Patient History Form - Texas Health Resources
advertisement

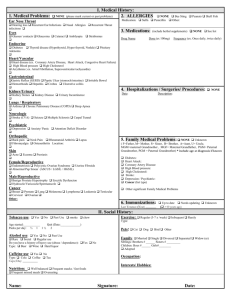
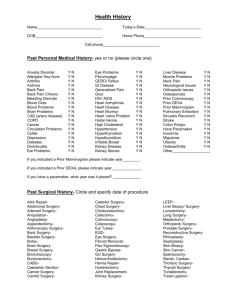
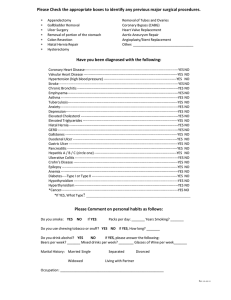
PATIENT HISTORY FORM Today’s Date: Click here to enter a date. DEMOGRAPHICS Name: Date of Birth: Marital Status: Single ☐ Married ☐ Widowed ☐ Separated ☐ Divorced ☐ Employer/Occupation: Primary Care Physician: MEDICATIONS Allergies to Medications: Current Medications: (List all; including ones not prescribed, such as alternative agents or herbal supplements) Drug Strength How Often You Take Per Day ILLNESS / HOSPITALIZATION Childhood Illnesses: Chicken Pox ☐ Measles ☐ Mumps ☐ Previous Medical Illness / Hospitalizations (other than surgery): -1- Rubella ☐ Scarlet Fever ☐ PATIENT HISTORY FORM Name: Date of Birth: SURGERY If yes, please check and give the approximate date of surgery in the corresponding blank. ☐ Gallbladder ☐ Hernia Repair ☐ Appendectomy ☐ Heart Angioplasty ☐ Tonsillectomy ☐ Heart Bypass ☐ Hysterectomy ☐ Pacemaker ☐ Mastectomy ☐ Other ☐ Tracheotomy ☐ Vasectomy ☐ Hip Replacement ☐ Knee Replacement FAMILY MEDICAL HISTORY Check the box next to the condition that your family member has; then specify their relation to you after the disease; using the abbreviations as follows (you can use more than one for each - please separate each additional entry with a comma): (M)-Mother (S)-Sister (PGM) Paternal Grandmother (MU) Maternal Uncle ☐ Alcoholism ☐ Anemia ☐ Asthma ☐ Arthritis ☐ Breast Cancer ☐ Colon Polyps (F)-Father (MGM)-Maternal Grandmother (PGF) Paternal Grandfather (PA) Paternal Aunt ☐ Diabetes ☐ Glaucoma ☐ Heart Disease ☐ High Blood Pressure ☐ Kidney Disease ☐ Migraines (B)-Brother (MGF) Maternal Grandfather (MA) Maternal Aunt (PU) Paternal Uncle ☐ Osteoporosis ☐ Prostate Cancer ☐ Stroke/TIA ☐ Thyroid Disease ☐ Cancer ☐ Other Enter "Other" Here Living Mother Yes☐ No☐ Father Yes ☐ No☐ Age or Age at Death Sibling (1) Yes ☐ No☐ Sibling (2) Yes ☐ No☐ -2- Present Health or Cause of Death PATIENT HISTORY FORM Sibling (3) Yes ☐ No☐ Name: Date of Birth: MEDICAL HISTORY Please check any of the listed items that apply to your medical history (past or present). ☐ Urinary Incontinence ☐ Blurred Vision ☐ Glaucoma ☐ Headaches ☐ Migraine Headaches ☐ Lumps or Swelling in Neck ☐ Constant Ringing in Ears ☐ Hearing Problems ☐ Frequent Earaches ☐ Frequent Nosebleeds ☐ Sinus Infections ☐ Allergies / Hay Fever Lungs ☐ Asthma ☐ Have Coughed up Blood ☐ Increasing Shortness of Breath ☐ Pneumonia ☐ Emphysema ☐ History of Tuberculosis ☐ Chronic Cough Heart ☐ Irregular Heartbeats / Palpitations ☐ Chest Pain or Tightness ☐ Heart Murmur / Valve Problems ☐ History of Enlarged Heart ☐ Swelling of Feet and Ankles ☐ History of Rheumatic Fever ☐ High Blood Pressure ☐ Previous Heart Attack Neuro. ☐ Seizures ☐ Loss of Consciousness ☐ Double Vision ☐ Memory Loss ☐ Numbness of Hands or Feet ☐ Stroke Kidney ☐ Recurrent Urinary Tract Infections ☐ Urination at Night More Than Once ☐ Blood in Urine ☐ Burning on Urination ☐ Kidney Stones ☐ Difficulty Starting Stream ☐ Problems with Sexual Function Head Abdomen ☐ Heartburn ☐ Difficulty or Pain Swallowing ☐ Have Vomited Blood ☐ Rectal Pain/Bleeding (Black Blood) ☐ Recent Changes in Bowel Habits ☐ Diverticulitis or Diverticulosis ☐ Colon Polyps ☐ Colonoscopy Click here to enter a date. ☐ Hepatitis / Yellow Jaundice ☐ Liver Disease ☐ Nausea ☐ Constipation ☐ Diarrhea ☐ Abdominal Pain ☐ Hemorrhoids ☐ Hernia ☐ Loss of Appetite Joints ☐ Back Trouble ☐ Swollen Joints ☐ Frequent Painful Feet ☐ Frequent Shoulder Pain ☐ Aching of Muscles ☐ Aching of Joints ☐ Gout ☐ Arthritis ☐ Osteoporosis General ☐ Diabetes (Diagnosed: Click here to enter a date.) ☐ Weight Loss or Weight Gain ☐ Fevers / Chills ☐ Night Sweats ☐ Sleeping Difficulty ☐ Sleep Apnea Choose an item. ☐ Thyroid Problems ☐ Increased Fatigue / Malaise ☐ Leg Cramps While Walking ☐ Depression ☐ Anxiety -3- PATIENT HISTORY FORM ☐ Anemia ☐ History of High Cholesterol ☐ Other Name: Date of Birth: MEDICAL HISTORY CONTINUED Males Only ☐ Weak Urine Stream ☐ Painful or Sore Genitals ☐ Prostate Issues ☐ Hard to Empty Bladder Completely ☐ Perform Self Testicular Exams Monthly ☐ Erectile Dysfunction Females Only ☐ Last Menstrual Period (Date: Click here to enter a date.) ☐ Vaginal Discharge or Problems ☐ Painful or Sore Genitals ☐ Lumps or Pain in Breast ☐ Last Mammogram (Date: Click here to enter a date.) ☐ Last Pap-Smear (Date: Click here to enter a date.) ☐ Perform Self Breast Exams Monthly ADDITIONAL NOTES / COMMENTS: -4- PATIENT HISTORY FORM -5-