module details
advertisement

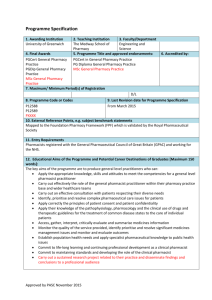
MODULE SPECIFICATION TEMPLATE MODULE DETAILS Module title Module code Credit value Level Mark the box to the right of the appropriate level with an ‘X’ Foundation Stage 1 “Practitioner Development and Establishment of Professional and Clinical Practice” CLM36 60 Level 4 Level 5 Level 6 Level 7 X Level 8 Level 0 (for modules at foundation level) Entry criteria for registration on this module Pre-requisites Registration with the UK General Pharmaceutical Council Specify in terms of module codes or equivalent Co-requisite modules Specify in terms of module codes or equivalent Module delivery Mode of delivery Taught Other Pattern of delivery Weekly X Distance Placement Block Other Online X When module is delivered X Semester 1 Semester 2 Throughout year Other Brief description of module This module is an 18 month long, work-based learning module forming content and/ or aims stage 1 of the Foundation Pharmacists Programme. Students will gather Overview (max 80 words) portfolio evidence against global and specific clinical pharmacy outcomes, demonstrating ability to consistently deliver safe and effective pharmaceutical care and optimise medicines use in complex patients. Students will also learn about basic operational aspects of hospital pharmacy and demonstrate progress in all aspects of general professional practice. Module team/ author/ Mrs E Sharp, Dr S Glaspole, Ms K Reygate, Mr Railton Scott coordinator(s) School PABS Site/ campus where Moulsecoomb delivered Course(s) for which module is appropriate and status on that course Course PGDip General Pharmacy Practice Status (mandatory/ compulsory/ optional) Mandatory MODULE AIMS, ASSESSMENT AND SUPPORT Aims To demonstrate a systematic understanding of the principles of pharmacy practice; to acquire the relevant expertise to deliver safe and effective pharmaceutical care across the spectrum of general practice; to critically review and monitor the drug treatment of patients in order to provide competent advice on the safe and effective use of medicines in the context of individual patient care. Learning outcomes Content Learning support At the end of this module practitioners will be able to: 1. Critically discuss the organisation and structure of the NHS and the role of the pharmacist working across sectors to deliver improved patient outcomes 2. Identify, prioritise and resolve the medicines management needs of patients, carers and other social and health care professionals 3. Consult effectively with patients, carers and the multi-disciplinary health care team, respecting diversity and confidentiality 4. Describe the principles of clinical governance and effectively relate them to the practice of pharmacy 5. Independently develop their clinical pharmacy knowledge and skills in order to identify, prioritise and resolve complex pharmaceutical problems in a range of common conditions 6. Critically review the overall management and monitoring of patients with a range of common disease states 7. Recognise the evidence-based approach to management of a range of common conditions and apply to individualised patient care 8. Demonstrate a systematic approach to medicines management for patients with a range of common conditions 9. Apply pharmacokinetic and pharmacodynamic principles to the design of appropriate drug regimens 10. Demonstrate a proactive and critical approach to self development and continue to advance their knowledge and understanding through continuing professional development and life long learning The module provides underpinning knowledge relating to the structure and function of the NHS by highlighting the strengths and weaknesses of past structures. The focus will then turn to the recent NHS reforms and how the current structure deals with key issues such as prioritisation and rationing of health. The syllabus will further cover the concepts of medicines management and medication review. The relationship between health care practitioners and patients will be explored to highlight strategies to improve adherence and the safe and appropriate use of medicines. Ethical and professional issues as they relate to the provision of pharmacy practice and the safe and effective use of medicines, in particular practitioner competence CPD, will be examined as will the role of clinical governance within healthcare and the profession. The interpretation, evaluation and application of laboratory data, clinical pharmacology, adverse drug events, parenteral drug therapy, fluid and electrolyte balance and extemporaneous production will be examined. The practitioner will be expected to describe and evaluate the therapeutic options available to manage a range of common clinical conditions. For example, the treatment of common gastrointestinal, cardiovascular, central nervous system, endocrine and respiratory disorders, antibiotic prophylaxis, anticoagulation and the management of pain and nausea and vomiting. Practitioners will be required to document and discuss the clinical contributions they make to patient care with their practice tutor. This will further explore their understanding and management of the range of common clinical conditions included in this syllabus. A unique feature of this module will be the requirement to review an instance of medication risk, in order to identify both active and latent failures inherent within the care setting and to recommend approaches to minimising risk in the future. E-based resources will be vital. Practitioners will have access to formative case studies intended to assist them in applying theoretical knowledge in the context of the care of patients. Practitioners will be expected to draw on current medical literature available in both their local medicines information centres, as well as their post-graduate library. In addition the following reference sources should be drawn on to provide the underpinning knowledge (current editions): UKMI Workbook, MiCAL (a computer based learning resource) Rules and Guidance for pharmaceutical manufacturers and distributors, ‘Orange Guide’ MHRA Beaney, Quality Assurance of Aseptic Preparation Services, London Pharm Press Allwood M, Stanley A, Wright P, The Cytotoxic Handbook, Ratcliffe Medical Press Clinical Medicine, Kumar P and Clark M. Elsevier & Saunders Davidson’s Principles and Practice of Medicine, Haslett, Chilvers, Boon, Colledge and Hunter, Churchill Livingstone Applied therapeutics: the clinical use of drugs. Young, Koda-Kimble, Kradjan & Guglielmo, App Ther Inc Clinical Pharmacy and Therapeutics, Walker R & Edwards C, Churchill Livingstone Relevant guidelines including National Institute for Health and Clinical Excellence (NICE) guidelines. Teaching and learning activities Details of teaching and learning activities Guided, self directed and self-managed learning is actively encouraged, supported by a range of resources including the library facilities at their practice base; the use of a jointly run MLE with the Medway School of Pharmacy and the world wide web. Practitioners will be expected to develop critical evaluation skills and undertake experiential learning under the guidance of educational facilitators in defined practical rotations. A series of regular learning sets will underpin the module and allow contact between practitioners and academics, in addition to practice tutors. Although formal teaching will be minimal, it will include tutorials given by expert pharmacists or clinicians. In the learning sets, practitioners will discuss, with an academic facilitator, evidence from their portfolio. In addition, practitioners will be supported through regular timetabled meetings to discuss their personal development with their practice and, if necessary, academic tutor. The portfolio of evidence, the opportunity to work with pharmacists from different practice backgrounds, as well as colleagues from within the multi-disciplinary team, will provide practitioners with full opportunities for engagement with the CPD process. Allocation of study hours (indicative) Study hours Where 10 credits = 100 learning hours SCHEDULED This is an indication of the number of hours students can expect to spend in scheduled teaching activities including lectures, seminars, tutorials, project supervision, demonstrations, practical classes and workshops, supervised time in workshops/ studios, fieldwork, external visits, and work-based learning. 65 HEI contact GUIDED INDEPENDENT STUDY All students are expected to undertake guided independent study which includes wider reading/ practice, follow-up work, the completion of assessment tasks, and revisions. 200 PLACEMENT The placement is a specific type of learning away from the University that is not work-based learning or a year abroad. 335 workbased TOTAL STUDY HOURS 600 Assessment tasks Details of assessment for this module All assessments take place at 18 months as listed below: 1) Critical Review of a transfer of care medicines management issue (Los 6, 7, 8 9)(Pass mark 50% but mark does not contribute to overall module mark) 2) 3) 4) Objective Structured Clinical Examination (50%) (LOs 2-3,5-9) Competency based portfolio review which includes evidence of practitioner development across a breadth of practice (Pass/Fail) (LOs 1,2,4,6,7,9,10) Multiple Choice Questions (50%) (LOs 6,8,9) In addition, at 12 months, the student is required to produce from the above list of assessments the following: 1. An interim competency based portfolio review which includes evidence of practitioner development across a breadth of practice 2. A draft of the Critical Review of a medicines management problem. Failure to comply with this requirement may result in the student not being allowed to undertake the final assessments. Types of assessment task1 % weighting Indicative list of summative assessment tasks which lead to the award of credit or which are required for progression. (or indicate if component is pass/fail) WRITTEN Written exam 50% COURSEWORK Written assignment/ essay, report, dissertation, portfolio, project output, set exercise Pass/fail PRACTICAL Oral assessment and presentation, practical skills assessment, set exercise 50% EXAMINATION INFORMATION Area examination board Joint AEB/CEB PG Professional External examiners Name Position and institution Date appointed Date tenure ends Dr C Morecroft Principal Lecturer, Liverpool John Moore’s University 01/01/13 31/12/16 QUALITY ASSURANCE Date of first approval 2011 Only complete where this is not the first version Date of last revision Only complete where this is not the first version Date of approval for this version 2013 Version number 2 Modules replaced n/a Specify codes of modules for which this is a replacement Available as free-standing module? Yes X No 1 Set exercises, which assess the application of knowledge or analytical, problem-solving or evaluative skills, are included under the type of assessment most appropriate to the particular task.