File - Lisa Sims, CRNP
advertisement
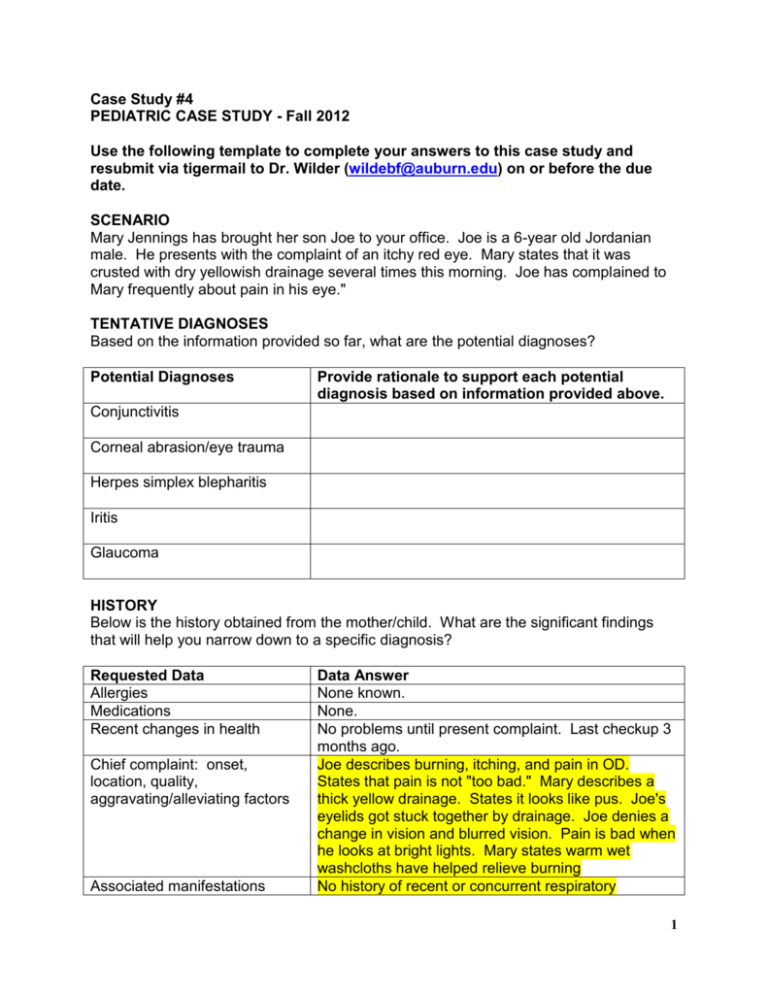
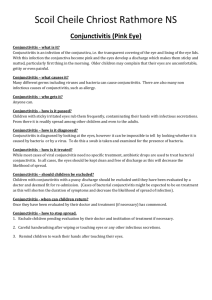
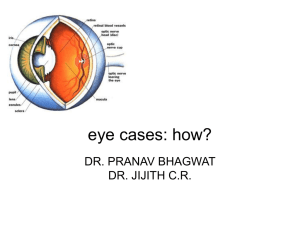
Case Study #4 PEDIATRIC CASE STUDY - Fall 2012 Use the following template to complete your answers to this case study and resubmit via tigermail to Dr. Wilder (wildebf@auburn.edu) on or before the due date. SCENARIO Mary Jennings has brought her son Joe to your office. Joe is a 6-year old Jordanian male. He presents with the complaint of an itchy red eye. Mary states that it was crusted with dry yellowish drainage several times this morning. Joe has complained to Mary frequently about pain in his eye." TENTATIVE DIAGNOSES Based on the information provided so far, what are the potential diagnoses? Potential Diagnoses Provide rationale to support each potential diagnosis based on information provided above. Conjunctivitis Corneal abrasion/eye trauma Herpes simplex blepharitis Iritis Glaucoma HISTORY Below is the history obtained from the mother/child. What are the significant findings that will help you narrow down to a specific diagnosis? Requested Data Allergies Medications Recent changes in health Chief complaint: onset, location, quality, aggravating/alleviating factors Associated manifestations Data Answer None known. None. No problems until present complaint. Last checkup 3 months ago. Joe describes burning, itching, and pain in OD. States that pain is not "too bad." Mary describes a thick yellow drainage. States it looks like pus. Joe's eyelids got stuck together by drainage. Joe denies a change in vision and blurred vision. Pain is bad when he looks at bright lights. Mary states warm wet washcloths have helped relieve burning No history of recent or concurrent respiratory 1 Associated symptoms History of exposure to conjunctivitis History of swimming in chlorinated or contaminated water History of trauma to eye History of exposure to chemical Recent cold sores or exposure to herpes lesions Recent history of impetigo Family members with eye problems Past medical history infection. Denies history of throat pain, ear pain, rhinorrhea. None. Has swam two times in the past week in nonchlorinated pool. None. None. None. None, but his younger brother was started on Keflex 3 days ago for impetigo on his face. Joe has two younger siblings who do not have any eye symptoms. Normally healthy. No hospitalizations or surgeries. PHYSICAL EXAM Significant portions of PE based on the chief complaints SYSTEM Skin FINDINGS Skin is pink and supple, no lesion noted. Heart sound S1 and S2 normal, without murmur Clear to auscultation Breath sounds Vital signs Ear, nose, throat Eyes T (oral) 98. HR 84, RR 22, BP 88/56 TMs pearl gray bilaterally. Nares patent and free of drainage. No pharyngeal erythema or edema. No oral lesions. OS sclera white, without injection, erythema, or edema. OD edema of eyelids present. Crusted yellow drainage on lashes. Conjunctiva markedly RATIONALE Overall quick assessment of visible skin should be performed. Particular attention should be given to the face. Provides baseline information. Allows the NP to determine if there has been respiratory involvement. Gives an indication of possible infection. Gives an indication of possible infection. Needs to evaluate eyes thoroughly to identify possible diagnoses. Visual acuity should be completed for all 2 Eyes (cont.) inflamed. Cornea and eyelid margins without ulceration. PERL with positive red reflex bilaterally. Visual acuity reveals OD 20/20, OS 20/20. Fundoscopic Discs well marginated. No AV nicking Lymphatics No palpable lymph nodes in the head of neck. patients with eye problems. It is vital for patients with decreased vision. This test may be painful if the child has photophobia. Provides a quick indication of eye health. This test may be difficult owing to photophobia and constriction of pupils. Palpation of lymph nodes can provide an indication of infection. DIFFERENTIAL DIAGNOSES Provide the significant positive and negative data that support or refute your diagnoses. DIAGNOSIS Allergic conjunctivitis POSITIVE DATA Visual acuity normal – OD 20/20, OS 20/20 – burning, itching and pain - pain is not “too bad’- denies change in vision and blurred vision-PERL-no palpable lymph nodes in the head of neck NEGATIVE DATA Pain is bad when he looks at bright lights- Bacterial conjunctivitis Itching in OD, Thick yellow drainage- states it looks like pus- eyelids got stuck together by drainage- visual acuity is normal and denies change in vision or blurred vision- crusted yellow drainage on lashes- PERLno palpable lymph nodes in the head of neck- swam two times in the past week in nonchlorinated poolyounger brother was started on Kelfex 3 days ago for impetigo on his face- conjunctiva markedly Pain is bad when he looks at bright lights- denies history of throat pain, ear pain 3 inflamed Chemical conjunctivitis Viral conjunctivitis Visual acuity is normalitching, burning and pain PERL- denies any change in vision and blurred visionconjunctiva markedly inflamed Corneal abrasion/eye trauma Pain in OD- pain is bad when he looks at bright lights- no history of trauma to eye Herpes simplex blepharitis Iritis Glaucoma Itching and burning in ODpain is bad when he looks at bright lights- younger brother was started on Kelfex 3 days ago for impetigo on his face Pain in OD- pain is bad when he looks at bright lights No history of exposure to chemical- swam in nonchlorinated pool Pain is bad when he looks at bright lights- no palpable lymph nodes in the head of neck – no history of recent or concurrent respiratory infection-TMs pearl gray bilaterally, nares patent and free of drainage- no pharyngeal erythema or edma- denies history of throat pain, ear pain or rhinorrhea Itching- thick yellow drainage- Cornea and eyelid margins without ulceration- normal visual acuity – no recent cold sores or exposure to herpes lesions Burning, itching and pain in OD, thick yellow drainagePERL- no blurred vision No palpable lymph nodes in Thick yellow drainagethe head of neck normal visual acuity- PERL- 4 DIAGNOSTIC TESTS Based on the history and PE, the following tests were ordered. The test and results are provided. You will need to provide a rationale to support the use of this test or provide documentation why you would not order this test in this case. DIAGNOSTIC TEST Eye culture and gram stain RESULTS Test not done. RATIONALE This test would not be ordered unless N. gonorrhea is suspected which it is not. The patient has not been treated for any type of conjunctivitis in the past nor has he failed to respond to any prior treatment. The visual acuity test was normal. DIAGNOSES Based on the data provided, what are the appropriate diagnoses for Joe? List all appropriate diagnoses for Joe in priority order. Diagnoses Rationale 1. Patient has thick yellow drainage. 1. Bacterial conjunctivitis Conjunctiva markedly inflamed. OD edema of eyelids present. – Visual acuity is normal. 2. Allergic Conjunctivitis 2. Itching and burning, normal visual acuity THERAPEUTIC PLAN Provide answers with scientific basis for the following questions about Joe's treatment plan. Provide APA references when indicated. (1) What therapeutic agent would you use in planning care for Joe? First Choice- Azithromycin ophthalmic drops- 1 drop two time per day for 2 days then 1 drop daily for 5 days Second choice – Trimethoprim and polymyxin B (Polytrim) – 1-2 drops four times daily for 5-7 days Third Choice – Erythromycin ophthalmic ointment – ½” four times daily for 5-7 days References: 5 Uptodate, 2012. Therapy of conjunctivitis. Bacterial Conjunctivitis. Retrieved from http://www.uptodate.com/contents/conjunctivitis?source=search_result&search=b acterial+conjunctivitis+children&selectedTitle=1%7E21 Gerzevitz, D., Porter, B. O. & Dunphy, L. M. (2011). Eyes, ears, nose, and throat problems. In L. M. Dunphy, J. E. Winland-Brown, B. O. Porter, & D. J. Thomas (Eds), Primary care: The art and science of advanced practice nursing (pp. 245330). Philadelphia, PA: F.A. Davis Company. (2) What is your rationale for choosing this particular agent? The reason this agent was chosen was because it is dosed less frequently. If the child goes to school, it will be difficult to give the child ointment or drops four times a day. Ointment can cause blurry vision for 20 minutes after use and if the child is in school this could be a problem. Azithromycin drops are more expensive so it will be beneficial to know if the child has insurance. If not then the second or third option should be chosen because it is less expensive but will require dosing more frequently. (3) What education does Mary need to provide relief for Joe and decrease the risk of reinfection? Education should be given to include: 1. The secretions may remain infectious for at least 48 hours after the start of treatment 2. Conjunctivitis is highly contagious 3. Use good hand washing 4. Do not touch eyes 5. Do not share towels and washcloths 6. Do not touch the medication applicator to the eye 7. Should stay home from school or day care until there is no longer any secretions but if that is not feasible then at least after receiving 24 hours of treatment Reference: 6 Gerzevitz, D., Porter, B. O. & Dunphy, L. M. (2011). Eyes, ears, nose, and throat problems. In L. M. Dunphy, J. E. Winland-Brown, B. O. Porter, & D. J. Thomas (Eds), Primary care: The art and science of advanced practice nursing (pp. 245330). Philadelphia, PA: F.A. Davis Company. 7