Phobias Post traumatic stress disorder Insomnia Anorexia Bulimia Mood disorders Substance abuse disorders Domestic violence Suicide Revised 10/23/13 Assessment Activities: Exams/quizzes (25%), Preceptor Evaluation (65%), Professionalism (10%). Grade Scale and Grade Points Percentage 89.50-100 85.50-89.49 79.50-85.49 75.50-79.49 69.50-75.49 Below 69.50 There is no rounding of grades. Letter Grade A B+ B C+ C U Grade points 4.0 3.3 3.0 2.3 2.0 0 Note: For further information regarding academic standing in the Department of Physician Assistant Studies, please see the Student Handbook. Grading Criteria: 1. Demonstrate acquisition of a strong basic science and medical science knowledge base as demonstrated on the written examination/quizzes. 2. Demonstrate satisfactory self-directed learning skills, clinical reasoning skills, commitment to patient-centered care and professionalism as evidenced by satisfactory performance on the preceptor evaluation. 3. Demonstrate a commitment to learning and professionalism by actively participating in all clinical activities and exceeding the professional behavior standards and minimum requirements for clinical rotations available in the Elon PA Student Handbook. Instructional Objectives: Upon completion of the clinical rotation clinical phase physician assistant students will be able to: 1. Clinical Skills a. Demonstrate the ability to obtain accurate and complete information via the patient interview in the following clinical situations: 1. An acute medical problem 2. A chronic medical problem. 3. A patient presenting with multiple problems. 4. Routine health care b. Demonstrate the ability to conduct a complete physical exam and a problem focused physical exam based on the stated reason for the visit. 2. Core Presentations 5 Revised 10/23/13 a. Acute Care: Differentiate among common etiologies based on the presenting symptom. Recognize “don’t miss” conditions that may present with a particular symptom. Elicit a focused history and perform a focused physical examination. Discuss the importance of a cost-effective approach to the diagnostic work-up. Describe the initial management of common and dangerous diagnoses that present with a particular symptom. For the following: i. Upper respiratory symptoms ii. Joint pain and injury iii. Pregnancy (initial presentation) iv. Abdominal pain v. Common skin lesions vi. Common skin rashes vii. Abnormal vaginal bleeding viii. Low back pain ix. Cough x. Chest pain xi. Headache xii. Vaginal discharge xiii. Dysuria xiv. Dizziness xv. Shortness of breath/wheezing xvi. Fever xvii. Depression (initial presentation) xviii. Male urinary symptoms/prostate xix. Dementia xx. Leg swelling b. Chronic disease management: Apply diagnostic criteria. Elicit a focused history that includes information about adherence, self-management, and barriers to care. Perform a focused physical examination that includes identification of complications. Assess improvement or progression of the chronic disease. Describe major treatment modalities. Propose an evidence based management plan that includes pharmacologic and non-pharmacologic treatments and appropriate surveillance and tertiary prevention. Communicate appropriately with other health professionals. Document a chronic care visit. Communicate respectfully with patients who do not fully adhere to their treatment plan. For the following: i. Multiple chronic illnesses (e.g., depression, hypertension, hypothyroidism, type 2 diabetes mellitus) ii. Hypertension iii. Type 2 diabetes mellitus iv. Asthma/chronic obstructive pulmonary disease v. Hyperlipidemia 6 Revised 10/23/13 vi. Anxiety vii. Arthritis viii. Chronic back pain ix. Coronary artery disease x. Obesity xi. Heart failure xii. Depression (previously diagnosed) xiii. Osteoporosis/osteopenia xiv. Substance use, dependence, and abuse c. Atypical presentation of disease: i. Identify physiologic changes of aging for each organ system and their impact on the patient, including their contribution to homeostenosis (the agerelated narrowing of homeostatic reserve mechanisms). ii. Generate a differential diagnosis based on recognition of the unique presentations of common conditions in older adults, including acute coronary syndrome, dehydration, urinary tract infection, acute abdomen, and pneumonia. 3. Understand the basis of health promotion and be able to apply the principles of primary, secondary and tertiary prevention. a. For women: elicit a full menstrual, gynecological and obstetric history b. For men: Identify issues and risks related to sexual function and prostate health c. Accurately identify clinical situations where life expectancy, functional status, patient preference or goals of care should override standard recommendations for screening tests in older adults. d. Accurately identify clinical situations where life expectancy, functional status, patient preference or goals of care should override standard recommendations for treatment in older adults. e. Assess and describe baseline and current functional abilities in an older patient by collecting historical data from multiple sources and performing a confirmatory physical examination. f. Develop a preliminary management plan for patients presenting with functional deficits, including adaptive interventions and involvement of interprofessional team members from appropriate disciplines, such as social work, nursing, rehabilitation, nutrition, and pharmacy. g. Identify and assess safety risks in the home environment, and make recommendations to mitigate these. h. Apply the stages of change model and use motivational interviewing to encourage lifestyle changes to support wellness (weight loss, smoking cessation, safe sexual practices, exercise, activity, nutrition, diet) i. Provide counseling related to health promotion and disease prevention. 7 Revised 10/23/13 j. Define and differentiate among types of code status, health care proxies, and advanced directives in the state where one is training. k. Discuss who should be screened and methods of screening for each of the following health conditions: i. Breast cancer ii. Cervical cancer iii. Colon cancer iv. Coronary artery disease v. Depression vi. Fall risk in elderly patients vii. Intimate partner and family violence viii. Obesity ix. Osteoporosis x. Prostate cancer xi. Sexually transmitted infection xii. Substance use/abuse xiii. Type 2 diabetes mellitus 4. Cognitive and Behavioral a. Define and distinguish among the clinical presentations of delirium, dementia, and depression. b. Formulate a differential diagnosis and implement initial evaluation in a patient who exhibits dementia, delirium or depression. c. In an older patient with delirium, urgently initiate a diagnostic work-up to determine the root cause (etiology). d. Perform and interpret a cognitive assessment in older patients for whom there are concerns regarding memory or function. e. Develop an evaluation and non-pharmacologic management plan for agitated demented or delirious patients. 5. Integrate the process of therapeutic review (review of current therapies and medications the patient is using) into each patient encounter regardless of the reason for the visit. a. Explain the impact of age-related changes on drug selection and dose based on knowledge of age-related changes in renal and hepatic function, body composition, and Central Nervous System sensitivity. b. Identify medication, including anticholinergic, psychoactive, anticoagulant, analgesic, hypoglycemic, and cardiovascular drugs that should be avoided or used with caution in older adults and explain the potential problems associated with each. Document a patient’s complete medication list, including prescribed, herbal and over-the –counter medications, and for each medication provide the dose, frequency, indication, benefit, side effects, and an assessment of adherence. 6. Demonstrate patient-centered communication skills: a. Setting a collaborative agenda with the patient for an office visit. b. Being able to elicit and attend to patients’ specific concerns 8 Revised 10/23/13 7. 8. 9. 10. c. Explain history, physical examination, and test results in a manner that the patient can understand. d. Clarify information obtained by the patient from such sources as popular media, friends and family, or the internet. e. Effectively incorporate psychological issues into patient discussions and care planning. f. Use effective listening skills and empathy to improve patient adherence to medications and lifestyle changes. g. Effectively describe the treatment plans for prevention and management of acute and chronic conditions to the patient and work to formulate plan with patient. h. Utilize motivational interviewing techniques with a patient to encourage behavior change i. Identify the psychological, social, and spiritual needs of patients with advanced illness and their family members, and link these identified needs with the appropriate interprofessional team members. Demonstrate proficiency in creating the medical record. Create progress notes for each of the following types of visits: a. Acute medical problem visit b. Chronic medical problem visit c. Visit for patient with multiple medical problems d. Preventive services visit Demonstrate proficiency in the referral/consultation process by a. Creating referral/consultation letter b. Analyzing the process of referral/consultation c. Determining the characteristics that contribute to a successful referral/consultation Describe the use of a quality improvement protocol within a practice and how the protocol might improve health care. Describe methods of monitoring compliance with preventive services guidelines. 9 Revised 10/23/13