shenandoah-valley-gastroenterology-medical-history
advertisement

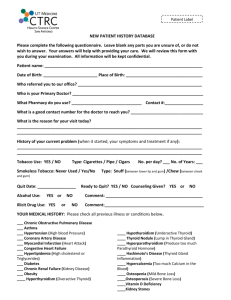
Shenandoah Valley Gastroenterology Center PLLC Please bring this completed form with you to your appointment. Appointment date: ______________ Arrival Time: ____________ Name (first, MI, Last) Date of Birth: PCP: How did you hear about us? Pharmacy name location and phone number: _______Male ______Female Referring MD: Reason for your visit and problems: Current and recent gastrointestinal problems: (Circle YES or NO for each) YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO YES or NO 1/5 Nausea Vomiting: If yes, with or without blood? Bloating Belching Acid reflux or heartburn Difficulty swallowing Barrett’s esophagus Hiatal hernia Ulcers H. pylori infection Decrease appetite or early satiety Abdominal pain Changes in bowel habits Diarrhea Constipation Blood in the stool Black tarry stools Hemorrhoids Rectal pain Colitis Crohn’s or Ulcerative colitis Celiac sprue Colon polyps Colon cancer Gallbladder problems Liver problems Pancreatic problems Leakage of stool Rectal Itching Dairy intolerance Patient Initial: _______ Prior Gastrointestinal procedures or imaging: YES Bring the official report if possible. / Date (M/Y)/ Place of Procedure / Indications or Findings Colonoscopy Upper endoscopy Sigmoidoscopy Capsule endoscopy Upper GI series Small bowel series Barium enema ERCP Endoscopic ultrasound Abdominal CT scan Abdominal MRI or MRCP Abdominal ultrasound HIDA scan Gastric emptying study Other: Your Past Medical History: □ Atrial fibrillation □ Heart attack □ Heart failure □ Heart Valve replacement □ Pacemaker/defibrillator □ High blood pressure □ Kidney disease □ Renal Dialysis □ Osteoporosis □ Diabetes I or II □ Asthma □ Sleep Apnea □ Home oxygen □ COPD □ Hyperthyroidism □ Hypothyroidism □ Any Cancer □ HIV / AIDS □ Anemia □ Blood Transfusions □ Stroke or CVA □ Seizures □ Alcoholism □ Tobacco use □ Depression □ Arthritis □ Pancreatitis □ Barrett’s esophagus □ Colon polyps or cancer □ Diverticulosis □ Gallstones □ Gastric/duodenal ulcers □ H. pylori □ C. Difficile □ Reflux/GERD □ Crohn’s /UC Are you pregnant? YES or NO or Uncertain Date of your last menstrual period? (M/D/Y) Seasonal allergies? YES or NO Other: Past Surgical History: 2/5 No surgical history Angioplasty Heart surgery Lung surgery Pancreatic Vaginal/ Bladder Ileostomy/colostomy Liver surgery Laparoscopy Vascular surgeries *Please Provide Month(M) and Year(Y) of the surgery* M/Y: Abdominal M/Y: M/Y: Cholecystectomy M/Y: M/Y: Appendectomy M/Y: M/Y: Hernia repair M/Y: M/Y: Hysterectomy M/Y: M/Y: Gastric band M/Y: M/Y: Gastric bypass M/Y: M/Y: Colon resection M/Y: M/Y Other: M/Y Patient Initial: _______ Family History: (Circle YES or NO for each) Unknown Family history Colon Cancer YES NO Relation(paternal or maternal): Colon Polyps YES NO Relation(paternal or maternal): Crohn’s or Ulcerative Colitis YES NO Relation(paternal or maternal): Liver Disease YES NO Relation(paternal or maternal): Gallbladder Disease YES NO Relation(paternal or maternal): Celiac Disease/ Gluten Intolerance Heart disease YES NO Relation(paternal or maternal): YES NO Relation(paternal or maternal): Diabetes YES NO Relation(paternal or maternal): Any other cancer YES NO Type and Relation: Social History: Current occupation / Employer: Marital status (circle one): Single, Married, Divorced, Separated, Partnered, Widowed Alcohol Use YES or NO Beer Drinks per week? ____________ wine Drinks per Month? ___________ liquor Last time you had a drink? ____________________ 3/5 Recovering alcoholic YES or NO When did you quit? Illicit drugs YES or NO When was the last time you used drugs and what type? Have you ever used a needle for drug administration? YES or NO Tobacco use YES or NO For how long? Tattoos YES or NO How many packs per day? Body area? Body Piercing YES or NO Body area? Diet products consumption Caffeine YES or NO Type? Quantity? YES or NO Type? Quantity? Patient Initial: _______ Do you have any of the following symptoms? (Mark all that apply) GENERAL Dentures Frequent UTIs Memory loss Weight loss _____lbs Weight gain _____lbs Fever/ Chills Nose bleeds Kidney stones Tingling Hearing loss Pregnant Numbness CARDIOVASCULAR MUSCULOSKELETAL Stroke Weakness Chest pain Neck pain Seizures Fatigue Chest pressure Back pain PSYCHIATRIC Night sweats Abnormal swelling of the legs Irregular heart beats Lightheadedness Joint pains Anxiety Stiff joints Depression Arthritis Scleroderma Vision loss Passing out/syncope RESPIRATORY Past evaluation and treatment ENDOCRINE Lupus(SLE) Excessive Thirst Use of glasses Shortness of breath SKIN Excessive Urination Glaucoma Wheezing Yellow skin Intolerance to cold ENT Asthma or COPD Rashes Intolerance to Heat Mouth ulcers Trouble breathing Psoriasis Teeth decay Cough Dermatitis HEMATOLOGY/ LYMPHATIC Bleeding problems Sinus problems GENITOURINARY Itching Transfusions Sore throat Blood in urine NEUROLOGICAL Miscarriages Hoarseness Burning urinating Headaches Large lymph nodes Insomnia EYES Yellow eyes 4/5 Patient Initial: _______ Please list ALL MEDICATIONS and ALLERGIES below or bring a list with you. Allergies: Do you have any known drug allergies? Any adverse reaction to sedation or anesthesia? Are you allergic to latex? Are you allergic to eggs or soy? YES YES YES YES Name of Medication Allergies or or or or NO NO NO NO Reaction MEDICATIONS LIST: (Including over the counter medications and natural remedies) Please list all medications or bring a list with you. Do you use any of the following medications? YES Medication name Blood Thinners: Coumadin warfarin, Plavix, Xarelto. Oral steroids Baby aspirin Regular aspirin, Aleve or Excedrin Ibuprofen(Advil/Motrin/ Naproxen) Laxatives Iron Calcium Multivitamins or natural remedies Other non prescription drugs Medication List Strength and dose How many time a day Strength and dose Times per day The information provided above has been accurately completed to the best of my knowledge: 5/5 ____________________________________________________________________ Patient Signature ________________________________ Date