Mock Inspection Template
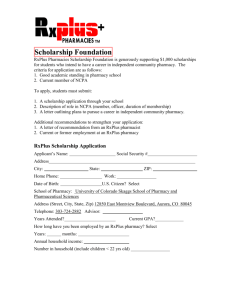
advertisement

Inspection Report Principle 1: Governance Arrangements Standard Risk Management 1.1 How are the What services are being provided? risks How do you ensure quality and safety of associated these services? with providing pharmacy services are identified and managed? What risk management measures would you take if you were to provide a new service? Do you have a regular review of adverse incidents? How do you report patient safety incidents? Examples of how to achieve Have documents ready to show e.g. PGD documents, NHS SLAs Training documents & certificates Risk assessments Have you initiated a new service? Facilities, equipment, staff, training, workload, etc Identify trends Review procedures Inform staff/recruitment of new staff Improvements to the design of the dispensary and/or service delivery, etc Do you have an incident report book/log? How are incidents reported Do you have Standard Operating Procedures in place? Can I view them? Read a SOP & ask a member of staff what it is they do & see if the two match up Have you had any dispensing incidents or near misses? Do you keep a log? Are these being followed? All staff working in line with SOPs Do all staff know where SOPs are kept Are staff named in the SOPs Are SOPs in date & regularly reviewed (every 2 yrs or following an incident) Is a log kept Are all errors logged? Including near misses & dispensing errors Reporting to the NPSA Comments Inspection Report What would you do in the event of a dispensing error going out to a patient? Is the near miss log regularly reviews? Is there a basket system in place? Is there a clear workflow/checking area? How do you maintain hygiene within the pharmacy? Do you have a cleaning rota? How do you dispose of medicines/sharps? Evidence of records/reporting Root cause analysis conducted? Examples: what did you do, how did you improve, how do you prevent it from happening again, what procedures have been put in place as a result of a review. E.g. moved similar sounding drugs, put markers on, work flow, dispensary benches, sufficient staffing Makes notes on the near miss log to show what changes you have made as a result of reviews Is there an infection control procedure in place Cleaning rota Sharps disposed of appropriately DOOP bins used & regularly collected How often are your DOOP bins collected? Can I see where you store unwanted medicines/patient returns? Look at how medicines are stored What are your date checking procedures? Are opened bottles of oral liquids marked with date of opening? Where is your CD cabinet? Where are fridge lines stored, explain the process of handling fridge lines? Is there a date checking matrix How does the pharmacy identify short dated stock? – do they mark packs When is stock with short expiry dates removed from shelves? How are CD’s stored? CD keys? In line with legal requirements? Is handling of fridge lines in line with SOP Unlicensed medicines should be Inspection Report How do you handle hazardous substances? Do you have any unlicensed medicines? Have you got a procedure in place in case there is a potential failure or disruption to services? segregated from other medicines 1.2 Is the safety & 1.4 quality of pharmacy services reviewed and monitored? Are feedback/ concerns about pharmacy services or staff can be raised by individuals/ organisations and action taken to Complaints & feedback How are complaints handled in the pharmacy? How are they acted upon? Is the complaints procedure advertised and proactively publicised? Ask a member of staff – do they know how a patient can make a complaint? Are patients asked for feedback on a regular basis? Has this lead to positive outcomes for patients? Contingency plan What are the arrangements of business continuity? Have these arrangements been tested? Alternative or replacement equipment and facilities are accessible/available There is sufficient capacity and skills/expertise to cope with both planning and unplanned staff absences/sickness There are alternative arrangements should the pharmacy premises cease to be fit for purpose Complaints procedure in place Record of complaints Complaints dealt with in a timely manner Complaints procedure should be outlined in the practice leaflet All staff need to be aware of the complaints procedure Patient survey conducted annually – these results should be published & feedback taken onboard Staff need to have examples at hand of feedback they have given to management & changes which have been implemented as a result Staff meetings & outcomes if you have any Inspection Report remedy them Is feedback shared within and outside the pharmacy? Is staff feedback taken onboard? Patients can provide feedback on the pharmacies NHS Choices profile Analysis of complaints made to identify trends & detect improvements to be made – conduct annually Ask a member of staff – example of when you have suggested something which was implemented? 1.3 Do staff have clearly defined roles and clear lines of accountability? Do you feel comfortable giving feedback to management & suggesting changes? Is there an appropriate skill mix in the pharmacy? Are staff roles reviewed on a regular basis? Are staff roles changed to meet the needs of services or emerging needs of patients? Give examples? Do staff have development plans in place? Where tasks are delegated to other members of the pharmacy team, what risk management procedures are in place? Are there clear lines of accountability and roles? Responsible Pharmacist Regulations Are all procedures being following? Pharmacy log – is the pharmacist signing in What training is provided to staff What staff roles are there in the pharmacy Job descriptions – are these evaluated & developed Do staff clearly understand their job role & do not operate outside of their competencies Risk manage staff operating outside of their role – are they competent to carry out this role? Dispensing process – are the dispensed and checked boxes signed on dispensing labels to be able to have an audit trail Are staff contracts in place? Are staff following SOPs Log to be kept for 5 years Sign in and out at the beginning and end of the day Record absences – good practice to Inspection Report and out everyday, are absences recorded? record reason (max 2 hours) RP SOPs to be kept for 15 years Do you have indemnity insurance in place? Certificate in date Are all legally required records kept? Specials Service records e.g. PGDs, SLAs POM register – Private rx, Emergency supplies Extemp dispensing Responsible pharmacist record CD register Destruction of patient returned Schedule 2 CDs Others: date checking, cleaning, fridge temp, calibration, recalls, alerts Is the responsible pharmacist notice displayed? Responsible pharmacist SOPs – are they in place? Ask a member of staff – what would are the procedures to follow if the responsible pharmacist is absent from the pharmacy? 1.5 Are indemnity/ insurance arrangements in place 1.6 Is record keeping relating to the safe provision of pharmacy services in place? 1.7 How is information managed to protect the privacy, dignity Can I see your records for specials products? What other record keeping documents are in place? How is your PMR backed up? Ensure records are clear, legible, accurate, up to date and available at the registered pharmacy What security arrangements do you have in place? How is confidentially maintained? IG regularly audited & updated Storage & accessibly of computers & laptops Protecting patient sensitivity information Public should not be able to access Inspection Report & confidentiality of patients/ public Have staff been trained on information governance? Are there passwords on computers? Who has access? Are passwords regularly changed on the PMR system? Are smartcards stored securely? prescription medicines Shop security – alarm, etc Procedures must be in place to ensure patient identifiable information is not shared intentionally or unintentionally Any confidential information stored in area where public have access e.g. consultation room – if so is the room/cupboard kept locked? Confidential waste? Can I see your practice leaflet? – look for data protection compliance publication 1.8 How are children & vulnerable adults safeguarded? Does confidentially data ever leave the pharmacy? If so how is it managed? Procedures in place for this? What procedures do you have in place for safeguarding of children & vulnerable adults? Are systems in place to ensure safeguarding? Who would you report to if you have a concern? What is the reporting procedure? Do you give consideration to children & vulnerable adults when services are developed? SOP in place Staff need to know when, where and who to report concerns to Children & vulnerable adults are to be treated with respect & information is provided to them in such a way that it is understood Consider these groups when developing services Groups treated with respect and made to feel safe See PharmaPlus procedures for further information & examples Inspection Report Principle 2: Empowered & Competent Staff 2.1 Are sufficient How many staff are present in the staff available pharmacy? to provide pharmacy Do they have an appropriate skill mix to services safely, provide pharmacy services safely? with appropriate Are staff suitably trained? skills and qualifications? 2.2 Do staff have the appropriate skills, qualifications and competence for their role/ task or, if in training are they working under the supervision of another person Does learning and development take place for all staff? Is there an induction procedure for staff? Is there an appraisal system? Do staff reflect on their own performance and identify learning and development needs? And are they supported to address them? Does the pharmacy encourage, support and provide access to CPD/continuous education Continuous learning taking place Staff have appropriate skills to reflect services being provided In order to qualify for a Practice Payment, the NHS Pharmacy Contract requires contractors to have minimum numbers of dispensary staff in place linked to the number of items dispensed Staff certificates available? Using GPhC approved programmes or approved sources e.g. CPPE Evidence of staff currently undergoing training Development plans in place Keep training matrix for every member of the pharmacy team Staff performance should be regularly reviewed Signed staff contracts in place & induction pack including a locum agreement & locum guide Staff have appropriate registration & evidence of training/competence for carrying out services (e.g. MURs, substance misuse) – these should be reviewed regularly Evidence of appraisals & learning development & personal development plans Staff know their roles Competency of staff is reviewed regularly Inspection Report 2.3 Compliance with professionals/ legal obligations and empowerment to exercise professional judgement in interests of patients/ public Are pharmacy professionals and staff supported and empowered to make decisions and act proactively for the benefits of their patients and the public and other members of staff? Is there a sale of medicines protocol in place which staff follow 2.4 Is there a culture of openness, honesty and learning Does the pharmacy ensure that the pharmacy team learns and improves? Are staff fully involved in improving delivery of pharmacy services? Do staff understand their own and other HCP’s legal and professional obligations when providing pharmacy services? Near miss/incident logs – can provide learning for staff Staff can describe their suggestions for improvements to pharmacy services as a result of training and development E.g. OTC product training sessions leading to increased knowledge to advise patients/ refer Decision making should be proactive and professional Pharmacy procedures should be understood by staff and followed Senior members of staff with management responsibilities are able to professionally and legally fulfil their duties with the correct authority Do staff have appropriate reference sources available to them in the pharmacy? E.g. BNF, counter assistants reference sources, DT, etc Are mistakes learnt from Shared learning from mistakes – open discussions – is there evidence of this Errors, incidents and near misses are regularly reviewed and work systems & processes modified accordingly to reduce the recurrence of similar incidents Are patient safety incidents reported to the NPSA and a log kept in the pharmacy Staff to accept responsibility for their mistakes and are involved in action taken to prevent similar occurances Inspection Report 2.5 Are staff empowered to provide feedback and raise concern about meeting these standards and other aspects of pharmacy services 2.6 Are incentives being offered which may compromise patients or the publics health, safety or wellbeing and professional judgement Do staff feel empowered to suggest changes or provide feedback to senior members and raise concerns? Do staff know about the whistleblowing policy? Staff to be encouraged to raise concerns where actions of others or procedures in the pharmacy may put others at risk Staff are confident in using the whistleblowing policy and are encouraged to do so Are staff opinions and feedback regularly sought in order to reduce risk and make improvements to patient/public services What targets and incentives does the pharmacy have in place/provide staff Check targets/incentives are appropriate and staff are not expected to act other than within their professional judgement and the interests of the patient Demonstrate patients are not at risk due to incentives or targets Inspection Report Principle 3: Managing pharmacy premises 3.1 Is the premises Is the building safe and well maintained? safe, clean and properly Is repair work/maintenance carried out maintained safely and in a timely manner? and suitable for the Are patients given advance notice of planned pharmacy maintenance work and provided with services appropriate information? provided? Designs & layout of the premises: Sufficient size for the services offered? Is there a consultation room – built to correct specifications to enable provision of pharmacy services? Equality Act – how does the pharmacy premises support patients with disabilities Does patient and public feedback inform the design and layout of the public area of the pharmacy? Is there a health & safety policy in place? Is health and safety law being followed? Fire safety? Appropriate lighting, heating, plumbing, alarm system – regularly tested? Signposting, how will services be affected, how long these services will be affected for Professional looking pharmacy premises Clean, tidy, well organised All pharmacy fixtures & fittings are well maintained and kept in good order Business continuity plans are in place with contact details of local contractors e.g. plumbers & electricians Sufficient dispensary space for checking prescriptions or preparation of monitored dosage systems Dispensing workflow – should not be obstructed by cramped conditions, particularly when the pharmacy is fully staffed during busy periods E.g. provision of ramps, hearing loops, aisles/doorways wide enough for wheelchairs/pushchairs Sufficient and appropriate space should be available to store stock awaiting collection or delivery, particularly large bulky items Sufficient storage available for stock Stock should not be stored on the floor e.g. where there is risk of unauthorised access Stock should not be stored in area that Inspection Report 3.2 Does the design of the premises protect the privacy, dignity and confidentiality of patients 3.3 Is there an appropriate level of hygiene maintained, depending on services offered? Consultation room available? Is it clearly signposted & promoted by staff during conversation with patients? Look out for use of the consultation room Is the pharmacy clean, tidy and well organised? How often is the pharmacy cleaned? Are floor spaces kept clear? Ceilings and walls well maintained? Clean sink 3.4 Are the What security features are present in your may be subject to temperature variations e.g. top shelves or next to a refrigerator May be other quiet areas in the pharmacy away from the main pharmacy counter where patients can discuss their medicines Layout of the pharmacy allows patient confidentiality and privacy to be protected Staff and patients are able to have confidential conversations IG SOPs are in place Staff have signed confidentiality clauses Infection control procedures in place Cleaning rota Cleaning equipment readily available and used and appropriate signage is in place (e.g. reminding staff to wash hands) Regular removal of waste – waste containers are filled to the appropriate fill line Contact details of waste contractors/pest control are available All areas of the pharmacy need to be clean/hygienic – stock room, kitchen, toilet, etc Adequate sink/hand basins with hot and cold water supplies are provided in appropriate areas to allow hygienic preparation of medicines, cleaning/sanitation and hand washing Locks/alarms/shutters/CCTV Inspection Report premises secure and safeguarded from unauthorised access? premises? How often are these security features reviewed? Is excess stock kept in a secure area? Access from the back of the pharmacy? Who holds keys to the pharmacy? Controlled Drugs: How are the CD keys stored – during the day & overnight? What is your procedure for destruction of CD’s? Records? T28 exemption? Is your CD register up to date? Balances well maintained? Balance checks occurring? Windows/hatches – locked Working alarm systems – cover all areas of the pharmacy Emergency call out procedure is in place Evidence of reviews following a breach in security and action taken Follow all controlled drug regulations CD keys to be kept on the pharmacist during the day At night should be stored securely – e.g. in a bag, stapled, signed & dated by the pharmacist & stored securely CD destruction kits should be available Balance checks should be occurring in line with SOPs Check CD cupboard – bagged prescriptions, out of date medicines, CD storage, solely used for CDs Is the CD cupboard bolted to the wall? Do you have the details of your accountable officer? 3.5 Are pharmacy How are CDs delivered to patients – what is your procedure? Working Area: Ambient room temperature is Inspection Report services provided in an environment that is appropriate for the provision of healthcare? Is there sufficient lighting and ventilation? How do you maintain the temperature in the pharmacy? What happens if the pharmacy temperature increases above 25C? Are there any distractions in the pharmacy e.g. audio/video equipment? Professional area: Is there a clearly defined professional area? Are medicines in this area healthcare related? E.g. alcohol and tobacco is not sold External Areas: What posters/campaigns are running? Are they relevant? Kept up to date? What is displayed in the shop, windows, doors? Does it create a professional appearance? Shop front signage needs to be professionally displayed Are pharmacy opening hours displayed? maintained at a level to ensure medicines remain fit for purpose and services can be provided comfortably Temperature control: AC unit, fans, windows – monitor using thermometers Volume levels of audio/video equipment being used in the pharmacy should be appropriate and not form a distraction to offering pharmacy services Confectionary not to be kept near the pharmacy counter Appearance of the premises presents a professional image for the provision pharmacy services Inspectors will examine all material – ensure you have relevant campaigns running Windows are not cluttered – keep it professional Inspection Report Principle 4: Delivering Pharmacy Services 4.1 Are the How are your services advertised? pharmacy services How do you choose what services you provided provide? accessible to patients and Do you provide services to fit the health the public needs of the local community? If your pharmacy is in an area where there is a large community who do not speak English how do you provide services to these patients? What facilities do you provide for disable patients? Is seating available for patients? Signposting – does this occur when you are unable to provide a pharmacy service? 4.2 How are pharmacy services managed and delivered safely and effectively? TELL THE INSPECTOR ABOUT ALL YOUR SERVICES!!!! Pharmacy services available are clearly displayed, up to date and actively promoted Practice leaflet – accurate & on display Services should be provided to fit the needs of your local community – have examples ready Bilingual leaflets Multilingual staff Staff should be clearly identifiable – e.g. uniforms & staff badges to indicate name & job title/role Seating should be available to assist those who may find it difficult to stand Clear lines of accountability – who is responsible for what? SOP on signposting in place Patients are referred/signposted to other appropriate health and social care providers or support organisations, when the pharmacy cannot meet their needs Make SOPs available for services Are staff following SOPs Local PGD protocols being followed Audit trails Use of baskets in the dispensing process Monitored dosage systems: Are PILs being put in patients bags? Ensure all points are fulfilled Ensure staff have relevant qualifications Are staff aware of when, where and who to signpost to? Do you have SOPs in place for all services provided? Inspection Report Staff to ensure hygiene when preparing MDS E.g. anticoagulants, opioids, oral methotrexate, insulin SOPs in place for dispensing these medicines? Are tablet shape/colour/markings/ etc recorded on the MDS Are warning labels put on the MDS (label requirements) Who has dispensed & checked the MDS – marked on MDS? Ensure preparation of MDS fulfil hygiene requirements Qualified member of staff to prepare MDS to patients? High Risk medicines: How do you identify patients taking high risk medicines? Are these patients proactively targeted & suitably counselled? Are patients with conditions such as diabetes, CHD, high BP, smokers & overweight patients proactively targeted for health promotion and healthy lifestyle advice? Evidence of health promotion in the pharmacy Stock Management: Is stock which is safe and appropriate to sell clearly segregated from that which is not? This could be done when handing out medicines, by counter staff, during MURs, NMS, etc Should participate in public health campaigns & local campaigns SOP – Safe storage of medicines Stock rotation system Managing expiry dates e.g. marking boxes Inspection Report Stock rotation system is in place? How are out of date medicines handled? Or those nearing their expiry date? Are oral liquids marked with date of opening/ expiry dates? Date checking matrix Ensure procedures are in place to keep owing items to a minimum & manage long term out of stock medicines Patients informed if medicine is short dated & provided with medicines with a sufficient shelf life How are owings managed – in line with SOP? What procedures are in place to manage long term out of stock products? Deliveries: How are your deliveries made? Do you have a record book? Record book to be kept & all deliveries to be logged Controlled drug procedures to be followed Cold chain maintained Do you deliver controlled drugs? What are your procedures? How do you maintain the cold chain of products? Are audits conducted annually 4.3 Medicines & medical devices How do you ensure you only obtain products from a reputable source? Contract monitoring requirement – one NHS England lead & one practice based audit to be undertaken Perform background checks Only use reputable wholesalers Check WDLs Maintain audit trails How do you file/store your invoices? Are your medicines safe and fit for purpose? Ensure stock is not stored in a location How are your medicines sourced? Inspection Report How are your medicines stored? How do you ensure ambient temperature is maintained? Do you monitor the temperature? What would you do if the temperature fell outside its range? How do you ensure correct storage of fridge lines? Do you ensure daily monitoring of fridge temperatures – can I see the log? Is your thermometer calibrated in line with manufacturers instructions? Look in the fridge – ensure medicines are stored appropriately – is there any food stored in the fridge? How are cytotoxic medicine stored and handled? Separate counting triangles? Are hazardous substances correctly handled and stored? Are medicines stored in their original packaging? If some are not are they marked with batch numbers and expiry dates? Are medicines sold/supplied in appropriate containers? – observe which may be affected by extremes of temperature Medicines are not to be stored on the floor Know procedures for dealing with medicines when they are exposed to temperatures outside of ranges Procedures on how to deal with temperatures when they go above 25C – AC, fan, windows, etc Fridge – back up fridge – how long has the temperature been out of range – what do you need to do with the stock Food must not be stored in the fridge with medicinal products Odd tablets should not be transferred from their original pack into another pack Separate counting triangles for cytotoxics Inspection Report Are they correctly and securely stored in line with their legal category? Are your medicines stored securely? Are they safeguarded from unauthorised access? Controlled drugs - who has access & keys? Medicines are supplied safely and accurately and appropriate to patients individual needs? Are patients given correct information on treatment and use of medicines & medicinal devices? How do you dispose of waste? Do you have appropriately coloured DOOP bins? Yellow sharps bins? Are they stored securely & used correctly? Where are patient returned medicines kept? How are they handled when received? Are patients actively counselled to promote the return of unwanted/unused medicines/ medical devices? See above with regards to controlled drugs Are loading areas for deliveries secure? Are patients able to access POMs ? Access to the dispensary and medicines is restricted to authorised staff Ensure staff are following sales protocols & referring to the pharmacist when necessary Using WWHAM questions Patients/carers are given information/ advice so that they can make informed decisions when purchasing medicines Counselling and advice is provided to ensure effective and safe use of medicines, devices & pharmacy services Staff asking patients about returned medicines before accepting them e.g. are there sharps contained in these returns, CDs, etc IG SOPs in place T28 exemption for destruction of CDs to be in place Battery recycling facility is available if more than 32kg of portable batteries are sold per year – promotion to public where appropriate How often is waste collected – ensure a suitable collection time Inspection Report Consignment notes are to be kept for 3 years Quarantine Relevant authorities notified Raise concerns with other pharmacies/ prescribers/ manufacturers Pharmacy should proactively follow up patients who have received a product not fit for purpose Yellow card reporting scheme Legal requirements for CDs followed? Is confidentiality of patient returned medicines/ devices protected? Is patient returned medicines and out of date stock segregated from normal pharmacy stock? 4.4 Are concerns raised when it is suspected that medicines or medical devices are not fit for purpose? Disposal of waste is in line with environmental guidance How are defective/ counterfeit/ medical devices dealt with? Do you have a SOP in place for dealing with drug alerts? Do you have a record of drug alerts actioned upon? Inspection Report Principle 5: Equipment & Facilities 5.1 Do you have Do you have a private consultation area? equipment and facilities Do you have up to date reference sources needed to available? provide pharmacy Does the pharmacy have internet access to services readily be able to view the most up to date available? resources & receive email alerts? Consultation area – to the specifications BNF, Drug Tariff, Stockley’s drug interactions, Martindale Equipment: Dispensing baskets, calibrated scales, glass measures (CE marked), counting triangles, MDS equipment, gloves, aprons, cleaning equipment, fridge, etc Do you have appropriate equipment to be able to provide services? Is seating available in the pharmacy? Do you have facilities to accommodate patients needs? Support for patients with disabilities? 5.2 Are your equipment and fit for purpose? Is your equipment obtained from a reputable source? What equipment do you have to provide your services? Is your equipment safe to use and fit for purpose? Does regular cleaning of equipment occur? All equipment should be clean and hygienic E.g. large print labels, product labels in different languages, print PILs in large print E.g. availability of induction (hearing) loop Equality Act – procedures and assessments Use recognised suppliers Installation by a recognised company Medical devices should have a CE mark Measures should not be chipped – clean and well maintained Calibration & servicing to occur in line with manufacturers recommendations Measures should be cleaned between uses Tablet counters cleaned regularly Methadone measures not to be used for Inspection Report Do you service/calibrate your equipment? And how often does this occur? Do you have records/certificates of calibration? If deficiencies are found – what corrective action is taken? Is the equipment appropriately maintained? Is seating provided? Clean & safe Are your equipment and facilities proactively reviewed to improve patient care? Example 5.3 Are equipment and facilities used in a way that protects the privacy & dignity of the patients and the public who receive pharmacy services? Are concerns raised when not fit for purpose? Is equipment stored securely to prevent unauthorised access? Where are sharps stored? Storage and access to smartcards? Password protection? Are computer passwords regularly changed? Where are prescriptions & registers stored? How do you prevent disclosure of confidential information: PMR screen positioning? Prescription retrieval system? other medicines Electrical equipment to be kept away from sink areas Pharmacies should share concerns with other pharmacies/ organisations to raise awareness of equipment deficiencies Patient feedback taken on board to improve facilities, equipment, services, etc in order to improve patient care Serviced/maintained by a reputable company if appropriate – these details should be made available in case of an emergency/breakdown/ failure of equipment Business continuity Sharps should not be stored where patients can gain access to them –should be stored safely and securely IG SOPs Inspection Report Passwords? Shredding? Locked cabinets? Etc? NOTE: To be rate POOR – a pharmacy will have to be failing significantly and be putting patient safety at risk Want to see outcomes from procedures put in place Need to tell the GPhC what you are doing in your pharmacy – why you are great, how are you serving the local needs of your community – don’t wait for them to ask! Think of examples for the questions they will be asking in advance – the more examples you have the higher your rating will be! At the end of the inspection the inspector will go through their findings with the Responsible Pharmacist, who will be asked to sign the report to confirm their agreement to the findings. The Responsible Pharmacist has an opportunity to make any additional comments. This is important to show that the evidence recorded on the report is an accurate reflection of what the inspector saw / was shown on the day. The Responsible Pharmacist is not signing to agree to an inspection judgement, which will not be made until after the inspection. Reports: Superintendents will have 2 days to confirm the report is accurate 2 days to respond to the action points Agreed timeframe for actions points will be set Action points may just require email confirmation or another inspection may take place The superintendent is responsible for the action plan