12.4.09 Vaginal estrogen for chronic UTI
advertisement
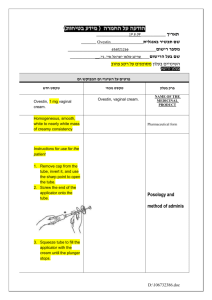
A Controlled Trial of Intravaginal Estriol in Postmenopausal Women with Recurrent Urinary Tract Infections A Randomized Control Trial N Engl J Med, 1993 Sept 9 EBM 12.4.2009 Lindsay Wilson Why this study is important: 1. UTIs cost money and time. In 1996 "direct health costs of an episode of acute cystitis range(d) from $40 to $80" (Ronald). On average, a patient with a UTI loses 24 hours of productivity (Ronald 1996). In 2005, researchers estimated that UTIs cost the global healthcare system at least 6 billion dollars (Kucheria et al.) 2. Additionally, with increasing antibiotic resistance, limiting infections requiring antibiotic treatment is undoubtedly important. 3. Treatment with antibiotics can have unwanted side effects (c diff, candidiasis, GI discomfort). Background: 10-15% of women over 60 have frequent UTIs, perhaps because they have a higher vaginal pH that allows the growth of uropathogens such as E. coli. Estrogen levels in premenopausal women maintain colonization of lactobacilli, which metabolize glycogen to lactic acid. As a result, premenopausal women have low vaginal pH and fewer UTIs. Prior studies have shown an association between use of topical estrogen cream and fewer UTIs in postmenopausal women. STUDY DESIGN: This study was a randomized control trial with the hypothesis that women treated with topical estrogen cream would have fewer urinary tract infections than those treated with placebo cream. Patients were randomly assigned to one of two regimens. One group of 50 women received 0.5 mg of estriol in vaginal cream to be used each night for two weeks followed by twice-weekly applications for eight months, and the other group of 43 received a placebo cream to be used in the same manner. Estriol is a weak estrogen that is not available in the United States. 0.5 mg estriol appears to be equivalent to 1/4 of 25 mcg Estradiol (the amount in Vagifem tablets). Patients and researchers were blinded. Women were asked to record use of cream, side effects, symptoms of UTI, and use of antibiotics in a diary. Urine specimens were taken once monthly and whenever symptoms occured. Women with symptomatic UTIs were treated with a 3 day regimen of either Bactrim or Cipro. Paper does not comment on whether or not urine was tested for cure after antibiotics were given. Possible that recurrent infections were infections that did not resolve with initial treatment. POPULATION: 93 postmenopausal women referred to the Infectious Disease Clinic at Central Emek Hospital, Afula, Israel, with a history of 3 or more microbiologically confirmed symptomatic episodes of UTIs during the previous year with a negative urine culture. **Exclusion criteria: Patients with thromboembolic disorders, severe liver disease, estrogen-dependent tumors, anatomical lesions in UG area, an indwelling urinary cather, or a history of long-term use of antimicrobial agents. **Comparison of the study groups: Similar mean ages (64.7 in estrioltreated group and 65.4 in the placebo-treated group). Similar number of UTIs in the past year (5.2 vs 5.4, respectively). OUTCOMES: **PRIMARY: Urinary tract infection (defined as presence of typical clinical symptoms--dysuria, frequency, urgency, and incontinence-- and laboratory evidence of pyuria (at least 8 leuks per cubic millimeter of unspun urine) and a midstream urine culture yielding 10^5 CFU per mm). **SECONDARY OUTCOMES: Vaginal pH, vaginal cultures, days of antibiotic use. Calculations: Limited based on the presentation of data in the paper. Hazard rate= # events/time Estrogen treated patients 10/310=0.458 Placebo treated patients 103/225= .032 Hazard ratio = 0.458/.032= 14 (Those not treated with topical estrogen cream were 14 times more likely to have a urinary tract infection) RESULTS: These other results are suspect given the paper does not indicate how they factored in the subjects who withdrew. Rates of infection: Mean incidence: 0.5 (estrogen-treated) vs 5.7 (placebo-treated) per patient year Estrogen-treated patients used significantly fewer abx. # of days on abx 6.9 (est) vs 32 (placebo), had lower vaginal pH, and were more likely to have cultures with lactobacilli. UTIs developed in 3 of the 23 estriol women who were colonized with lactobacillus as compared with 7 of the 13 who were not colonized with lactobacillus. Adverse reactions: vaginal irritation, burning, itching who were observed in 10 of the estriol-treated women and 4 of the placebo recipients. These rxns were mild but caused all of these women to actually withdraw from the study. Early withdrawal also occurred with 10 women in the placebo group due to need for systemic antimicrobial prophylaxis for recurrent infections. One woman in the estriol-treated group was withdrawn from the study because she died. CONCLUSION: "The intravaginal administration of estriol prevents recurrent urinary tract infections in postmenopausal women, probably by modifying the vaginal flora." ARE THESE RESULTS VALID? 1. Was assignment randomized? YES 2. Was follow-up complete? ??? Paper does not provide clear information regarding the duration of follow up for all subjects or how they were analyzed if they did not complete the entire 8 month duration of the study. 3. Were patients analyzed in the groups to which they were randomized? YES 4. Was the study blinded? YES 5. Were the groups similar at the start of the trial? YES 6. Were the groups treated equally? YES DISCUSSION: UTIs are an important health problem for a large and growing population of postmenopausal women. Due to increasing antibiotic resistance and the undesirable side effects of antibiotics finding an alternative approach to this problem is important. This study confirms the efficacy of estrogen in reducing the number of urinary tract infections in pm women who have a history of recurrent infections. In my opinion, these results are applicable to my ACC clinic patients who are postmenopausal with recurrent UTIs. Given estriol is not available, I would have to prescribe Estradiol instead. Vagifem is a dissolving tablet form of local Estradiol that is likely easier to use. It has been shown to reduce vaginal atrophy at the dose of 25 mcg. Vagifem 10 mcg will be available in 2010 (MPR 2009). I would prescribe that amount for my postmenopausal women with recurrent UTIs, being careful to not prescribe it to women with a history of clots, breast cancer, or uterine cancer. Works Cited: Kucheria, R, Dasgupta, P, Sacks, S H, Khan, M S, Sheerin, N S (2005). Urinary tract infections: new insights into a common problem. Postgrad. Med. J. 81: 83-86 Ronald, A. (1996). Sex and Urinary Tract Infections. NEJM 335: 510-512 Vagifem 10mcg approved for atrophic vaginitis due to menopause. Monthly Prescribing Reference. December 3 2009. http://www.empr.com/vagifem-10mcg-approved-for-atrophic-vaginitis-due-to-menopause/article/158994/