File - Whether through formal schooling or through the
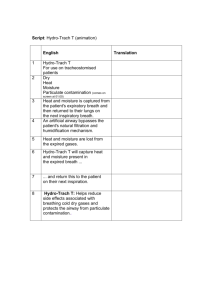
advertisement

Running Head: QUALITY IMPROVEMENT PROCESS 1 QUALITY IMPROVEMENT PROCESS Kimberly K. Proux Ferris State University QUALITY IMPROVEMENT PROCESS 2 Abstract This paper reflects a leadership strategy analysis indicating a quality improvement process. The quality improvement process concentrates on patient advocacy and patient safety regarding pediatric tracheostomy suctioning. Pediatric tracheostomy patients are even more vulnerable than their adult counterparts because of their inability to communicate effectively. Nurses, family, and other care givers must be trained to be aware of the patient’s needs as well as the actual evidence-based techniques used to suction pediatric tracheostomy patients. The quality improvement process integrates action theory and education to address the needs of pediatric tracheostomy patients. Keywords: quality improvement process, patient advocacy, patient safety, pediatric tracheostomy suctioning, evidence-based practice, action theory, education QUALITY IMPROVEMENT PROCESS 3 Quality Improvement Process In the healthcare field when quality improvement is addressed it can be delivered in a couple of different ways; there is more than one focus regarding quality improvement. There are quality improvement indicators for patients. Evidence-based management is used in achieving patient safety; “the National Database of Nursing Quality Indicators (NDNQI) are good resources for the nurse manager. The NDNQI measures are specifically concerned with patient safety and aspects of quality of care that may be affected by changes in the delivery of care” (Yoder-Wise, 2011, p.63). There are quality improvement indicators of staffing effectiveness such as average daily census (ADC), percentage of occupancy, and average length of stay (ALOS), these are measures used to help the nurse manager calculate the number of patients coming and going on a particular unit so that the nurse can “match the needs of the patients with the appropriate number of staff members” (Yoder-Wise, 2011, p.288). The last quality indicator this paper will focus on is what Yoder-Wise (2011) refers to as “the basic building block of quality, patient safety” (p. 26), which healthcare workers provide by advocating for their patients. The examples of quality improvement provided are not only used in facilities, but by nurses who work in patient homes. In the home nurses provide quality improvement by being concerned with patient safety, there is usually only one nurse in the home at a time, but that nurse has a team to work with to help ensure the patient needs are met, and patient advocacy is a home care nurse’s way of giving the patient a voice. Home care nurses also provide education to patients as well as families so that they can be assured that the patient will be properly cared for when they are not in the home. This paper will address leadership strategies by focusing on advocacy and education to safeguard patient safety. QUALITY IMPROVEMENT PROCESS 4 Identified Clinical Need The particular home care service I am employed with has approximately 114 clients, of the 114 clients 4 are clients who have tracheostomies; of the 4 clients who have tracheostomies 3 are children. Some of these children have diseases that will improve to the point where they will no longer need the assistance of a tracheostomy; others will be tracheostomy dependent their entire lives. We have one family with a child who has a tracheostomy and experiences many negative health issues due to the fact that she is not being suctioned enough when the nurses are not in the home. A tracheostomy tube that is obstructed even moderately causes severe breathing difficulties. The significance of tracheostomy management is to ensure patency of the airway. Neglecting to suction a child in need exposes the child to risks such as hypoxia, respiratory compromise and pneumonia. (Lippincott Williams & Wilkins, 2013) Interdisciplinary Team Quality improvement is an attitude and culture that should resonate through the entire interdisciplinary team. As such, “the foundation for a successful quality improvement program is strong motivation, teamwork, and leadership. Potential motivators for quality improvement programs are numerous” (Curtis et al., 2006). In this case a patient-specific safety issue is the stimulus. The interdisciplinary team will be selected based on their contact with the child, their involvement in the case, and their propensity to educate; this will allow for a multidisciplinary team with a common goal of achieving the best possible outcome for this child. The interdisciplinary team for this case and all other tracheostomy cases will consist of: service coordinators who open the tracheostomy cases, the nurses who will be working the cases, the durable medical equipment (DME) employees who supply equipment to tracheostomy cases, the respiratory educators from the main hospital and the patient’s mother. QUALITY IMPROVEMENT PROCESS 5 Data Collection Method According to Yoder-Wise (2011), “After the multidisciplinary team forms, the group collects data to measure the current status of the activity, service, or procedure under review. Various data tools may be used to analyze and present this information (p. 396). The tool most helpful in this case is a flow chart diagramming the existing educational process of pediatric tracheostomy suctioning. (See Appendix A) Quality Improvement Goals There are two very specific goals for improvement, 1.) Children who have a tracheostomy and are cared for by Home Services nurses will maintain a patent airway as evidenced by, a.) No mucus plug(s) witnessed in the tube and/or trachea. b.) Child will experience no respiratory compromise from pooling secretions. c.) Mechanical ventilator will show no increase in peak airway pressures during volume controlled mechanical ventilation. d.) Mechanical ventilator will show no decreased tidal volume during pressure controlled ventilation. 2.) Mom will learn and demonstrate pediatric tracheostomy suctioning and maintain a patent airway when nurses are not in the home as evidenced by, a.) Attendance of quality improvement processes and completing demonstrations of learned equipment and suctioning techniques. b.) An improved patient picture observed by Home Services nurse upon entering the home for shift work. c.) No mucus plug(s) witnessed in the tube and/or trachea. QUALITY IMPROVEMENT PROCESS 6 d.) Child will experience no respiratory compromise from pooling secretions. e.) Mechanical ventilator will show no increase in peak airway pressures during volume controlled mechanical ventilation. f.) Mechanical ventilator will show no decreased tidal volume during pressure controlled ventilation. Evidence-based practice promotes airway patency regarding pediatric tracheostomy suctioning. “Airway patency is maintained in a child with a tracheostomy tube by periodically suctioning excessive secretions and mucus plugs from the tube and the trachea” (Lippincott, Williams & Wilkins, 2013). Proper suctioning technique ensures that the child doesn’t experience respiratory compromise. Implementation Strategies Appendix B provided in this paper outlines a process for implementing a plan for change. The plan integrates all members of the interdisciplinary team and focuses on education as well as demonstration not only by the trainers, but also by the trainee’s. I perceive this plan as based upon an action theory, These theories may include motivational elements, but postulate that other factors are necessary to predict behavior. Examples include operant conditioning and implementation intentions. Operant conditioning proposes that behaviors that have positive consequences for the individual (such as remuneration) are likely to be repeated. For example, women are told to specify where and when they will perform breast self-examination, and subsequently are found to have followed through more frequently than those with no plan regarding their intention to implement. While studies thus far have utilized this theory for QUALITY IMPROVEMENT PROCESS 7 patient behavior change, it may be just as applicable to provider behavior change (e.g., a provider education QI strategy might incorporate a step that asks the clinician to formulate a plan for implementing a change in practice). (McDonald, K., Graham, I., Grimshaw, J., 2004) If both the nurses and mom are taught using the specific equipment that is used in the home and are learning what evidence-based practice teaches using proper suctioning technique guidelines provided by Lippincott Williams & Wilkins the only other barrier that needs to be addressed is the action theory’s application of repetition, which will start with the initiation of demonstrating back in the training sessions and continue in the home as evidenced by the child’s patent airway. Evaluation After attending the training for pediatric tracheostomy suctioning education a “check and balance” system will be put into place. Documentation will be a strong component. A log will be kept in the home specifically addressing the issue of tracheostomy suctioning; it will include the indicators of why the patient needed suctioning (patient picture), what time the suctioning was done, and what the results of the suctioning were (again, patient picture). Client/family in this case mom, will also be asked to document her actions on this log; she will then have documented evidence of the outcomes of her efforts. Theoretically, she should see an improvement in her daughter’s morning routine of needing an extreme amount of suctioning, percussion and breathing treatments because she suctioned her throughout the night as needed. Home services will follow up on the education with formal testing and informal testing, QUALITY IMPROVEMENT PROCESS 8 The formal examinations will focus on measuring the knowledge and practices learned, they will be performed as written or verbal tests. All who attend the education will demonstrate competency in pediatric tracheotomy suctioning. Informal testing will include questions focused on specific aspects of pediatric tracheotomy suctioning. Informal testing allows trainers to interact directly with nurses and client/family and discuss general aspects of patient care. It also allows nurses and client/family to ask questions and learn more about challenging areas of training that they may be having difficulties with. Peer assessment will allow nurses and client/family to evaluate each other and to learn from one another. Peer assessments encourage communication and interaction among one another, nurses and client/family will have increased opportunities to share knowledge and information about patient care. On-the-job training assessment will include evaluation of clinical competency, patient interactions and the clinician's adherence to generally accepted clinical practice guidelines. (Day, R., 2013) The 4 different types of testing and assessments (formal and informal testing, peer evaluation and on-the-job assessment) will be done throughout the year following the initial education process. At the end of the year records shall show the nurses and client/family have had documentation of each type of testing completed. If records show that the testing disclosed unsatisfactory results, the tests will be retaken after completing more training. QUALITY IMPROVEMENT PROCESS 9 Conclusion At this point mom should have developed a routine suctioning her daughter throughout the night and her efforts will be rewarded when she realizes the benefits to her child as the action theory advocates. Evidence-based practice has been accomplished by teaching and learning skillful pediatric suctioning techniques and following up on skill retention. The quality improvement process developed in this paper addresses patient advocacy by helping the mother of the child to understand the importance of developing a routine of night-time suctioning as needed. Patient safety is addressed by providing education to all involved in the patient’s care. QUALITY IMPROVEMENT PROCESS 10 Appendix A Home Services manager hires nursing staff Written skills test is given prior to hire Steps diagramming the existing educational process of pediatric tracheostomy suctioning Practical skills test is given prior to hire Orientation day touches upon the fact that we care for pediatric tracheostomy patients New nurse shadows with current nurse in the home of a pediatric patient Client/Family never receives formal training and/or refresher training from Home Services QUALITY IMPROVEMENT PROCESS 11 Appendix B Service Coordinator Determines Date, time, and place for training purposes Steps diagramming the educational process of pediatric tracheostomy suctioning Informs interdisciplinary team and confirms availability Meets with DME & Respiratory Educators to plan educational outline Review of knowledge gained from education process DME educates specifically regarding equipment Respiratory Educator trains suctioning technique Have nursing staff demonstrate learned equipment and suctioning technique Have mom demonstrate learned equipment and suctioning technique QUALITY IMPROVEMENT PROCESS 12 References Boroughs, D. S., & McNichol Dougherty, J., (2013), Evidence-Based Pediatric Secretion Management, Retrieved from: http://ce.nurse.com/ce619/evidence-based-pediatricsecretion-management/coursepage/ Curtis, J. R., Cook, D. J., Wall, R. J., Angus, D. C., Bion, J., Kacmarek, R.,… Kane-Gill, S. L. (2006). Intensive care unit quality improvement: A "how-to" guide for the interdisciplinary team. Critical Care Medicine, (34)1, 211-218. doi: 10.1097/01.CCM.0000190617.76104.AC Day, R., (2013), Methods of Evaluating Training in Primary Health Care, Retrieved from: http://www.ehow.com/list_6939007_methods-training-primary-health-care.html Lippincott Williams & Wilkins, (2013), Tracheostomy Suctioning, Pediatric, Retrieved from: Munson Healthcare Intranet McDonald, K., Graham, I., Grimshaw, J., (2004), Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies, Volume 1—Series Overview and Methodology. Technical Review 9 (Contract No. 290-02-0017 to the Stanford University–UCSF Evidence-based Practices Center). AHRQ Publication No. 04-0051-1. Rockville, MD: Agency for Healthcare Research and Quality. Retrieved from: http://www.ncbi.nlm.nih.gov/books/NBK43908/pdf/TOC.pdf Yoder-Wise, P. S. (2011). Leading and managing in nursing (5th ed.). St. Louis, MO: Elsevier Mosby.