NBNPLC Quality Committee Annual Report June 2015
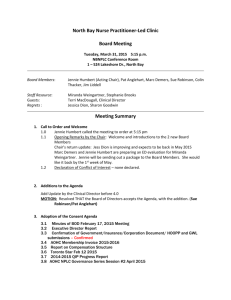
North Bay Nurse Practitioner-Led Clinic
Quality Improvement Committee
Annual Report DRAFT
June 16, 2015
The NBNPLC, through the provision of primary health care services, promotes optimal health for those living with chronic disease and for families with young children
C ollaboration
I ntegrity
R espect
I nnovation
H olistic
P articipation
Membership: Jennie Humbert, Chair, Sharon Goodwin (until April 2015), Marc Demers, Patricia
Anglehart (beginning May, 2015)
Staff Support: Miranda Weingartner, Leeann Whitney
Quality Improvement Plan
The North Bay NPLC continues to be aligned with the Ontario Ministry of Health’s four pillars of quality care in primary health care settings: Access, Integrated, Patient Centred, and
Population Health.
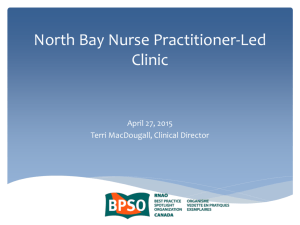
Access
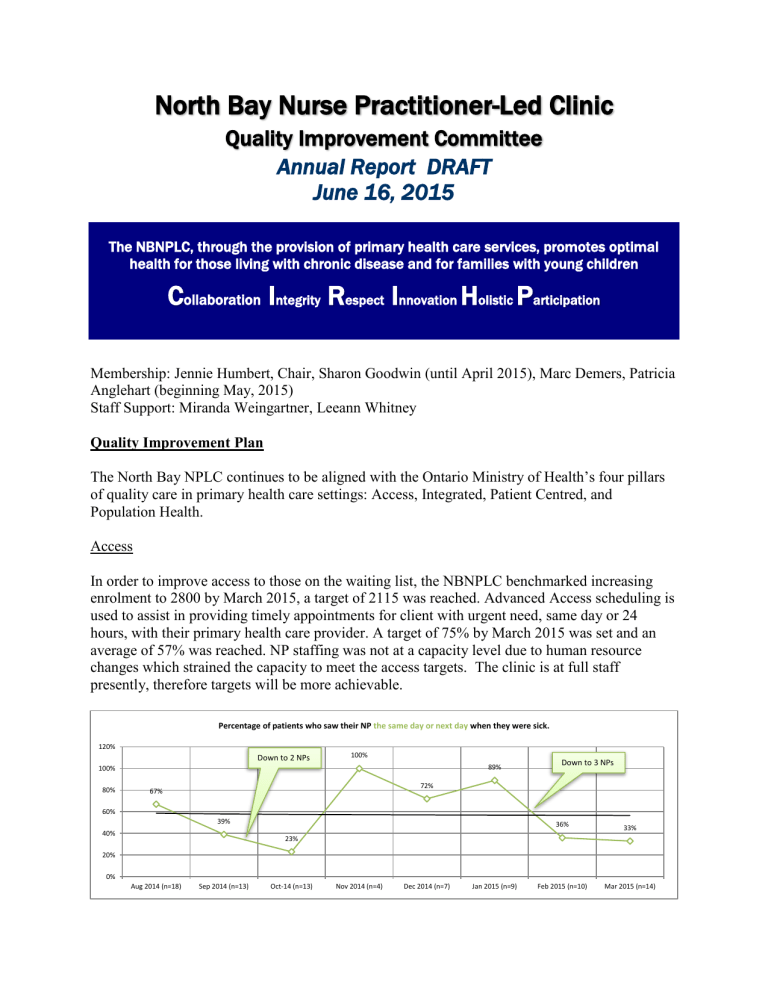
In order to improve access to those on the waiting list, the NBNPLC benchmarked increasing enrolment to 2800 by March 2015, a target of 2115 was reached. Advanced Access scheduling is used to assist in providing timely appointments for client with urgent need, same day or 24 hours, with their primary health care provider. A target of 75% by March 2015 was set and an average of 57% was reached. NP staffing was not at a capacity level due to human resource changes which strained the capacity to meet the access targets. The clinic is at full staff presently, therefore targets will be more achievable.
Percentage of patients who saw their NP the same day or next day when they were sick.
120%
100%
Down to 2 NPs
Down to 3 NPs
100% 89%
72%
80% 67%
60%
39%
36%
33%
40%
23%
20%
0%
Aug 2014 (n=18) Sep 2014 (n=13) Oct-14 (n=13) Nov 2014 (n=4) Dec 2014 (n=7) Jan 2015 (n=9) Feb 2015 (n=10) Mar 2015 (n=14)
Integrated
A target of 90% was set for the clients who were to see their primary care provider within 7 days after discharge from hospital, a target of 42% was reached. Processes are being put into place with the hospital so discharge reports are sent to the PHC provider. Then an appropriate health team member will follow-up with the client post discharge.
The challenge is meeting these targets without negatively impacting access. A post-discharge protocol is now in place, whereby a licensed professional follows-up with the patient postdischarge to determine what follow-up is most effective to keep them from being re-admitted.
An inter-professional team bands together around the patient to provide the best possible care: registered nurse, pharmacist, social worker, physician and nurse practitioner all working together for the patient. Communication is facilitated between the specialists/agency and the clients referred. Client follow-up takes place after the referral visit. These strategies will help to meet targets.
Already these new processes are paying dividends. Since February 2015, our numbers have improved two-fold to 86%.
Patient-Centred
Patient care surveys continue to indicate a high satisfaction with care. The three indicators given to track this priority are the extent to which the patients are given the opportunity to ask questions, to participate in decisions regarding their care; and the extent to which patients feel the NP has spent enough time with them.
Percentage of survey respondents who report that they NP always or often gives them the opportunity to ask questions.
110%
100%
90%
80%
70%
60%
50%
100%
83%
92%
84%
75%
100% 100% 100% 100%
Percentage of survey respondents who report that their NP always or often involves them in decision regarding their care.
110%
100%
90%
80%
70%
60%
50%
100%
78%
83%
100% 100%
84%
78%
90%
100%
110%
100%
90%
80%
70%
60%
50%
83%
Aug 2014 (n=17)
77%
When you see your NP, do they spend enough time with you?
100% 100% 100%
85%
Sep 2014 (n=13) Oct 2014 (n=13)
75%
Nov 2014 (n=4) Dec 2014 (n=7) Jan 2015 (n=9)
93%
Feb 2015 (n=10) Mar 2015 (n=14)
Population Health
Population health initiatives for primary prevention, such as influenza vaccinations for elders over 65, breast, cervical and colorectal cancer screening are integrated into patient care.
Processes for consistent documentation in the EMR have been put into place so data can be extracted to provide accurate achievement of targets.
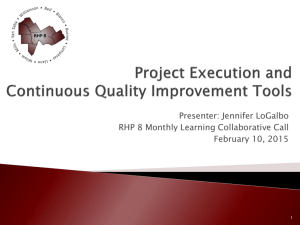
Quality Monitoring
Quality is being monitored in our organization using a Balanced Score Card, and BPSO Reports.
These are some excellent tools to provide the board with outcomes of quality indicators.
Risk Management
A Risk Response Map, a tool to assess the impact of an incident or potential incident, the action and level of involvement required to address the incident will be created and brought to the
Strategic Planning meeting on October 2015 for discussion.
Compliance with Privacy Legislation
A NBNPLC Research policy was drafted and approved by the board.
RNAO BPSO
NBNPLC is in the third year of participation in the RNAO Best
Practice Spotlight Organization candidacy.
Six Best Practice Guidelines have been incorporated into the clinic practice with excellent outcome.
Integrating Smoking Cessation into Nursing Practice
Assessment and Management of Pain
Strategies in the Self-Management of Chronic Disease Management
Interventions in Post Partum Depression
Woman Abuse Identification and Early Intervention
Working as a Collaborative Team
Quality Reporting
Quality indicator outcomes will be reported to the board on a quarterly basis as part of the consent agenda. The QIP Committee of the board will meet annually prior to the AGM and provide an annual report. The committee will meet on an ad hoc basis should an issue arise which the committee needs to address.
Respectful Submitted,
Jennie Humbert, Chair NBNPLC Quality Committee
June 16, 2015