MERS-CoV - Department of Health
advertisement
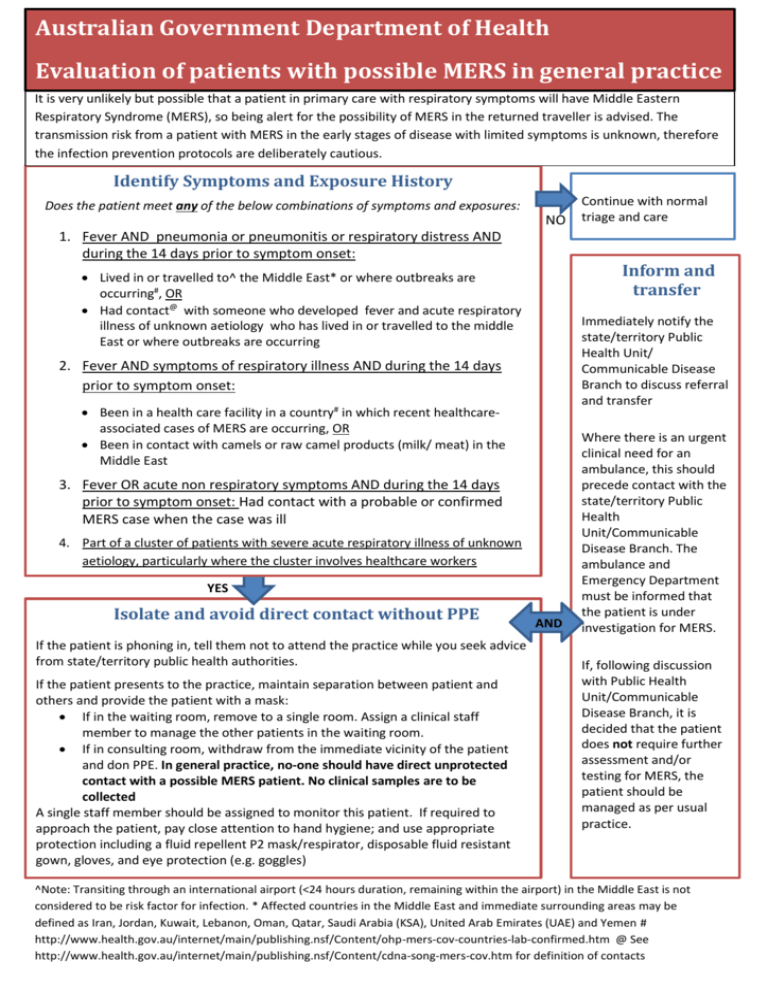
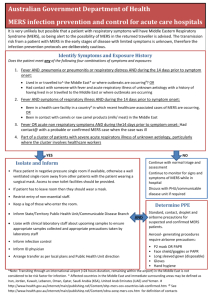
Australian Government Department of Health Evaluation of patients with possible MERS in general practice It unlikely but possible that a patient in primary care with respiratory symptoms will have Middle Eastern inis very Australia Respiratory Syndrome (MERS), so being alert for the possibility of MERS in the returned traveller is advised. The transmission risk from a patient with MERS in the early stages of disease with limited symptoms is unknown, therefore the infection prevention protocols are deliberately cautious. Identify Symptoms and Exposure History Does the patient meet any of the below combinations of symptoms and exposures: NO 1. Fever AND pneumonia or pneumonitis or respiratory distress AND during the 14 days prior to symptom onset: Inform and transfer Lived in or travelled to^ the Middle East* or where outbreaks are occurring#, OR Had contact@ with someone who developed fever and acute respiratory illness of unknown aetiology who has lived in or travelled to the middle East or where outbreaks are occurring Immediately notify the state/territory Public Health Unit/ Communicable Disease Branch to discuss referral and transfer 2. Fever AND symptoms of respiratory illness AND during the 14 days prior to symptom onset: Been in a health care facility in a country# in which recent healthcareassociated cases of MERS are occurring, OR Been in contact with camels or raw camel products (milk/ meat) in the Middle East 3. Fever OR acute non respiratory symptoms AND during the 14 days YES prior to symptom onset: Had contact with a probable or confirmed MERS case when the case was ill 4. Part of a cluster of patients with severe acute respiratory illness of unknown aetiology, particularly where the cluster involves healthcare workers YES Isolate and avoid direct contact without PPE If the patient is phoning in, tell them not to attend the practice while you seek advice from state/territory public health authorities. If the patient presents to the practice, maintain separation between patient and others and provide the patient with a mask: If in the waiting room, remove to a single room. Assign a clinical staff member to manage the other patients in the waiting room. If in consulting room, withdraw from the immediate vicinity of the patient and don PPE. In general practice, no-one should have direct unprotected contact with a possible MERS patient. No clinical samples are to be collected A single staff member should be assigned to monitor this patient. If required to approach the patient, pay close attention to hand hygiene; and use appropriate protection including a fluid repellent P2 mask/respirator, disposable fluid resistant gown, gloves, and eye protection (e.g. goggles) Continue with normal triage and care AND Where there is an urgent clinical need for an ambulance, this should precede contact with the state/territory Public Health Unit/Communicable Disease Branch. The ambulance and Emergency Department must be informed that the patient is under investigation for MERS. If, following discussion with Public Health Unit/Communicable Disease Branch, it is decided that the patient does not require further assessment and/or testing for MERS, the patient should be managed as per usual practice. ^Note: Transiting through an international airport (<24 hours duration, remaining within the airport) in the Middle East is not considered to be risk factor for infection. * Affected countries in the Middle East and immediate surrounding areas may be defined as Iran, Jordan, Kuwait, Lebanon, Oman, Qatar, Saudi Arabia (KSA), United Arab Emirates (UAE) and Yemen # http://www.health.gov.au/internet/main/publishing.nsf/Content/ohp-mers-cov-countries-lab-confirmed.htm @ See http://www.health.gov.au/internet/main/publishing.nsf/Content/cdna-song-mers-cov.htm for definition of contacts