eprint_4_14329_473
advertisement

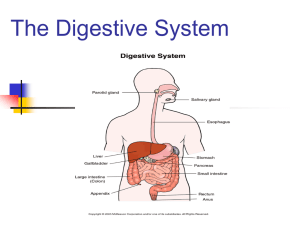
GIT physiology المرحلة الثانية المحاضرة الخامسة Gastric digestion and absorption: Carbohydrate digestion in the stomach depend on the action of salivary amylase, which remains active until by low pH in the stomach. Protein digestion occur in the stomach by about 10% and mediated by HCL and gastric pepsin. Fat digestion is minimal in the stomach due to restriction of gastric lipase activity. Very little absorption of nutrients take place in stomach. The stomach is a poor absorptive area of the gastrointestinal tract because it lacks the typical villus type of absorptive membrane, and also because the tight junctions between the epithelial cells. Only a few highly lipid-soluble substances, such as alcohol and some drugs like aspirin, As well as( non-ionized triglycerides of acetic. propionic and butyric acid can be absorbed in small quantities.), Aspirin at gastric pH is non-ionized and fat soluble, after absorption, it ionizes intracellular. damaging mucosal cells. Ethanol is rapidly absorbed in proportion to its concentrationof water. water moves in both direction across mucous, Water-soluble substances including Na+ , K-. glucose and amino acid are very poorly absorbed. Vomiting (emesis): Vomiting is an example of central regulation of gut motility function. The sensory signals that initiate vomiting originate mainly from the pharynx, esophagus, stomach, and upper portions of the small intestines. It is a forceful expulsion of contents of stomach and upper intestinal tract through mouth. It is reflex coordinated by brain stem, medulla known( vomiting center) which found in the reticular formation of the medulla, or by activation of chemoreceptor trigger zone within brain stem. increased pressure within skull, rotating movement of head, intense pain, tactile stimuli applied to back of the throat and excessive distention or irritation of the duodenum provides strong stimulus for vomiting when the vomiting center is directly activated. In the early stages antiperistalsis begins to occur often many minutes before vomiting appears. Antiperistalsis means peristalsis up the digestive tract rather than down ward antiperistaltic wave travels backward up the intestine at a rate of 2 to 3 cm/sec; this process can actually push a large share of the lower small intestine contents all the way back to the duodenum and stomach within 3 to 5 minutes. when the vomiting center is directly activated, it causes projectile vomiting not accompanied by nausea while stimulation of chemoreceptor trigger-zone is accompanied by nausea. Importance of vomiting with nausea is to remove the ingested toxic substances before they can be absorbed. Nausea importance to avoid ingestion of food containing the same toxic substances. Vomiting is preceded by increase salivation, sweating, increased HR, pallor and feeling of nausea. all characteristic of discharge of sympathetic nervous system. Vomiting begin deep inspiration, closure of glottis, elevation of soft palate, abdominal and thoracic muscles contract. Upper small intestine contract lower esophageal sphincter relax. Event occur repeatedly without vomiting is known retching. 3- Small intestine The intestinal walls are made up of smooth muscle that contract and relax moving the food or chyme forward then slightly backward. This gives the intestine additional time for absorption. It is major site of digestion and absorption of carbohydrates, proteins, and fat on GIT. The small intestine has three parts: the duodenum, the jejunum, and the ileum It is 5 m long, it has an absorption area of over 250 m2 . The entire mucosal surface is lined by microvilli, protrude from the surface of intestinal cells, give intestinal mucous its characteristics brush border appearance .The villi contain capillary and lymphatic which transmit the absorbed substance into the portal circulation. villus. A, Longitudinal section B, Cross section showing a basement membrane beneath the epithelial cells and a brush border at the other ends of these cells. movement of the small intestine: The smooth muscles of small intestine is myogenic property(spontaneous contraction ) serves two major functions: 1- Mixing the chyme with digestive juices and bile to facilitate digestion and absorption. 2- Propelling the chyme from the duodenum to the colon. Types of movements: A- Segmentation(mixing contraction): It is most common type of intestinal contraction. in which the Chyme cause distention of intestine wall lead to streach reflex and this cause concentric contraction of 1cm interval then few seconds later the contraction of the previous segment will disappear and another one will occur at the mid portion of relaxed segment, forcing the chyme back toward the stomach and toward the colon. when muscle relaxes, the chyme return to the area from which it is displaced, it is occur in more frequency in duodenum than the ileum. The segmentation contraction are weak when enteric plexus is blocked by atropine. Segmentation movements of the small intestine B- Peristalsis ( Propulsive movement) Chyme is propelled through the small intestine by peristaltic waves occur in any part of the small intestine, and they move toward the anus. Contraction of small section of proximal muscles is followed by relaxation of muscles just distal to it. Resulting wave like motion moves food along the GIT from proximal to distal direction as well spread out the chyme along the intestinal mucosa. movement of the chyme is very slow only 1 cm/min. This means that 3 to 5 hours are required for passage of chyme from the pylorus to the ileocecal valve. It is greatly increased after meal.This is caused by enter of the chyme into duodenum by gastroenteric reflex. In sever infection diarrhea can cause powerful and rapid peristalsis called peristaltic rush. This is initiated by vagovagul nervous reflex to brain stem and back to GIT. C- Migrating motor complex contractions During fasting between periods of digestion, the pattern of electrical and motor activity in gastrointestinal smooth muscle becomes modified so that cycles of motor activity migrate from the stomach to the distal ileum. These cycle called migrating motor complex (MMC). Gastric secretion, bile flow, and pancreatic secretion increase during each MMC. They are immediately stopped by ingestion of food . It is peristaltic wave that remove food left in stomach and intestine. They likely serve to clear the stomach and small intestine of luminal contents in preparation for the next meal. It begin within esophagus and travel through entire GIT and occur even 60-90 minutes. The hormone motilin which is released from the epithelium of small intestine increase the strength of contraction MMC ,(migrating motor complex) is a set of strong contractions that lasts a few minutes in one section of the digestive tract, then moves aborally. Their roles 1) flush remaining food and bacteria into the large intestine 2)tell you that you’re hungry. Intestinal secretion: 1- Mucus: Serves as a protective role, preventing HCL and chyme from damaging the intestinal wall. Mucus is secreted by Brunner's glands which are located within duodenum, and by goblet cells which are located along the length of intestinal epithelium. It is secreted in response to tactile or irritating stimuli, to vagal stimulation, and to GIT hormones secretion, Brunner's glands. Inhibited by sympathetic stimulation which may lead to peptic ulceration. 2- Enzymes: Epithelial cell of the mucosa covering the villi contain digestive enzymes .They capable of breaking down a small peptide by peptidase to amino acids ,disaccharide to monosaccharides by sucrase ,maltase and lactase and lipase for fats into glycerol and fatty acids .They are not secreted into intestine, they able to digest them during absorptive process. 3- Water and electrolytes: They are secreted by all the epithelial cells of the intestine. The water secretion provides a solvent into which the products of digestion are dissolved. Function of the ileocecal valve: A principal function of the ileocecal valve is to prevent back flow of fecal contents from the colon into the small intestine. the ileocecal valve itself protrudes into the lumen of the cecum and therefore is forcefully closed when excess pressure builds up in the cecum and tries to push cecal contents backward against the valve lips. The valve usually can resist reverse pressure of at least 50 to 60 centimeters of water. The wall of the ileum for several centimeters from the ileocecal valve has a thickened circular muscle called the ileocecal sphincter. This sphincter normally remains mildly constricted and slows emptying of ileal contents into the cecum. after a meal, a gastroileal reflex intensifies peristalsis in the ileum, and emptying of ileal contents into the cecum .Resistance to emptying at the ileocecal valve prolongs the stay of chyme in the ileum and thereby facilitates absorption. Normally, only 1500 to 2000 milliliters of chyme empty into the cecum each day. Emptying at the ileocecal valve