Herpes Zoster Ophthalmicus: Symptoms, Diagnosis, and Management
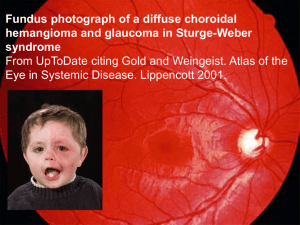
advertisement

Patients with HZO typically present with prodromal pain in a unilateral V1 dermatomal distribution, followed by an erythematous vesicular or pustular rash to the same area. Pain is neuropathic, and patients may describe the sensation as "burning" or "shooting," sometimes accompanied by paresthesias. Additionally, the herpetic rash may be preceded by constitutional symptoms such as fever, fatigue, malaise, and headaches. The presence of herpetic lesions around the tip of the nose is known as the Hutchinson sign. The presence of Hutchinson's sign indicates nasociliary branch involvement of V1, which confers a higher risk for ocular involvement. The nasociliary branch innervates the tip of the nose and cornea, as well as other ocular structures.[8][9][10][11][12][13] The physical exam begins with an external evaluation of lesion distribution, including the eyelids and scalp. The rash often appears maculopapular before transitioning to vesicles and pustules that ultimately rupture and scab over. Although the rash is usually limited to a single unilateral dermatome, immunocompromised patients may develop disseminated disease, with a possible bilateral presentation. Particular attention should be paid to eyelid involvement, which is frequently associated with blepharitis, conjunctivitis, and episcleritis. Ptosis is rare but may occur in response to marked inflammation. A thorough ocular exam is required and must include visual acuity, slit-lamp examination with fluorescein staining, and ocular tonometry. A thorough dilated funduscopic exam is also necessary. • • Corneal involvement includes both epithelial keratitis and stromal keratitis. o Epithelial keratitis may present as punctate and/or pseudodendritic keratitis. Punctate keratitis is characterized by scattered fluorescein-stained swollen lesions on the superficial surface of the cornea. It is thought that these lesions contain the live replicating virus. Pseudodendrites appear as branching lesions similar to the true dendritic lesions seen in herpes simplex virus (HSV) keratitis. Unlike the dendrites of HSV, which appear as brightly staining ulcers with terminal bulbs, HZO pseudodendrites are non-erosive mucous plaques that exhibit minimal staining with an absence of terminal bulbs. o Stromal keratitis may be classified as anterior or deep and usually develops after epithelial keratitis. Anterior stromal keratitis results from an immune-mediated response to the virus and is characterized by nummular (coin-shaped) granules in the superficial stroma. Deep stromal keratitis usually occurs late in the disease course (often months after the acute phase) and presents with marked corneal edema often associated with anterior uveitis. o Severe keratitis may eventually lead to neurotrophic keratopathy due to persistent inflammatory injury to the corneal sensory nerves. Assessing corneal sensation can help evaluate for peripheral nerve damage. Uveitis may be categorized as anterior, posterior, or panuveitis. o Anterior uveitis is visualized on slit-lamp examination as floating leukocytes and proteins from vascular damage, commonly referred to as "cell and flare." o • Posterior uveitis presents as leukocytes floating in the vitreous cavity (vitritis) or as areas of retinal whitening representing inflammation and necrosis in severe cases. Optic neuritis may be an associated finding as well. Every patient with HZO should undergo ocular tonometry to evaluate for elevated intraocular pressure (IOP). Elevated IOP due to HZO usually occurs secondary to zosterinduced trabeculitis. However, it may also occur due to obstruction of the trabecular meshwork from the inflammatory cell and protein debris or from the formation of synechiae as a consequence of extensive intraocular inflammation. Prolonged elevation in IOP may lead to secondary glaucoma. Go to: Evaluation HZO is primarily a clinical diagnosis based on history and classic findings on physical and slitlamp examination. Additional procedures, such as ocular tonometry and corneal esthesiometry, may be performed for a more thorough evaluation to assess for complications. Other diagnostic tests, such as viral cultures, polymerase chain reaction (PCR), and antibody testing, are rarely required to establish a diagnosis of HZO. For patients with disseminated herpes zoster (disease involving multiple dermatomes), severe illness, or those with significant risk factors, it is reasonable to consider HIV testing. Additional laboratory tests and imaging are seldom warranted.[14][15] Minor M, Payne E. Herpes Zoster Ophthalmicus. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557779/ DIFFERENTIALS https://emdaily1.cooperhealth.org/content/back-basics-ocular-herpes-simplex-vs-herpeszoster-ophthalmicus Herpes simplex keratitis vs Herpes Zoster Ophthalmicus Herpes Simplex Virus (HSV) Keratitis: • • Similarities: Can present with a painful red eye, corneal involvement, and vesicular rash. Differences: Usually affects younger patients and may recur more frequently than HZO. Dendritic ulcers are characteristic of HSV keratitis. Contact dermatitis • Similarities: Can present with erythematous and vesicular skin rash. • Differences: Usually has a history of contact with an allergen and does not follow a dermatomal distribution.