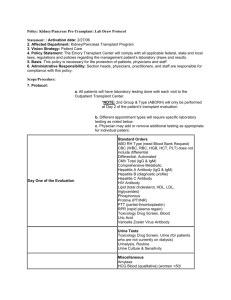
Immuno TB Flashcards Unit 4
advertisement

Immuno TB Flashcards Unit 4 1) The most likely reason for the development of an IgE antibody response in humans is: A) protection against helminth infections B) protection against bacterial diseases C) protection against viruses D) protection against allergens 2) Which statement best describes antigenic variation seen in parasites? A) The host immune system can respond more quickly. B) Different parasites have different antigens. C) Parasites can periodically change their surface antigens. D) Parasites become sequestered in host cells. 3) A host's immunological response to parasites includes all of the following EXCEPT: A) formation of IgG, IgM, and IgA antibodies B) production of cytokines C) gamma-interferon production by natural killer cells D) sequestering the parasite in host cells 4) In an individual with AIDS, what is the most likely reason for a toxoplasmosis infection that invades the central nervous system? A) The host produces a lot of antibody. B) Cysts in the tissue become reactivated. C) The individual ingests contaminated water. D) The parasite has acquired new surface proteins. 5) A 25-year-old pregnant female has serologic testing to determine if she has a toxoplasmosis infection. A low level of both IgM and IgG is found. On repeat testing 2 weeks later, the results are the same. What can be concluded from these results? A) She has an active infection. B) The baby will have serious central nervous system damage. C) She was exposed to toxoplasmosis at some time in the past. D) She has never been exposed to toxoplasmosis. 6) A 30-year-old male patient with AIDS exhibits pulmonary symptoms that include coughing and some difficulty breathing. The patient reported that he had previously worked in a bakery. His white blood cell count was normal, indicating that the infection is not bacterial in nature. Tests for the presence of fungal antigens were performed with the following results: ouchterlony immunodiffusion negative for antibodies to Aspergillus; negative latex agglutination test for Candida antigen, and positive EIA test for the galactomannan antigen of Aspergillus. What conclusion can be reached from these results? A) The galactomannan is a false-positive result. B) The infection is likely caused by Aspergillus. C) The Candida antigen test is a false-negative D) An Aspergillus infection is ruled out due to negative antibody testing. A C D B C B 1 Immuno TB Flashcards Unit 4 7) All of the following may be drawbacks of antibody testing for fungal infections EXCEPT: A) The patient is immunocompromised. B) Serologic tests may not be positive at a particular stage of the disease. C) Presence of antibodies may not indicate an active infection. D) False-positive results occur often in patients with functioning immune systems. 8) Why is testing for Cryptococcal antigen preferred over testing for antibodies? A) This is usually not a humoral response to infection. B) Immunocompromised patients do not produce antibody. C) Subclinical infection can be detected. D) all of the above 9) When is antibody testing for Cryptococcal antibodies most useful? A) in determining patient prognosis B) in diagnosing immunocompromised patients C) in ruling out the disease in young patients D) as a screening test after exposure to the fungus 10) What would be an advantage of using the tube precipitation test for diagnosis of infection with Coccidioides immitis? A) It is good at detecting IgG antibodies. B) It detects early IgM antibodies. C) It is subject to cross-reactivity. D) It is subject to anticomplementary reactions. 11) A patient is suspected of having latent syphilis. Which set of test results for RPR, MHA-TP, and CSF-VDRL best confirms this diagnosis? A) RPR = R-8 dils; MHA-TP = reactive; VDRL = R-4 dils B) RPR = nonreactive; MHA-TP = reactive; VDRL = nonreactive C) RPR = nonreactive; MHA-TP = nonreactive; VDRL = nonreactive D) RPR = R-2 dils; MHA-TP = nonreactive; VDRL = nonreactive 12) The RPR and VDRL tests differ from each other in which of the following ways? A) method for reading or visualizing the reaction B) specificity of antibody detected C) specificity of antigen detected D) principle for detecting antigen–antibody complexes 13) RPR stands for A) reagin plasma reactive B) reactive phosphate reagent C) rapid plasma reagin D) random positive reagin 14) The RPR and VDRL are similar in which of the following ways? RPR and VDRL are both: A) read macroscopically B) flocculation reactions C) specific assays for syphilis D) antigen detection assays D D A B B A C B 2 Immuno TB Flashcards Unit 4 15) Which of the following is a cause of a biological false-positive in the screening assays for syphilis? A) prozone B) reagents too cold C) sera dried on card D) autoimmune disease 16) A laboratory test that is used to confirm syphilis and detects specific treponemal antibodies is: A) VDRL B) MHA-TP C) RPR D) monotest 17) Which of the following is a cause of a laboratory-induced false-negative in the screening tests for syphilis? A) Alcohol ingestion prior to blood draw B) Systemic lupus erythematosus C) Excess serum D) Hot laboratory 18) Which of the following is a cause of a biological false-negative in the screening tests for syphilis? A) Rotated too long B) Rheumatoid arthritis C) Latent syphilis D) Low rotator speed 19) At which stage of syphilis is the RPR specific for syphilis? A) Primary B) Secondary C) Tertiary D) Latent E) None of these 20) At which stage of syphilis is the RPR the most sensitive? A) Primary B) Secondary C) Tertiary D) Latent 21) A patient has a reactive RPR at a titer of 1:128 and a reactive MHA-TP. What does this indicate for the patient? A) True-positive diagnosis of syphilis B) False-positive diagnosis of syphilis C) True-negative ruling out syphilis D) False-negative ruling out syphilis D B C C E B A 3 Immuno TB Flashcards Unit 4 22) Patient serum is mixed with sheep red blood cells that have been sensitized with Treponema pallidum antigens as well as with unsensitized red blood cells in a separate well. Agglutination was observed in the well with sensitized red blood cells and not in the well with unsensitized red blood cells. What is the interpretation of these results? A) Positive for anti–Treponema pallidum antibodies B) Positive for heterophile antibodies C) Negative for anti–Treponema pallidum antibodies D) Negative for anticardiolipin antibodies 23) A 25-year-old patient presents with a fine rash on his chest, palms and feet, fever and malaise. The RPR is reactive with a titer of 1:64, the VDRL is non-reactive, and the MHA-TP is positive. What is the diagnosis? A) Primary syphilis B) Secondary syphilis C) Tertiary syphilis D) Latent syphilis 24) A patient is diagnosed with syphilis. Which of the following laboratory tests can be used to monitor the effectiveness of therapy in this patient? A) RPR B) MHA-TP C) C-reactive protein D) Mono test 25) A patient presents with a painless genital ulcer. The patient is then diagnosed as having syphilis. In what stage of syphilis is the patient? A) Primary B) Secondary C) Latent D) Tertiary 26) A patient presents with personality changes, altered mental state, and delusions of grandeur. The patient is then diagnosed as having syphilis. In what stage of syphilis is the patient? A) Primary B) Secondary C) Latent D) Tertiary 27) A new technologist is busy one night and has to perform an RPR on a serum sample. He does not calibrate the needle delivering the antigen and the needle is delivering a larger volume of antigen than it is supposed to. What kind of error can this cause on the test result? A) Laboratory-induced false-negative due to postzone B) Laboratory-induced false-positive due to prozone C) Biological false-positive D) biological false-negative A B A A D A 4 Immuno TB Flashcards Unit 4 28) A 32-year-old heterosexual male presents to the physician with a 3-day history of multiple skin lesions located all over his body and on his mucous membranes. He hasn't felt well and has a low-grade fever. The patient cuts down trees in Massachusetts for a living. He is single, has had multiple sex partners, and does not use condoms. Here are the results of his laboratory tests: rapid plasma reagin = reactive 1:128; Treponema pallidum–particle agglutination assay = reactive; Borrelia burgdorferi IgM = < 1:8; Rickettsia rickettsii IgM < 1:8. This patient has: A) Primary Syphilis B) Secondary Syphilis C) Lyme Disease D) Rocky Mountain spotted fever 29) Lyme disease is caused by: A) Treponema pallidum B) Borrelia recurrentis C) Leptospira autumnalis D) Borrelia burgdorferi 30) A 30-year-old man presents to the physician with a painless ulcer on his penis. An RPR performed on the man is reactive 1:128, and the MHA-TP test is positive. This man has: A) Neisseria gonorrhoeae B) Chlamydia trachomatis C) Treponema pallidum D) Mycoplasma hominis 31) Which best describes the antibody called reagin found in syphilis? A) It reacts with cardiolipin B) It is specific for treponemal antigen. C) It appears in all patients within 7 days after exposure to syphilis. D) It is detected by the FTA-ABS test. 32) Which of the following may characterize the disease process in syphilis? A) Generalized rash B) Period of latency C) Localized chancre D) All of the above E) All except one of the above 33) Lab results on a patient indicated a positive RPR and a negative FTA. The patient had no obvious sore, rash, or other symptoms. What is the most likely cause of these results? A) Primary syphilis B) Secondary syphilis C) Tertiary syphilis D) Another disease, such as mono 34) Which of the following is a test for specific treponemal antibody? A) VDRL B) RPR C) FTA- ABS D) All of the above B D C A D D C 5 Immuno TB Flashcards Unit 4 35) Which of the following is a confirmatory test for syphilis? A) Rapid Plasma Reagin B) fluorescent antibody (FTA) C) VDRL D) All of the above 36) Which best describes the antibody known as reagin? A) It occurs only in the disease syphilis. B) It is tested for using charcoal and cardiolipin. C) It is found in all patients with primary syphilis D) It is antibody directed against IgG. 37) In an indirect fluorescent immunoassay such as the FTA confirmatory test for syphilis, all of the following are true EXCEPT: A) A labeled antigen is used. B) Washing is an important step. C) Patient antibody is detected. D) Antihuman globulin has a fluorescent tag. 38) A patient has a hepatitis B profile performed and is positive for hepatitis B surface antibody only. This patient: A) was vaccinated against hepatitis B) had a previous hepatitis B infection C) is a chronic carrier of hepatitis B D) has acute hepatitis B 39) Which is the first detectable antibody in serum after infection with hepatitis B? A) anti-HBs B) anti-HBe C) anti-Hbc D) all are detectable at the same time 40) Which of the following positive antibody tests may be an indication of recent vaccination or early primary infection for rubella in a patient with no clinical symptoms? A) only IgG positive B) only IgM positive C) both IgG and IgA antibodies positive D) fourfold rise in titer for IgG 41) A patient has the following serologic profile: HBsAg = negative; HBeAg = negative; anti-HBc IgM = negative; anti-HBc IgG = positive; anti-HBs = positive; anti-HBe = positive. These results indicate: A) early acute HBV infection B) chronic infection with HBV C) a patient vaccinated against HBV D) past infection with HBV B B A A C B D 6 Immuno TB Flashcards Unit 4 42) In infectious mononucleosis, which of the following would be detectable earliest in the infection, thereby indicating a current infection? A) anti-EA-IgG B) anti-EBNA C) anti-VCA-IgM D) anti-VCA-IgG 43) Serologic test results indicating that a patient is a chronic carrier of hepatitis B would be which of the following? A) HBsAb positive; HBsAg negative B) HBcAb and HBsAb positive C) HBsAb negative; HBsAg positive for 12 months D) HBeAb and HBeAg negative 44) In the routine diagnosis of hepatitis C virus, which type of laboratory test should be ordered first? A) antigen detection in liver biopsy B) antibody detection in blood C) viral culture of stool D) viral culture of biliary drainage 45) A patient has detectable levels of IgG and IgM against the viral capsid antigens of Epstein-Barr virus (EBV). This patient has: A) been infected with EBV in the past B) an infection with HIV, too C) a current infection with EBV D) never had EBV 46) A patient has the following hepatitis profile: anti-HAV IgM = not detected; HBsAg = not detected; anti-HBc IgM = not detected; anti-HBc total = not detected; anti-HBs = detected; anti-HCV = not detected. What is his diagnosis? A) acute hepatitis A B) acute hepatitis B C) chronic hepatitis B D) immune to hepatitis B 47) A 36-year-old African American male presents to a free clinic with symptoms of anorexia, malaise, vomiting, abdominal pain, and mild jaundice. The patient is a known IV drug abuser. The physician orders liver function tests and an acute hepatitis serum panel. The laboratory reports the following results: anti-HAV IgM = not detected; HBsAg = not detected; anti-HBc IgM = not detected; anti-HBc total = detected; anti-HBs = detected; anti-HCV = detected. This man has: A) acute hepatitis B B) chronic hepatitis B C) acute hepatitis A D) acute hepatitis C C C B C D D 7 Immuno TB Flashcards Unit 4 48) A patient was diagnosed with acute hepatitis B infection 9 months ago and has followup testing performed today. The following results are obtained: anti-HAV IgM = not detected; HBsAg = not detected; anti-HBc IgM = not detected; anti-HBc total = detected; anti-HBs = detected; anti-HCV = not detected. What is the diagnosis now? A) acute hepatitis B B) chronic hepatitis B C) chronic hepatitis C D) convalescent hepatitis B 49) A patient has the following hepatitis profile after presenting with jaundice, nausea, and vomiting: anti-HAV IgM = detected; HBsAg = not detected; anti-HBc IgM = not detected; anti-HBc total = detected; anti-HBs = not detected; anti-HCV = not detected. What is his diagnosis? A) acute hepatitis A B) acute hepatitis B C) acute hepatitis C D) chronic hepatitis B 50) A patient has the following hepatitis profile: anti-HAV IgM = not detected; HBsAg = detected; anti-HBc IgM = detected; anti-HBc total = detected; anti-HBs = not detected; anti-HCV = not detected. What is his diagnosis? A) acute hepatitis A B) acute hepatitis B C) acute hepatitis C D) chronic hepatitis B E) immune to hepatitis B 51) In the routine diagnosis of rubella virus, which type of laboratory test should be ordered first? A) antigen detection B) antibody detection C) viral culture 52) Serology is performed on a patient with a rash and fever with the following results: rubella IgM = positive; rubella IgG = positive; measles IgM = negative; measles IgG = positive; varicella-zoster IgM = negative; varicella-zoster IgG = negative. What is the interpretation of these results? A) acute infection with rubella virus B) acute infection with measles virus C) not immune to measles or rubella viruses D) immune to varicella-zoster virus only 53) A physician wants to know if his patient who currently has a rash and fever has an active varicella-zoster virus infection. IgG against varicella-zoster virus was detected. IgM against varicella-zoster virus was not detected. What do these results mean for the patient? A) The patient has a current varicella-zoster virus infection. B) The patient has never had varicella-zoster virus. C) The patient has had varicella-zoster virus in the past, but does not have it now. D A B B A C 8 Immuno TB Flashcards Unit 4 54) A 14-year-old boy presents to the physician complaining of sore throat, fatigue, and fever for the last week. A monotest was performed and was reported as positive. This boy has: A) infectious mononucleosis B) streptococcal pharyngitis C) acute glomerulonephritis D) common cold 55) The causative agent of infectious mononucleosis is A) Streptococcus pyogenes B) Staphylococcus aureus C) Epstein-Barr virus D) HIV 56) A patient presents to the physician complaining of a 4-week history of fever, malaise, and irritability. The patient admits to feeling better as compared to how he felt even a week ago. The physician thinks that the patient might have had cytomegalovirus (CMV). Which of the following sets of serologic results would you see in this patient if he is recovering from CMV? A) CMV IgM pos; CMV IgG neg B) CMV IgM neg; CMV IgG pos C) CMV IgM neg; CMV IgG neg 57) A patient has an antibody profile for Epstein-Barr virus performed with the following results: EBVCA IgM = pos; EBVCA IgG = pos; EBV-NA = neg; EBV-EA = neg. This patient has which of the following? A) acute EBV infection B) convalescent EBV C) past exposure to EBV D) lack of EBV infection 58) A patient with infectious mononucleosis would have what outstanding feature in the hematology evaluation? A) decreased total white blood cells B) presence of atypical lymphocytes C) increased percentage of eosinophils D) absence of neutrophils 59) A patient has the following EBV antibody profile: EBVCA IgM = neg; EBVCA IgG = pos; EBV-EA IgG = pos; EBV-NA IgG = pos. Which of the following is the correct interpretation of these data? A) never infected with EBV B) acute infection with EBV C) recent convalescence from EBV D) long-ago past infection with EBV A C B A B D 9 Immuno TB Flashcards Unit 4 60) A physician suspects that his patient has infectious mononucleosis. Heterophile antibody tests are negative. Serological testing for Epstein-Barr virus was performed with the following results obtained: EBV VCA IgM = neg; EBV VCA IgG = neg; EBV-EA = neg; EBV-NA = neg. What is this person's status with regards to EBV? A) acute EBV B) convalescent EBV C) never infected with EBV D) past exposure to EBV 61) A 17-year-old female with suspected mononucleosis tested negative for heterophile antibody using the slide agglutination monotest. Her serum was sent to a reference lab, and the following results were obtained: negative for anti-VCA, positive for EA. What do these results suggest? A) She does not have mononucleosis. B) She is a healthy carrier of the virus. C) Mononucleosis has been reactivated. D) She is in the early stages of the disease. 62) All of the following are characteristic of the Epstein Barr virus EXCEPT: A) latent virus B) DNA virus C) cause of infectious mono D) invades T cells 63) In the slide test for infectious mononucleosis, what purpose do the guinea pig kidney cells serve? A) absorb out mono antibody B) absorb out Forssman antibody C) enhance the agglutination reaction D) serve as a positive control 64) The Paul Bunnell test for mononucleosis would detect which of the following? A) heterophile antibody for mononucleosis B) Forssman antibody C) serum sickness antibody D) any of the above 65) A positive rubella titer in a healthy, nonpregnant 22-year-old female most likely indicates which of the following? A) immunity after administration of the vaccine B) current presence of the disease C) no immunity D) possibility of congenital rubella 66) In a slide agglutination test for mononucleosis using guinea pig kidney and horse red blood cells, if there is no agglutination when the horse red cells are added, what conclusion can be drawn? A) It is positive for mononucleosis. B) It is negative for mononucleosis. C) It is positive for Forssman antibody. D) It indicates RF antibody. C D D B C A B 10 Immuno TB Flashcards Unit 4 67) A patient has serum tested for HIV antibodies by ELISA, and the test is positive. The patient's serum is retested in duplicate with two more positive results. What should be done next? A) Patient is diagnosed with acute HIV infection. B) Serum is tested for antibodies against hepatitis C virus. C) HIV Western blot assay is performed on patient's serum. D) Results mean that patient had HIV in the past but not now. 68) A 25-year-old male presents to the public health clinic complaining of flu-like symptoms. The man has been an IV drug user and prostitute for the last 5 years. HIV antibody screening is positive. Subsequently, antibodies are found to have specificity for p24, gp120, p31, and gp41. This patient has: A) current HIV infection B) indeterminate HIV infection C) lack of HIV infection D) infection with some other virus 69) Which is most likely a positive Western blot result for infection with HIV? A) band at p24 B) band at gp60 C) bands at p24 and p31 D) bands at p24 and gp120 70) The HIV p24 protein encodes: A) group-specific antigen (GAG) B) the receptor for host cells (ENV) C) reverse transcriptase (POL) D) none of these 71) Which technique is most widely used for the confirmation of a positive serologic assay for antibodies against HIV? A) enzyme-linked immunosorbent assay (ELISA) B) complement fixation C) Western blot assay D) polymerase chain reaction 72) Which of the following HIV-encoded proteins/glycoproteins is the receptor for host cells? A) p24 B) gp120 C) gp41 D) p31 73) The Western blot test used to confirm HIV is an example of which of the following? A) immunofixation B) immunoelectrophoresis C) double diffusion D) passive agglutination C A D A C B A 11 Immuno TB Flashcards Unit 4 74) All of the following body fluids are considered to be possible routes of transmission for HIV even if there is no visible sign of blood EXCEPT: A) spinal fluid B) semen C) urine D) vaginal secretions 75) Which test would be most reliable in detecting HIV infection in an infant younger than 18 months of age? A) ELISA test for antibody B) testing for p24 antigen C) Western blot D) DNA PCR testing 76) A 22-year-old male sees his physician for an annual checkup. He reported having flu-like symptoms including fever, sore throat, and lymphadenopathy several months ago. He has lost about 10 pounds but otherwise feels fine. Since he reports that a former girlfriend told him she is HIV positive, the physician recommends testing. An ELISA test is positive, a Western blot is positive, and a CD4+ T-cell count is 500/L. What do these results indicate? A) He has AIDS. B) He has recovered from HIV infection. C) He is HIV positive but in a latent stage. D) He has an opportunistic infection and not HIV. 77) What is different about the replication cycle of HIV that separates it from many other RNA viruses? A) Viral RNA is used to make cDNA. B) Viral RNA replicates itself directly to make new RNA. C) The virus reproduces only in B cells. D) Proviral DNA makes new viral particles immediately. 78) All of the following conditions would indicate AIDS EXCEPT: A) a CD4+ count of less than 200 cells/L B) Kaposi's sarcoma C) esophageal candidiasis D) infectious mononucleosis 79) What is the main mechanism of action of nucleoside analogue drugs such as zidovudine? A) inhibiting the action of reverse transcriptase B) blocking entry of HIV into host cells C) acting as protease inhibitors D) preventing release of HIV particles 80) Viral load testing is of most clinical utility in all of the following situations EXCEPT: A) initial diagnosis of HIV infection when antibody tests are positive B) monitoring patients during antiretroviral therapy C) setting a baseline before antiretroviral therapy has begun D) investigating a patient's sudden drop in T-cell count C D C A D A A 12