Gilbert: Mg2+, Ca2+, PO4- Handling & Na2+ Volume Regulation
advertisement

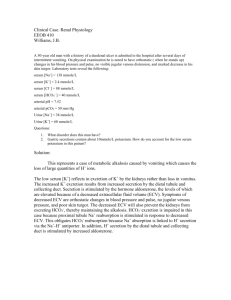
Gilbert: Mg2+, Ca2+, PO4- Handling & Na2+ Volume Regulation Ruth Olson Desmopressin may occasionally be administered to patients with substantial polyuria caused by central diabetes insipidus. A risk associated with the use of ADH in this context is that acute hyponatremia and volume expansion can occur in a patient receiving IV fluids with consequent brain swelling and dath. In this setting what terminates the physiologic effects of ADH? 1. Increase in plasma volume 2. 2. Decrease in plasma osmolarity 3. Inc levels of cAMP in collecting duct cells 4. Endocytosis of aquaporin water channels 5. Receptor-mediated endocytosis of ADH from the luminal surface The thick ascending limb in the loop of Henle is: 1. Permeable to water 2. Permeable to NH3 3. Permeable to H+ 4. Impermeable to water 2. Permeable to NH3 3. Permeable to H+ A dec. in the conc. Of NaCl in the intraluminal fluid causes the juxtaglomerular apparatus to release: 1. ADH 2. Aldosterone 3. Adenosine 4. Renin 5. Angiotensinogen Factors that alter renal Ca2+ excretion Mg2+ ↓Calcium Excretion ↑Parathyroid hormone (PTH) ↓ ECF Volume ↑Calcium Excretion ↓PTH ↑BP ↑ Plasma PO4Metabolic acidosis Vitamin D3 ↑BP ↓Plasma PO4Metabolic Alkalosis • As far as we know, there is NO hormone that has direct control of Mg excetion and absorption. HE WON’T ASK US QUESTIONS ON MG2+ EXCEPT IN TERMS OF ION TRANSPORT FROM ANOTHER LECTURE • >1/2 of body Mg++ is stored in bone • Mechanisms of Mg++ excretion are poorly defined • These disturbances lead to increased Mg++ ↑ ECF Volume excretion • Increased ECF Mg++ • ECF volume expansion • Increased ECF Ca++ concentration This schematic shows an illustration of Ca2+ balance in the body. Under normal conditions, its interactions with the bone and liberation of Ca2+ from bone (resorbption) or formation. Magnesium balance. IN calcium, PTH has well defined actions on bone and kidney… magnesium is not that way. Factors affecting Phosphate excretion The primary hormone regulator is PTH • Dietary intake • Calcium levels • Acute hypercalcemia decreases phospate excretion • Chronic hypercalcemia inhibits excretion • Chronic hypercalcemia increases reabsorption Gilbert: Mg2+, Ca2+, PO4- Handling & Na2+ Volume Regulation Ruth Olson Potassium \ K+ input= output; you can increase intake a lot without really affecting [plasma K+] 98% is intracellular (opp. Of Na+) Severe hyperkalemia o Partial depolarization of cell membranes o Cardiac toxicity ventricular fibrillation or asystole Severe hypokalemia Hyperpolarization of cell membranes Fatigue, muscle weakness hypoventilation delayed ventricular repolarization Control of Principal cell K+ Secretion Remember these factors! On the left favor K+ movement into the cell. On the right, they do the opposite movement out of the cell. Secretion occurs in the cortical collecting tubule: K+ secretion by principal cells: active pumping followed by passive diffusion in to the tubule Inc. Extracellular K+ concentration : increases K+ secretion Aldosterone : increases K+ secretion o Without aldo system the more K+ you intake, the higher the K+ concentration of plasma. Sodium (volume) delivery : increases K+ secretion o Increase in Na volume (not the same as increases in [Na]) increased delivery to macula densa cellsincreases K secretion Acid - base status: - acidosis : decreases K+ secretion - alkalosis : increases K+ secretion Gilbert: Mg2+, Ca2+, PO4- Handling & Na2+ Volume Regulation Ruth Olson Questions: 1. Fill in ↑ OR ↓ in table ↓Calcium Excretion __Parathyroid hormone (PTH) __ECF Volume Increase the flow rate (water) and you “wash out of K+” Remember that K will stay the same if Na intake is increased. H+ ions inhibit the ATPase mechanism inhibits K secretion! Alkalosis ↑K+ in cells↑K+ Secretion ↑K+Excretion K+ Depletion **For K+, dietary intake is very important. If you increase you intake, you’ll excrete the excess, but if your on a chronically low K+ diet, that can cause hypokalemia. ↑Calcium Excretion __PTH __ECF Volume __BP __BP __Plasma PO4- __Plasma PO42. What hormone is the primary regulatory hormone for Ca2+? 3. T/F You can increase intake a lot without really affecting [plasma K+] 4. K+ secretion by intercalated cells in the cortical collecting tubule Answers: 1. ↓Calcium Excretion ↑Parathyroid hormone (PTH) ↓ ECF Volume ↑Calcium Excretion ↓PTH ↑BP ↑ Plasma PO4- ↑BP ↓Plasma PO4- ↑ ECF Volume 2. Parathyroid hormone 3. T 4. F. Secretion occurs by principal cells. Gilbert: Mg2+, Ca2+, PO4- Handling & Na2+ Volume Regulation Ruth Olson Na2+ Volume Regulation Sodium balance is maintained but at a higher AP. This summarizes whats become known as RENAL-Body Fluid Arterial Pressure Feedback. Na2+ intake or excretion interacts to produce whatever EC fluid volume you have. CO*TPR=MAP Regulation of arterial pressure long-term relies on proper renal function. On top, it demonstrates that salt doesn’t affect BP that much in healthy kidneys. The dotted line indicates a problem with renal function BP is raised. Normal Water and Sodium Balance Na+ is the primary solute in the ECF Inextricably linked but at the same time separate Na+ regulation can be thought of as two processes o Proximal nephon: coupled changes in Na+ and water excretion o Distal nephron: Na+ can be reabsorbed independently of water Disorders of Na+ Balance are disorders of ECF volume Hyponatremia o Usually associated with hypoosmolality o May occur with normal, excess or deficit of Na+ Hypernatremia o Usually a result of excess water loss Gilbert: Mg2+, Ca2+, PO4- Handling & Na2+ Volume Regulation Ruth Olson Remember that if filtration falls, the reabsorption needs to also decrease (that’s occurring in the positive balance section.) If reasborption dec, excretion would initially increase to bring it back down to steady state. Decrease initially in Na+ excretion until they reach a set point for maintaining sodium balance but at a higher arterial pressure Gerenally this is like when you give diuretics. Diuretic therapy increases Na2+ excretion and decreases ECF volume Negative feedback loops involved Gilbert: Mg2+, Ca2+, PO4- Handling & Na2+ Volume Regulation Ruth Olson Regulation of Fluid Balance in Hypertension: When there is a disturbance of kidney function that tends to cause sodium and water retention, and if local and hormal mechanisms are unable to maintain balance, increase BP (HTN) serves to allow the kidney to “escape” from Na2+ and water retention (a result of a nasty feedback loop.) Decrease initially in Na+ excretion until they reach a set point for maintaining sodium balance but at a higher arterial pressure. People with fewer glomeruli develop HTN, but they don’t seem to be salt sensitive. This can be a gradation, depending on the severity of the disease. Common example. CHF results in a dec. in CO; which in the kidney is a dec in GFR, which results in dec. delivery of NaCl at the macula densa. These pateints have acites. Similar response occurs for hemorrhage. Minimal chenge disease loss of charges at basement membrane excess filtration With accumulating edema, kidney will see that as a dec. in GFR and initiate the feedback mechanisms to retain Na and expand plasma volume. Gilbert: Mg2+, Ca2+, PO4- Handling & Na2+ Volume Regulation Ruth Olson Questions: 1. T/F Na+ is the primary solute in the ECF 2. Increased Na+ reabsorption is caused by all but: a) Small increase in blood pressure b) Decreased peritubular capillary pressure c) Increased angiotensin II d) Increased aldosterone 3. T/F People with fewer glomeruli develop HTN and they seem to be salt sensitive. 4. Which of the following are systemic mechanisms of body fluid regulation a) b) c) d) e) Changes in hormones Changes in sympathetic activity Changes in BP Changes in Blood composition All of the above As Blood Pressure increases, initially, excretion is declining. But as the volume expands, the P increases until it reaches a steady state again. Answers: This gives you the benefit of seeing the time component. 1. T If there is impaired renal function impaired ability to excrete Na na is retained and H2O follows Plasma volume expands inc hydrostatic P and BP. 2. a. Small DECREASE in BP would be correct Here you’re achieving a new set point to excrete Na+ at a higher BP. This is an example of renal ablation. Clinically it would be more progressive. 3. F. People with fewer glomeruli develop HTN, but they DON’T seem to be salt sensitive. 4. e