Module Description Template
advertisement
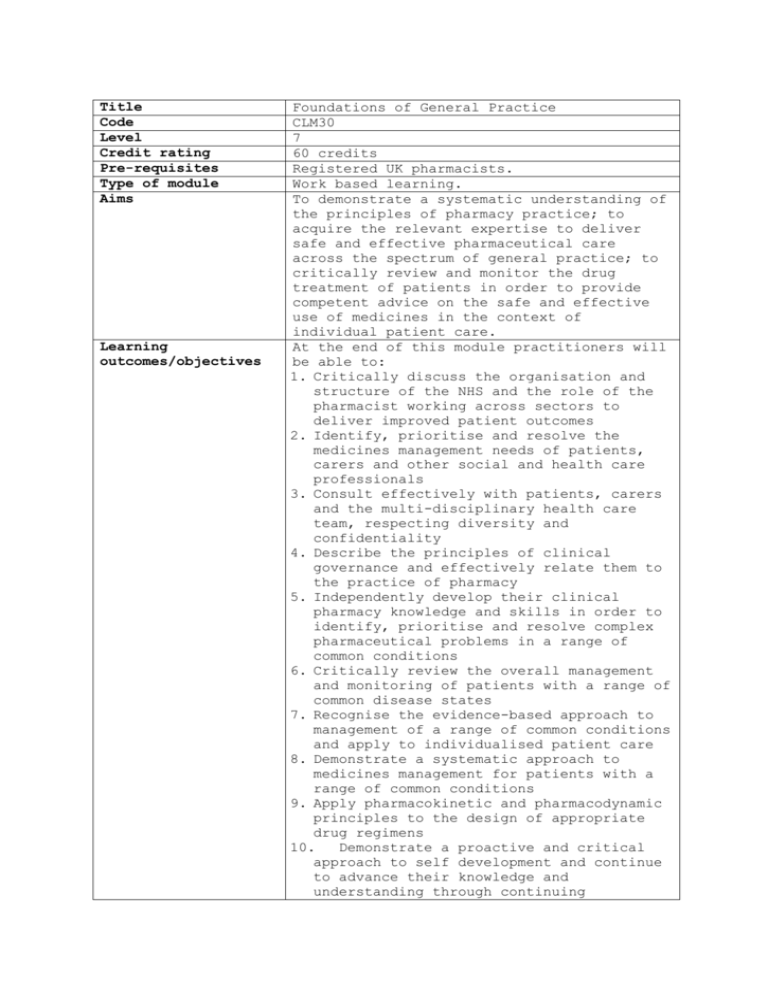
Title Code Level Credit rating Pre-requisites Type of module Aims Learning outcomes/objectives Foundations of General Practice CLM30 7 60 credits Registered UK pharmacists. Work based learning. To demonstrate a systematic understanding of the principles of pharmacy practice; to acquire the relevant expertise to deliver safe and effective pharmaceutical care across the spectrum of general practice; to critically review and monitor the drug treatment of patients in order to provide competent advice on the safe and effective use of medicines in the context of individual patient care. At the end of this module practitioners will be able to: 1. Critically discuss the organisation and structure of the NHS and the role of the pharmacist working across sectors to deliver improved patient outcomes 2. Identify, prioritise and resolve the medicines management needs of patients, carers and other social and health care professionals 3. Consult effectively with patients, carers and the multi-disciplinary health care team, respecting diversity and confidentiality 4. Describe the principles of clinical governance and effectively relate them to the practice of pharmacy 5. Independently develop their clinical pharmacy knowledge and skills in order to identify, prioritise and resolve complex pharmaceutical problems in a range of common conditions 6. Critically review the overall management and monitoring of patients with a range of common disease states 7. Recognise the evidence-based approach to management of a range of common conditions and apply to individualised patient care 8. Demonstrate a systematic approach to medicines management for patients with a range of common conditions 9. Apply pharmacokinetic and pharmacodynamic principles to the design of appropriate drug regimens 10. Demonstrate a proactive and critical approach to self development and continue to advance their knowledge and understanding through continuing Content Teaching and learning strategies professional development and life long learning The module provides underpinning knowledge relating to the structure and function of the NHS by highlighting the strengths and weaknesses of past structures. The focus will then turn to the recent NHS reforms and how the current structure deals with key issues such as prioritisation and rationing of health. The syllabus will further cover the concepts of medicines management and medication review. The relationship between health care practitioners and patients will be explored to highlight strategies to improve adherence and the safe and appropriate use of medicines. Ethical and professional issues as they relate to the provision of pharmacy practice and the safe and effective use of medicines, in particular practitioner competence CPD, will be examined as will the role of clinical governance within healthcare and the profession. The interpretation, evaluation and application of laboratory data, clinical pharmacology, adverse drug events, parenteral drug therapy, fluid and electrolyte balance and extemporaneous production will be examined. The practitioner will be expected to describe and evaluate the therapeutic options available to manage a range of common clinical conditions. For example, the treatment of common gastrointestinal, cardiovascular, central nervous system, endocrine and respiratory disorders, antibiotic prophylaxis, anticoagulation and the management of pain and nausea and vomiting. Practitioners will be required to document and discuss the clinical contributions they make to patient care with their practice tutor. This will further explore their understanding and management of the range of common clinical conditions included in this syllabus. A unique feature of this module will be the requirement to review an instance of medication risk, in order to identify both active and latent failures inherent within the care setting and to recommend approaches to minimising risk in the future. This module is managed and assessed in collaboration with the Joint Programme Board. Guided, self directed and self-managed learning is actively encouraged, supported by a range of resources including the library facilities at their practice base; the London School of Pharmacy based MLE and the world wide web. Practitioners will be expected to develop critical evaluation skills and undertake experiential learning under the guidance of educational facilitators in defined practical rotations. A series of regular learning sets will underpin the module and allow contact between practitioners and academics, in addition to practice tutors. Although formal teaching will be minimal, it will include tutorials given by expert pharmacists or clinicians. In the learning sets, practitioners will discuss, with an academic facilitator, evidence from their portfolio. In addition, practitioners will be supported through regular timetabled meetings to discuss their personal development with their practice and, if necessary, academic tutor. Learning support The portfolio of evidence, the opportunity to work with pharmacists from different practice backgrounds, as well as colleagues from within the multi-disciplinary team, will provide practitioners with full opportunities for engagement with the CPD process. E-based resources will be vital. Practitioners will have access to formative case studies intended to assist them in applying theoretical knowledge in the context of the care of patients. Practitioners will be expected to draw on current medical literature available in both their local medicines information centres, as well as their post-graduate library. In addition the following reference sources should be drawn on to provide the underpinning knowledge (current editions): UKMI Workbook, MiCAL (a computer based learning resource) Rules and Guidance for pharmaceutical manufacturers and distributors, ‘Orange Guide’ MHRA Beaney, Quality Assurance of Aseptic Preparation Services, London Pharm Press Allwood M, Stanley A, Wright P, The Cytotoxic Handbook, Ratcliffe Medical Press Clinical Medicine, Kumar P and Clark M. Elsevier & Saunders Assessment tasks Davidson’s Principles and Practice of Medicine, Haslett, Chilvers, Boon, Colledge and Hunter, Churchill Livingstone Applied therapeutics: the clinical use of drugs. Young, Koda-Kimble, Kradjan & Guglielmo, App Ther Inc Clinical Pharmacy and Therapeutics, Walker R & Edwards C, Churchill Livingstone Relevant guidelines including National Institute for Health and Clinical Excellence (NICE) guidelines. There are two sets of assessments: foundation and clinical. Foundation assessments may be undertaken 12 or 18 months after starting the module. Clinical assessments are normally undertaken 18 months after starting the module. The range of foundation assessments is designed to test the knowledge, skills and attitudes of practitioners. The assessments to be used are (with equal weighting): 1) Foundation Objective Structured Clinical Examination (at 12 or 18 months) (50%) (LOs 2-3,5-9) 2) Competency based portfolio review which includes evidence of practitioner development across a breadth of practice (12 & 18 months) Pass/Fail (LOs 1,2,4,6,7,9,10) 3) Foundation Multiple Choice Questions (at 12 or 18 months) (50%) (LOs 6,8,9) The OSCE will be a criterion referenced with practitioners required to pass 5/8 of the available work-stations in order to pass the module. The range of clinical assessments is designed to test the clinical knowledge, skills and attitudes of the practitioners. The assessments to be used are (with equal weighting): 1) Clinical Objective Structured Clinical Examination (18 months) 50% (LOs 2-3,5-9) 2) Clinical Multiple choice questions 50% (LOs 6,8,9) 3) Competency based portfolio review which includes demonstrating application of medicines management to patients with a defined range of conditions Pass/Fail (LOs 1,2,4,6,7,9,10) Brief description of module content and/or aims (maximum 80 words) Area examination board to which module relates Module team/authors/coordin ator Semester offered, where appropriate Site where delivered Date of first approval Date of last revision Date of approval of this version Version number Replacement for previous module Field for which module is acceptable and status in that field Course(s) for which module is acceptable and status in that course School home The OSCE will be a criterion referenced with practitioners required to pass 5/8 of the available work-stations in order to pass the module. This module focuses on the principles of pharmaceutical care and the core knowledge and skills required of a general level clinical pharmacy practitioner. It requires the practitioner to apply these to a range of patients that reflect the scope of general pharmacy practice. In order to achieve this, practitioners will be required to apply a range of clinical and scientific knowledge to solve common, medication related, problems. It also allows the practitioner to explore and evaluate drug therapy in a number of common disease states and associated surgical conditions. This will require an understanding of the current treatment options, including the current evidence base, available to manage these conditions. A particular emphasis will be placed on minimising the risk associated with medication use. Another feature of this module is the proactive engagement required of practitioners with the process of continuing professional development. AEB/CEB PGDip GPP Mr R Scott, Ms A Conway Not applicable Not applicable February 2010 February 2010 1 CL31 and CLM32 Postgraduate Diploma in General Pharmacy Practice Postgraduate Diploma in General Pharmacy Practice; compulsory module Pharmacy and Biomolecular Sciences External examiner Mrs K Hodson