Day One - In Sharper Focus * Part One
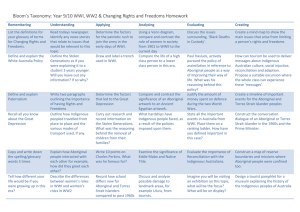
advertisement

Day One - In Sharper Focus – Part One CATH HALPERT: Tell me when I’m right to go. (INAUDIBLE) CATH HALPERT: Okay. Welcome, everybody. We might get started with this session. So welcome to this In Sharper Focus session, which is focusing on Indigenous Australians and what DisabilityCare might mean for them. I’m Cath Halbert. I’m the General Manager of Services Integration in DisabilityCare Agency in Canberra. First up, I would just like to acknowledge the traditional owners on whose land we’re meeting today - as many others have - and to pay my respects to the Elders past and present. This afternoon, we have got about an hour to focus on some Practical Design Fund projects, which have a particular focus for Indigenous Australians, or a very strong relevance for Indigenous Australians. We have got six presenters to get through, each will get about 10 minutes. As I understand, we’ll then go to the break, we’ll come back for the yarning session and then we’ll have questions and answers about the Practical Design Fund projects in the second session. So people can remember to write down their questions, so they don’t forget them. Given the limited time, I won’t go through the full list. I will just introduce each one at a time. The first Practical Design Fund project we’re going to look at is done by integratedliving Australia. We have Indra Arunachalam to present for us. Thanks, Indra. (APPLAUSE) INDRA ARUNACHALAM: Thank you. DisabilityCare culturally appropriate support services for Indigenous Australians with a disability. Why culturally appropriate disability care? Indigenous Australians have considerably higher rates of disability. It is more than 2.2 times the rate experienced by nonIndigenous Australians with a profound or severe core activity limitation. This is driven by factors such as the social and economic disadvantage as well as exposure to a range of risk factors. Some of the functions of DisabilityCare, such as early intervention and prevention of risk approaches can contribute towards closing this gap and reducing the disadvantage experienced by Indigenous Australians. However, Indigenous Australians face greater barriers to accessing disability support. This underutilisation is mainly due to social marginalisation, concern about approaching government agencies, cultural attitudes towards disability, services that are not culturally sensitive, and the remoteness of Indigenous population distribution. 25% of Indigenous people, versus 1% of non-Indigenous people, live in remote Australia. So how can we as providers help address this gap? We engaged First Peoples Disability Network to ask Indigenous people with disability, their carers and kinship group members what was actually working for them in the current system and what was not working for them. We also asked how we can make it happen for them. The first thing they identified was that they were really frustrated with the current system that is overly complex and inflexible to Indigenous needs. They said things like it is difficult to navigate and it’s not culturally sensitive. They have to deal with multiple agencies to obtain holistic support, and it is not easy to have a conversation with strangers. It’s not easy to paint the worst-case scenarios in order to obtain the required support. They also said that the current system is not supportive of solutions that are outside program guidelines. So basically, when we talked to them about DisabilityCare, that is truly person centred and a system that gives choice and control to the person with a disability, Indigenous people felt that this was a system that might work for them. Sorry, I’m still on the right slide. What they did suggest is that we actually need to disseminate information about DisabilityCare into Indigenous communities, through existing gatherings and networks. They suggested things like elder groups, community gatherings, stalls at sporting events, such as rugby league Koori knockout. They also suggested that we use multiple formats to distribute this information, such as social media, as well as storytelling. Past experience of Indigenous people has led to a general distrust of government agencies, and this is a critical access factor for DisabilityCare Australia to take into consideration when conducting assessment and planning of Indigenous people with disabilities. Many Indigenous consumers suggested that perhaps their existing providers, with whom they have a relationship, could advocate and support them to gain the full benefits of DisabilityCare. We engaged Corporate Culture - which is an Indigenous owned and operated organisation, building a sustainable Indigenous workforce - to ask Indigenous workers where we can find more Indigenous workers. They suggested we target mature age people reentering the workforce. Good recruitment sources suggested were local Indigenous communities, including Indigenous employment agencies and Aboriginal medical centres. This once again stresses the importance of engaging with your local community. The main reasons cited by Indigenous support workers for entering the disability sector were the desire to care for people in general, need to make Indigenous health a priority. And a wish to expand their skills and knowledge. The survey also indicated that Indigenous support workers stay in the sector for these three reasons, plus having a supportive supervisor, observing good community care practices that’s making a difference and having like-minded colleagues. We asked them why they would leave. Lack of Indigenous role models and mentors, lack of culturally supportive workplace and lack of cultural awareness about kinship matters, were listed. Better pay and other working conditions was actually only the fourth reason listed as to why they would leave. We asked them if there was one thing that they could change in the sector, what would that be? More than a third of the participants said that greater provision of services to Indigenous people. As you can see, we’re all on the same page. Finally, we engaged Corporate Culture to develop a cultural awareness training resource. This is to help service providers to increase cultural awareness among non-Indigenous staff so that we can provide culturally appropriate support services. The expected learning outcomes from this particular training package are insight into people from Indigenous background within the workplace, customers and communities. As well as practical back to work tools for staff who mentor and manage and work with Indigenous staff. The training resource has a session plan, as well as a PowerPoint presentation for you to use. It covers the following three elements. Cultural behaviour that may impact on delivering services to Indigenous people. It looks at the importance of land, family and kinship, ceremonies and separation of knowledge, men’s and women’s business. Historical perspective from exclusion to inclusion. To understand the present situation of Indigenous people, it is to understand the past. It explored policy considerations, assimilation, integration, self-determination, as well as poverty and prosperity cycle. Lastly, putting into practice covers disability-specific data, initiatives, and best practice. It looks at elements and strategies of cultural competencies, including engagement and effective communication. You can access these tools from our website after the 28th of June. The tools you can download are the actual Indigenous workplace survey, so you can use that tool to find out from our own cohort of Indigenous workers why they came, how to keep them, and how to develop them further. The cultural awareness training resource, like I said, it has got a session plan as well as a PowerPoint presentation, with actual facilitator notes within it so you can actually do this training in-house. However, I do suggest that it is delivered by an Indigenous person, just to give it good context. I mean, I can't do it. Other than that, thank you very much. (APPLAUSE) CATH HALPERT: I’m led to believe I can get this... That’s working? Good, thank you. Thanks very much, Indra. Very useful tool, I think you’ll all agree,, Indra has to rush off to another session but will be back for the question and answer session later on. Now we have Libby Massey, from the MJD Foundation, to present to us. Thank you. (Applause) LIBBY MASSEY: I'd like to start off today by also paying my respects to the Wurundjeri people, members of the Kulin nation and to say thank you for the opportunity to share with you our PDF project. I can’t say a lot in eight minutes, I’d probably like to, but I can say it’s been a privilege to have the opportunity to tell the story... I should probably show you some slides too, shouldn't I? Go back? FEMALE SPEAKER: Yep, if you click on... LIBBY MASSEY: They’re just pictures, really. It is actually a great privilege to have the opportunity to tell the story of people who live with disabilities in a very remote context. And to hopefully point to some of the facts and issues that will impact on the ability of these people to have control and choice, as are the aims of the DisabilityCare new system. Our Practical Design Fund disability audit was conducted in remote communities, very remote communities, across northeast Arnhem Land, and a little bit south through to Ngukurr. Our project was funded under the Practical Design Fund and it included the communities of: Angurugu, on Groote Eylandt. Umbakumba, also on Groote Eylandt. Milyakburra, which is nearby on Bickerton Island. Galiwin'ku, which is on Elcho Island. Ngukurr, which is on the mainland. And the tiny community of Urapunga, quite close to Ngukurr. While we would have liked to have the time and resources to look at the many other remote communities in the region, we simply didn’t, but we do hope that what we’ve been able to find through this disability audit is indicative of the issues that might be existing for those other communities. We conducted over 90 interviews with people with disabilities, with their carers, and with service providers across the region. To do this, we employed local community translators and mentors, and we worked with community service providers as well. We analysed published and unpublished data, such as census figures, the Disability Services National Minimum Data Set, FaHCSIA baseline data, ANU CAEPR reports, ABS stats, and as many other reports as we could get our hands on. I don't think any of the findings of this particular audit will be a surprise to anybody who has spent much time in the remote communities. The key issue was funding. All of the service providers who are currently providing funding in these remote communities stated that they didn’t have the funding to provide the very basic services they are intended to provide. This impacts on sector and workforce developments. It impacts on the ability of people to access services and it impacts clearly on equity. 80% of current funding for operational costs for community service providers at this point comes from aged care funding, and services are provided in a mixed manner. Of that funding, only 40% of those clients would have actually been technically frail aged. The rest of them would have a disability that was commensurate with DCA, having been acquired before the age of 65. There was no disability infrastructure, not vehicle, not building, in any of these communities that had been provided from the government disability source. Everything was aged care sourced funded. The same issues that are routinely raised about remote communities came up. Community infrastructure and housing were universally poor, and this has a huge impact on the quality of life for people with disabilities and their carers. There are no kerbs, there are no gutters, there’s very little access to community facilities. Homes are overcrowded and many of the people we interviewed lacked basic amenities, such as hot water, laundry facilities, or refrigeration in their homes. The scope of the disability services people currently have access to is extremely limited. Regardless of the disability profile of the person that we were interviewing, the services are firmly centred on low level attendant care. So people could access Meals on Wheels programs, for example, limited day access programs, and pretty much nothing else. In quite a few contexts, even their access to those programs was stymied by the lack of accessible transport. There’s no public transport in any of these communities and even the disability programs that were being funded didn’t always have an accessible vehicle to get people to their programs. If a vehicle was offline, people couldn’t access the program. Quite often, these vehicles need to be shipped off islands, to be repaired in a main centre. There’s no backup, there’s no spare vehicle, there’s nothing to replace it. So people just stopped getting their service. Respite was a huge issue in these communities. Respite is poorly understood and has become a de facto care provision scenario. It under-supports cares and is often used as a last resort emergency care after carer breakdown. A typical scenario is that a care situation reaches breaking point, and the client is sent off to a residential care facility, so the carer gets a break. Unfortunately, I could tell you a thousand stories of really unfortunate situations that arise. Respite needs to be used in its true context and it needs to be available to people, to keep informal care networks strong. It’s just not happening. There’s no overnight respite capacity or residential care capacity in any of the committees that we surveyed, people have to be transported to Darwin, usually by air, at great cost, and have to have their residential care component of their care suite hundreds of kilometres away from their families, in completely culturally inappropriate situations. Disability education was a, probably an inaccurate term, but what we’ve found is that many people that we were surveying and talking to had no construct of disability as you or I would know it as professionals. They didn't understand their disability in the same context at all. This leads to a really significant inability to advocate for needs, in a system that has the word ‘disability’ in it. It is predicated on your understanding that you have a disability and that there are services for you. It’s a very limited scope of knowledge about what those services might be outside of these tiny, very remote communities. People just don't get to see what they might have access to. Traditionally, they have not advocated for themselves at all. There are lots of things, of course, to be considered in the rollout of the DCA. I think, in these very remote communities, we’re sort of at the pointy end of what is and isn't available. The cashed out consumer choice versus block funding model is obviously something to think about. For either of those models to work better, there need to be significant steps put into place to better resource the current service providers into work on workforce issues. We need to consider the concept of individual needs versus community needs and collective decision-making. Most of the communities that we work in, collective decision-making is an inherent part of how everything happens, not just for disability care, but people need to have the opportunity to involve all of the people that are important in their care and in their decision making in those decisions. The systems issues that need to be addressed before expanding services include those wellknown barriers of funding, on-costs in remote communities, including freight, the lack of infrastructure, staff housing, the complete lack of capital infrastructure for disability-specific services. The other big issue is eligibility criteria. Currently, people aged over 50 are considered aged in an Indigenous context. So there’s a crossover for people who have acquired a disability before the age of 65 who are Indigenous and are eligible for aged care services. In the current context, would probably receive more, if not less, appropriate services through the aged care model. I'm actually finished. (LAUGHS) (APPLAUSE) Thank you. CATH HALBERT: Thanks very much, Libby. Although some of that is not surprising, it’s extremely important to have all those challenges that we’ll face in remote Australia back, clearly on the table. (COUGHS). Excuse me. Now we have Brain Injury Australia. Yes, and I don’t have your name. I’ll have to ask you to introduce yourselves. You just have to... MALE SPEAKER: Who’s up first? CATH HALBERT: Brain Injury Australia. It’s confusing on the slide, sorry. You’re up next. Applause, we’re meant to be having now. (APPLAUSE) (LAUGHS) Hang on, what’s happened? Can a tech person help us retrieve our presentation? JENNIFER CULLEN: Thank you, Cath. Good afternoon, ladies and gentlemen, my name is Jennifer Cullen, and I’m a very proud Waka Waka woman from Queensland. And our project this afternoon is a consortium group - Brain Injury Australia and James Cook University. Before I commence, I too wish to acknowledge and pay respects to Aunty Pat and her wonderful welcome to her country this morning. And on behalf of our three project members, we wish to pay respects to our Elders past and present who have walked before us. And I also will to acknowledge Aunty Gayle Rankine, who’s in the room this afternoon, as chairperson of First Peoples Disability Network. But let’s not also forget our young ones. Our young ones who are growing up to be strong, black, and deadly, who are going to be the workforce and the leaders for our people, for DisabilityCare Australia. Now, I think I moved that and I didn’t mean to. Is that right, Anne? ANNE STEPHENS: I think so. JENNIFER CULLEN: Oh, I did. ANNE STEPHENS: It’s moving by itself. JENNIFER CULLEN: Let me go back. FEMALE SPEAKER: We’ve got too many options... (LAUGHS) JENNIFER CULLEN: I can’t see without my glasses, that’s probably the problem. Right. Oops, let me start again. Okay, there. Just to give you a little bit of background - and I know we have only got ten minutes, eight minutes - just to give you some context around why Brain Injury Australia, Synapse, and James Cook Uni decided to apply for the Practical Design Fund. What we have found in the work that we’ve been doing in Aboriginal and Torres Strait Islander community is a high level of prevalence and incidence around acquired brain injury. As you know, acquired brain injury is any damage that occurs to the brain after birth. Unfortunately, we don't know much, scientifically and empirically, about the levels of disability. Most of it is anecdotal and through our discussions with... I’m doing it again. Anne, you’ll drive that, please. And also through information that we have in talking to our people. One of the biggest issues that we found is around that the current assessment tools don't actually capture the needs for people with an acquired brain injury who are an Aboriginal and Torres Strait Islander. What we’re also finding is that the way that often an acquired brain injury presents leads to misdiagnosis, misrepresentation, and often we were finding a clinical pathway for our people with an acquired brain injury was very often either into the hospital setting or into the criminal justice. DisabilityCare presents an amazing opportunity for Aboriginal and Torres Strait Islander people. So for us as a group, and through discussions with other organisations, such as First Peoples Disability Network, we said it’s time for us to stand up and look at ways to develop assessment tools. But it was more than just that. You can have the right tools but you still need to have a framework in which to apply those tools culturally. We had three deliverables for our project. They were to develop or recommend culturally appropriate assessment tools that can assess functioning, cognitive impairment, and the care and support needs of Aboriginal and Torres Strait Islander Australians with an ABI. Also, look at developing best practice guidelines for engaging Aboriginal and Torres Strait Islander people. One of the things we heard very clearly amongst all the communities we visited was that Aboriginal people and Torres Strait Islander people are not a homogenous group. The way we operate and work within my community is different to how other Indigenous communities operate that we went to. That slide up there shows you the areas in which we consulted. We went to Redfern, Darwin, Palm Island...no, not Palm... Wujal Wujal, and into Cairns, and Thursday Island, and Darwin. We also looked at developing a support framework for the assessors. That was actually to have understanding around the skills that would be needed to engage with Aboriginal and Torres Strait Islander people. There are a number of very clear messages that actually came through to us. One, in terms of the current structure in which DisabilityCare is looking at, very clearly we heard from Aboriginal and Torres Strait Islander people and communities to build the workforce capacity to encourage Aboriginal and Torres Strait Islander people to become assessors. That’s because of a whole lot of reasons, but mainly because Aboriginal people will understand the structure, the kinship and relationships within those groups. They will also understand who to engage with and who not to engage with around some of those personal care questions. Over to Anne, to explain about the framework. Did I go too fast? I’m trying to get through quickly. ANNE STEPHENS: Well, we developed this framework, which we took the assessment and planning map that we saw in some of the documents as the NDIS legislation and consultation documents were coming through, and we adapted this so we would be providing a culturally appropriate, best practice way to engage with communities to do assessments for people with cognitive impairments. So, we looked first at entry into the system. We looked at the ‘no wrong door’ policies. So these are ways that people might get a referral into the NDIS. We then looked at that, assuming someone has entered into the system, an assessment planner, an LACO are willing to further develop their case, there needs to be some engagement with the community. So we felt that it was very important that the NDIS appropriately seek permission to contact the community, seek permission to enter the community, and liaise with service providers in the communities, who know that community, know those people and clients very, very well, and can be a good liaison and point of call for particularly non-Indigenous people who might not have a history or understanding of the community in which they’re entering. In our PDF toolkit is guidelines, which includes little diagrams like this, which we call our map. It’s a typical community and some of the services that you might find. The second stage of the assessment process is pre-assessment. Prior to an assessment, a certain process needs to be followed, where there’s mutually-convenient times to visit the prospective participant and their community, you do that with service providers. You contact the appropriate agencies in the community. You visit and undertake some formal assessment if you’re really scoping, building relationships, and importantly, doing this face-to-face. In our consultation, it was said to us over and over again that assessment should not be conducted by phone or Skype or any other way than face-to-face, in language and in the context of the community and family in which people are living. You then provide an opportunity for people to be actually assessed. There may be that after all that, what we hear from you, Libby, about the appalling lack of services on the ground, many families might not want to go through the process of having an assessment and being found whether they’re eligible or not. You need to provide that choice. If they do, they shouldn't be removed from the system. They need an opportunity to come back at a later time. Assuming they go on to be assessed, then there needs to be another face-to-face, where their goals and aspirations are taken into account. There’s a gathering of pre-assessments that may have to be done. So case histories. We developed an assessment toolkit, which we cannot talk about because we just don't have time. But we have a suite of instruments that are developed for this purpose, for acquired brain injury, and there may be occasion to seek further specialist assessment in doing that appraisal. They’re either deemed as eligible or they’re not. Either way, there needs to be a discussion with the individual and their families, the communities, about what the next step is. Again, we heard repeatedly, people want feedback and they want that in a timely fashion. There are some families that can wait up to 12 months to find out whether they’re eligible for support. For a child, and 12 months is a long time for kids. So, there’s a lot of issues around giving feedback. Anything else I need to add? This was a team. We have from Brain Injury, Doctor Derek Brooks, who’s in the audience. Of course, myself, I’m from JCU and Jennifer, it’s been an honour to work on this project. Our next step is to develop the cognitive assessment instruments further. We would like very much to undertake validation and reliability studies so we have very substantive to offer this sector. Thank you. (APPLAUSE) CATH HALBERT: Thank you very much, Jennifer and Anne. Very valuable and exciting work for Disability Care Australia. Now, I hope this is true, we’ve now have got Arafmi - Mike Seward and Faye Dean to present. Just Mike, perhaps. Thanks very much. (APPLAUSE) MIKE SEWARD: Thank you. Faye will be talking from the floor in a way that she’s comfortable. First of all, I wish to acknowledge the traditional elders of the land, the Wurundjeri people of the Kulin nation and to pay my respects to their Elders, past and present. And to acknowledge that this land is, has been, and always will be their Wurundjeri land. I’ve deliberately chosen not to have a PowerPoint presentation because I want you to focus on what I have to say. The copies of the guidelines you have and more importantly from a remote Aboriginal community in WA, my co-presenter, Fay Dean, from Bidyadanga Aboriginal community in the Kimberley. This project was to develop guidelines for service providers and family members of those eligible for tier three psychological DisabilityCare Australia services. You have a copy of those guidelines. We hired a project manager, Professor Alan Huggins, to go to remote Aboriginal communities, Broome and Canarvon, to speak to family members and service providers. It soon became apparent to Alan that what the community members wanted was to be listened to and have their wishes acted upon. Isn’t that exactly what the introduction of DisabilityCare Australia is all about? Empowering people to have their reasonable needs met. So what is it that the community members wanted? Faye will tell you that in more detail. In a nutshell it was: One, instead of relying on service providers providing services by visits, use modern technology like mobile phones, email, Skype, to provide services. Two, acknowledge that Indigenous people have their own ways of dealing with disability. And to embrace this, not ignore it, or worse still, actively discourage it. Three, use the Indigenous cultural family concepts, by including families in discussion around the needs of the DisabilityCare recipient. Four, what came through loud and clear was work with the community. Make life better for those DisabilityCare recipients and their families in the community. We can’t turn members of the community into psychiatrists, OTs, or the like, but what a service provider can do is train community members in frontline service provision. Someone in the community working for a service provider to provide exercise regimes, to provide mental health first aid for somebody experiencing mental anguish, and the like. Not only is it needed, it is wanted by communities. Indeed, last week, on Q&A, former Australian of the Year and living national treasure, Professor Fiona Stanley, said her 30 year journey working with Aboriginal people led her to just this, “Listen to what Indigenous people want and implement it.” This could be a change point. DisabilityCare Australia can and should do this. On this note, I would like to introduce Faye Dean to you. Faye is from Bidyadanga Aboriginal community, some 200 km from Broome. Rather than come up and lecture you, Western style, Faye will talk to you from the floor, in the way that’s comfortable for her. Faye. (APPLAUSE) FAYE DEAN: Hello, everybody. Hi, everybody. Like Mike says, I’m from Bidyadanga community. It’s a strong cultural community, 170 ks south of Broome. Concerns we have are mainly Indigenous health workers not trained to support people with disabilities. Also, community people not educated to understand disabilities instead isolate disabled people, even if it’s their own families. In a crisis point, there’s a... the police and the clinic have an argument about who makes first contact. While we’re screaming for help, you know...it’s terrible. (WHISPERS) What was it I wanted to say? FEMALE SPEAKER: (INAUDIBLE WHISPER) FAYE DEAN: The main thing is, like I said, I’m here to try and get the government to train our Indigenous health workers to support people with disabilities in our community. Thank you. (APPLAUSE) CATH HALBERT: Thank you very much, Mike and Faye, for that perspective. Now we have Fiona Green from Cooloola Human Services Network to present for us. Thank you very much. And we are going okay on time, thank you for all your timely presentations. FIONA GREEN: Thank you very much. I would like to acknowledge the traditional owners of the land in which we meet today. Whoops. I was the project consultant for the Gympie region NDIS transition project. This was a project that was auspiced by the Cooloola Human Services Network. We also have in the audience today Abbie Grant-Taylor, the president of the Cooloola Human Services Network, Emma Rice, the project liaison, and Dianne Hughes, who provided project support. In our project, I would like to acknowledge and thank the Aboriginal Elders of the Gubbi Gubbi nation and the other language groups of the Gympie region. And particularly everyone who contributed collective wisdom to our project, including people with disabilities, families, carers and service providers of the Gympie region. The Cooloola Human Services Network, for those who aren't aware, we’re a non-profit, Gympie-based body, in terms of support for human services in the Gympie region. And it’s the peak body in our region for that, for all human services. The vision of the Cooloola Human Services Network is about a responsive and inclusive community. It fitted really well with the whole idea of a Practical Design Fund project. So, Cooloola Human Services Network partnered with About Freedom - which is the organisation that I work for - to deliver the project in the Gympie region. Where is Gympie, for those that don't know? I can't imagine there is anyone that doesn't know where Gympie is! We’re about 160 km north of Brisbane. Gympie township is in the centre, and the region covers Rainbow Beach, Tin Can Bay, the western towns of Kilkivan and Goomeri, south into the Mary Valley, and Fraser Island is just off the coast. It’s a very nice place. So our project looked at how will people with disability and their families in rural and regional Australia be supported to understand their rights and responsibilities and entitlements under DisabilityCare and learn to navigate the system for their benefit. And how will Aboriginal and Torres Strait Islander people, particularly those who don’t currently access the service system, also be supported to understand their rights and entitlements under DisabilityCare. The key topics we looked at were around choice and control, issues for rural communities, and Indigenous participation. Our activities involved a number of discussion groups with people with disabilities, families and carers throughout our region, including Indigenous Australians. We met with 18 different groups, 18 different discussion groups were held. Originally, we thought we’d meet with 10, but the interest was so great in our community that we ended up meeting with 18 different groups. Meetings with local service providers. We thought we would meet around five at a minimum, and we ended up meeting with 22, again, because of the high levels of interest in DisabilityCare. Gathering peoples practical ideas. Instead of us coming up with the resource, we thought we would ask people what they thought about ways DisabilityCare could work in a rural community. Make recommendations about that and share those results. We’ve come up with a final report. The groups that we held were around the kitchen table with individual families in their own communities, larger groups in community halls - one at the Gympie Civic Centre - and also smaller groups around the region as well. We were interrupted by two major floods of the Mary River during the project. In January, we had Ex-Tropical Cyclone Oswald come by. That’s the Mary River, as it runs through Gympie. We had a flood peak of 20.3 metres. Disrupted our project a little bit. Postponed a couple of meetings, made the roads impassable for a while. We also had a second flood three weeks later in February. That’s one of the main streets of Gympie, with a well-known company's building underwater. So, what were the recommendations? We talked to the Aboriginal Elders of our community and Aboriginal and Torres Strait Islander workers in the community around what was important for Indigenous people. It’s interesting that our projects today have all been done very independently of each other, but the findings are quite similar. There are common themes coming through, I can see that. Providing information to local communities needs to be tailored and in culturally appropriate ways. That’s really specific information about what is DisabilityCare, how it might work, what’s the eligibility, how do I access it, what can and can't be purchased... all the really basic questions people need to know. We need to use Aboriginal and Torres Strait Islander Elders and community workers that people recognise and trust in the community to deliver that message and tell people about the system. We need to use Indigenous forums, network meetings, community events and festivals, yarning sessions to share personal stories about what is possible, Facebook and other social media. Service providers need to really develop genuine respectful partnerships with Aboriginal people. Listen and hear each other. And work together in a spirit of cooperation built on trust and goodwill. That came through very strongly from the Elders in our community. We need to display the Aboriginal flag on flyers and in service venues that do offer culturally-appropriate services. Flying the flag lets people know that the service is welcoming to Aboriginal people, it assists people to recognise a place they’ll feel safe and get the right kind of help. Services do need to walk the talk though and not just display the flag for tokenism. Across the sector, we need to employ more Aboriginal and Torres Strait Islander people as managers, project officers, coordinators, planners, support workers. Aboriginal people need to see a familiar face within organisations that they can trust. Over time, we need to provide information and advice for Indigenous families on how to manage their own funds in culturally appropriate ways. This needs to occur though, the message was, after people are familiar with the scheme and how it works. Then talk more specifically about self-management and funding and how that might happen in a culturally appropriate way, so that people aren’t set up to fail. Explore opportunities for funding and development of specific Aboriginal and Torres Strait Islander run services too. In our community, we don’t have that. I imagine in a lot of communities around Australia, we don’t have that. We also looked at issues more generally for rural Australia. What we found was that funding needs to take into account the extra costs of living with disability in rural, remote, and isolated areas of Australia. Transport and travel costs need to be included in the definition of reasonable and necessary supports. I'm pleased to see that’s in there. We need to remove the red tape. This is a very strong message from rural people everywhere I went. Remove the red tape and unnecessary barriers in place for accessing disability services. Particularly things like clear, simple to understand processes for claiming travel expenses, not the current systems we have operating in Queensland. Explore ways of pooling resources, or developing collectives between individuals and families in rural or more isolated areas, to increase the range of support options that might be then available to them. But, there is a word of caution on this recommendation, that if we’re encouraging people to pool their funds, we need to be mindful that we run the risk of reducing flexibility or losing the individually-tailored approach of supports. It’s a doubleedged sword that one, but it may mean the difference between a service coming to the community and not, if there is a number of people who need the same kind of service and they can pool their funds together to get that to come to their community. Services need to provide support to rural areas from within local communities, using local staff, rather than using an outreach model from larger regional centres, in order to provide authentic and credible service responses. This is a very strong message from the Gympie region. We’re in between two larger regions, the Sunshine Coast and the Wide Bay, and it’s a very sore point with a lot of people about the fact that outreach services from somewhere else are often used, and it doesn't necessarily provide the most ideal service. I know that’s probably the case for many other smaller communities across Australia. Local area coordinators within DisabilityCare need to be based in rural community, and not just larger regional centres. Existing federally defined geographical boundaries will be too large for local area coordinators to have that effective coverage of rural Australia. We need to provide incentives for service providers to visit people in their own communities, and in their own homes, rather than rural people having to travel all the time to services. We need to provide information in a variety of ways, not just rely on internet-based communication, given the comparatively low rates of internet access in rural Australia. For service providers, the key messages were around services needed to embed a culture of working collaboratively with families and other supports, rather than working in isolation or competition. Helping people develop skills to manage their own lives, and not take over their lives. And utilising and encouraging local neighbourhood supports and peer support networks wherever possible. We need to increase people’s expectations and knowledge about what is possible for people with disabilities into contemporary Australia. This includes the need to challenge old expectations of what people with disability can achieve. We need to ensure DisabilityCare interfaces strongly and seamlessly with education, employment and housing systems across Australia. We need additional resources to address the longstanding issues of poor accessibility of the build environment, in order to enhance social and economic participation. We need robust protocols for suppliers of specialist aids and equipment to prevent price gouging and ensure certainly of supply, maintenance, and repairs, for aids and equipment across Australia, particularly in rural and remote Australia. Our final report is available for download from the Cooloola Human Services Network website and, hopefully it will also be on the DisabilityCare website. There’s the webpage if you’d like to access a copy. Thank you very much. (APPLAUSE) CATH HALBERT: Thanks very much, Fiona. Again, some very valuable messages for the effectiveness and sustainability of the scheme. Lastly, and you’ve all been terribly disciplined, we are well within our time, we’ve got Ray Mines from Motivation Australia Development Organisation. Thank you. (APPLAUSE) RAY MINES: How do you follow five presentations like that? Okay. What do I need to do first? Motivation Australia is a small not-for-profit development organisation that works in partnership with local organisations to enhance the quality of life for people with mobility disabilities in the Asia-Pacific region and in remote Australia. The project team carried out discovery and education sessions in five communities in northeast Arnhem Land. They were all Yolngu communities and they were all considered to be remote or very remote communities. Libby has ably covered most of these barriers, so I will whip through these fairly quickly. Northeast Arnhem Land is geographically very remote from services. It’s generally an extreme physical environment. Systems are very complex. Buildings and transport is largely inaccessible. There’s a lack of durable assistive devices and there’s a general lack of empowerment for people with disabilities. Perhaps the largest barrier and the one we focused on in our Practical Design Fund project was the access to culturally and linguistically appropriate information. Our project dived deeply into Yolngu language and worldview about disability. What we found was that disability is an unfamiliar idea. The Yolngu are an intelligent people with a rich and sophisticated culture, possessing very deep knowledge about all aspects of life. But disability is a big word. It’s an umbrella word. It’s a collective noun for many very different conditions. It’s not only foreign in the way the Spanish ‘incapacidad’ or German ‘behinderung’ is to an English speaker, but the very concept of disability has no meaning for Yolngu and cannot be translated, because there are no equivalent words. In fact, the disability sector involves a great many concept words which do not translate into Yolngu languages. Yolngu have a different completely framework of worldview. In fact... Sorry. Getting ahead of myself. The way that Yolngu view and interact with the world is quite different to non-Aboriginal people. There’s a general lack of biomedical knowledge, including the details of many of the body's internal functions and health related cause-and-effect relationships. In what Richard Trudgen calls the Yolngu ‘cultural knowledge base’. Yolngu understanding is based on objective observations of the body. Yolngu relate much more easily to physical impairments which are observed on the outside of the body, therefore they have less knowledge in their cultural knowledge base about intellectual disability and mental illnesses. There continues to be a lack of effective communication between Yolngu and non-Aboriginal personnel. Basically, white fellas keep banging their head against the same wall. Information about disability has not been in a language or format that the Yolngu can understand. All of this leads to a general lack of understanding about their own disability and a lack of general knowledge within the community about disability. We feel that the first step in DisabilityCare Australia fulfilling its aspirations for Aboriginal and Torres Strait Islanders in a remote community has to be developing and telling foundational stories about individual disabilities. Our Practical Design Fund developed several processes, this being one of them. In order to make informed decisions, Aboriginal and Torres Strait Islander people are going to need accurate and detailed biomedical information about their disability in a language and format that they can understand. Culturally and linguistically appropriate information is needed, which explains the stories of disabilities in a way which is meaningful to Aboriginal people. The process of developing foundational stories in Aboriginal languages requires expertise built up over many years and detailed clinical knowledge. It takes time to generate these stories, ones which are meaningful and even longer... Sorry, an even longer time to develop ones which communicate foundational concepts to Aboriginal people. I'm not going to go through - because of time - the process in detail, but it’s an iterative process whereby after some research, we generate ideas with Yolngu and then basically try them, reflect on how it went, amend the story and go around again. This takes quite a lot of time before you can say you have something which has meaning. Motivation Australia are not a frontline service provider. Where we see our involvement is in assisting service providers and disability specific organisations to build local capacity and to develop an inclusive community approach to working in remote Aboriginal and Torres Strait Islander communities. Utilising tools like this to develop linguistically and culturally appropriate information. If anyone - well, I hope someone - would like a copy of this, I have a booklet and then on the table at the front, or you can come and see me and we can discuss it afterwards. One page too many. Lastly, but not least, I would like to acknowledge the Aboriginal Resources and Development Services Incorporated for their huge contribution to the project. They’re a Darwin-based organisation which we would not have been able to complete the project without. Also, I’d like to thank the Yolngu people with disabilities, their families, carers and elders, who discussed Yolngu language and worldview of disability with us. I’d like to assert the Yolngu ownership over the language and the cultural concepts contained in our material. The full report, including a list of all the recommendations, will be available on our website, and I hope on the DisabilityCare Australia website as well. Thank you very much. (APPLAUSE) CATH HALBERT: Thanks very much, Ray, for that very valuable variation on the theme but providing us with very, again, very useful information. We’ve come to the close of this more formal part of the session. I know people will be torn, because there are so many interesting concurrent sessions to be run from 3:45. We’re coming back for a less formal forum just to have a yarning discussion, but also for people to be able to put questions direct to the presenters that we have seen this afternoon, all of those very, very high-value projects that have already been completed. I think they’ve all been completed. So I hope as many of you as possible will come back to ask the questions, but we’ll now have a half an hour break, so make good use of it. Thank you.