2-page briefing document - Natural Digestive Healing

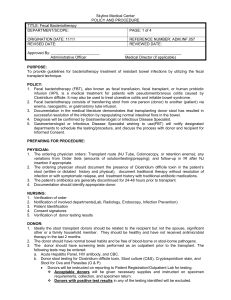
Bacteriotherapy
History
Fecal enema, or bacteriotherapy has been practiced in humans for over 50 years, and is established practice among veterinarians. It is commonly used to restore the ruminant capacity of ruminant animals (cows) who have lost the ability to digest cellulose due to antibiotic treatment. It was introduced as practice in humans in 1958 as an adjunct to pseudomembranous enterocolitis in the journal Surgery . Since then, it has been used intermittently, with success, for various forms of idiopathic colitis, IBS, and some microbial infections such as C. difficile .
The Theory
The efficacy of probiotic bacteria for Inflammatory Bowel has been established in the literature, though there are still questions about the efficacy of individual strains, and minimum therapeutic dosages are still being debated. However, there is a fundamental problem with current probiotic research for IBD: most research, and indeed most probiotic mixes use 1-8 different bacteria, but these bacteria are not ideal for several reasons.
(1) Bacteria, such as Lactobacillius and Bifidiobacterium , are specialized at milk digestion;
(2) These bacteria are not among the top 60 most abundant species found in the large intestine, such as anaerobes like Bacteriodes sp.
;
(3) The research shows that probiotic bacteria like Lactobacillius are transient in the gut.
That is, they do not establish themselves in the large intestine, and detectable levels disappear between 48 hours and 10 days after a person discontinues probiotic supplementation. It is likely that they are out-competed by resident bacteria in the large intestine. The effectiveness of probiotics as we know them only last while the patient is ingesting the bacteria through supplements.
But what if one affect a durable replacement of the altered community of someone with IBD
(stool samples from IBD patients consistently have ~25% fewer bacterial species than samples from gut-normal people) with a full spectrum of bacteria from someone who is disease-free?
Case Studies and Results
Case studies for bacteriotherapy for colitis have been reported in 17 peer-review publications to date. These case studies document the therapeutic effects of the fecal transplant on 150 patients. In the overwhelming majority of these cases, bacteriotherapy resolved the colitis for the entire follow-up period, which ranged from 10 days to 13 years. Many, many subjects have gone years without manifesting any signs of colitis, and without needing any treatment at all.
Risks
Donors are extensively screened prior to donating stool. No adverse health effects have been reported in the literature. All papers refer to the low risk of bacteriotherapy as compared to steroids, immunosuppression, and surgery.
Protocols
Donor Screening :
Donors must be screened for viral, bacterial, and parasitic infections. They must also be screened for transmittable diseases. It is suggested that the donor’s lifestyle be screened via questionnaire also. Some have suggested that a close family member be chosen as the donor.
This is not necessary from a bacterial community standpoint (indeed, there have been
successful case studies using unrelated donors), but it reduces the need for screening, and reduces the risks of disease transmission.
A suggested screening protocol is below.
Full blood count
Liver function test
HIV, Hep A, B, and C; cytomegalovirus, Epstein-Barr, and Syphilis
Salmonella, shigella, Campylobacter sp., Aeromonas hydrophilia, Yersinia sp.,
Vibrio parahaemolyticus, Vibrio colerae, Candida albicans, enterohemorragic E. coli O157, and Clostridium difficile.
Protozoa (trophozoites and cysts), helminthes and Entamoeba histolytica,
Giardia lamblia, Cryptosporidium sp., Dientamoeba fragilis, Blastocystis hominis,
Ascaris lumbricoies , trematodes and tape worms
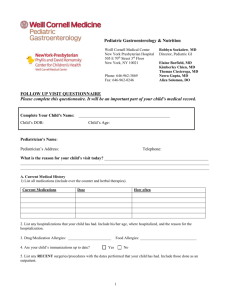
Patient
Reducing Colonization Resistance:
Antibiotics are used to reduce the bacterial load in the intestine, and to reduce the colonization resistance of the large intestine, thereby maximizing the opportunity for full recolonization of the colon.
Vancomycin, 500 mg bid (7-10 days)
Metronidazole, 400 mg bid (7-10 days)
Rifampicin 150 mg bid (7-10 days)
Preparation and Collection of Stool:
Fresh stool is collected from the donor daily in an airtight container. It is refrigerated immediately after collection, used within 6 hours of collection, and within10 minutes of preparation. 5-10 daily samples are required.
Stool is removed from its refrigerated container. 2-300 grams of stool is mixed with 2-
300 ml of distilled water or saline solution (1:1), using a blender to create a uniform suspension.
The sample is strained to remove undigested matter, and the remaining sample liquid is placed in a clean, disposable enema bag.
Administration of Donor Stool:
On the final day of antibiotics, and before administration of the first enema, the patient is prepped as if for colonoscopy. This further reduces the bacterial load in the colon, and removes stool that could act as a reservoir for the old bacterial community. Immediately after bowel movements have ceased from the prep, the first enema is given.
One enema is administered daily for a minimum of 5 days. 10 days is preferred.
Patients are encouraged to retain each enema for as long as possible (6-8 hours).