Comprehensive Discharge Planning Gap Analysis
advertisement
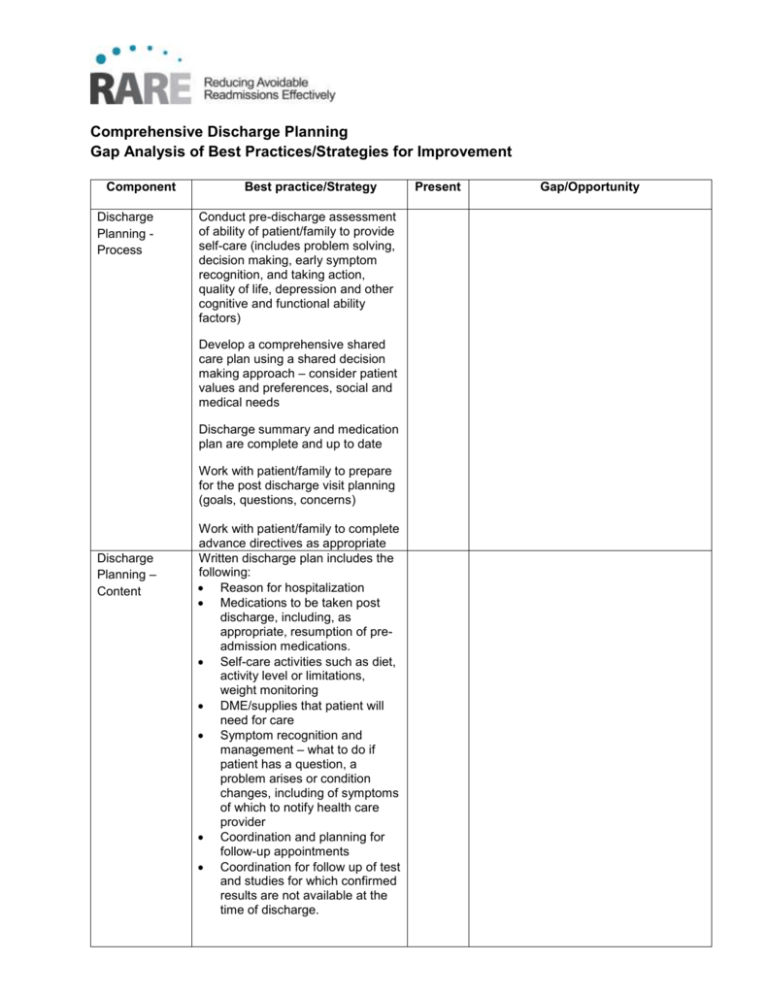
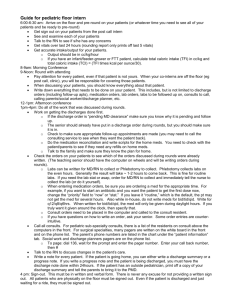
Comprehensive Discharge Planning Gap Analysis of Best Practices/Strategies for Improvement Component Discharge Planning Process Best practice/Strategy Conduct pre-discharge assessment of ability of patient/family to provide self-care (includes problem solving, decision making, early symptom recognition, and taking action, quality of life, depression and other cognitive and functional ability factors) Develop a comprehensive shared care plan using a shared decision making approach – consider patient values and preferences, social and medical needs Discharge summary and medication plan are complete and up to date Work with patient/family to prepare for the post discharge visit planning (goals, questions, concerns) Discharge Planning – Content Work with patient/family to complete advance directives as appropriate Written discharge plan includes the following: Reason for hospitalization Medications to be taken post discharge, including, as appropriate, resumption of preadmission medications. Self-care activities such as diet, activity level or limitations, weight monitoring DME/supplies that patient will need for care Symptom recognition and management – what to do if patient has a question, a problem arises or condition changes, including of symptoms of which to notify health care provider Coordination and planning for follow-up appointments Coordination for follow up of test and studies for which confirmed results are not available at the time of discharge. Present Gap/Opportunity Care Coordination Coordination of community resources patient will utilize, such as: o Home Health Care o Meals on Wheels o Adult Day Care o PT, OT, ST The written discharge plan should be easy to read: Include only essential education on health condition Utilize plain language - clear, straightforward expression, using only as many words as necessary Use universal principles of health literacy to specify readerfriendly written materials: simple words, large font, short sentences, short paragraphs, no medical jargon, headings and bullets, highlighted or circled key information, lots of white space, use visual aides Make appointments for follow-up and post-discharge testing, with input from the patient regarding time and date Use personal health records or patient portals so patients have access to necessary information (lab results, radiology results, request prescription refills, ability to email doctors, nurses, and staff with questions) All care providers have a complete discharge summary All care providers know their care roles and responsibilities Conduct post discharge telephone care management Health Literacy/ PatientProvider Communication Educate the patient about diagnosis throughout the care continuum Embed health literacy principles into all patient education and interactions Give the patient a complete and written discharge plan Employ teach back to ensure patients/families understand the care plan, information and explanations given and that their questions are answered Provide culturally and linguistically appropriate care Ensure continuity in care in order to build trust Use a shared decision making approach Ensure enough time is available for consultation Discuss with the patient any tests or studies that have been completed and who will be responsible for following up the results Confirm the medication plan with the patient Ensure provider contact and followup information is provided to the patient Review with the patient appropriate steps of what to do if a problem arises RARE Campaign www.rarereadmissions.org