Top ten quality standards for spondyloarthritis
advertisement
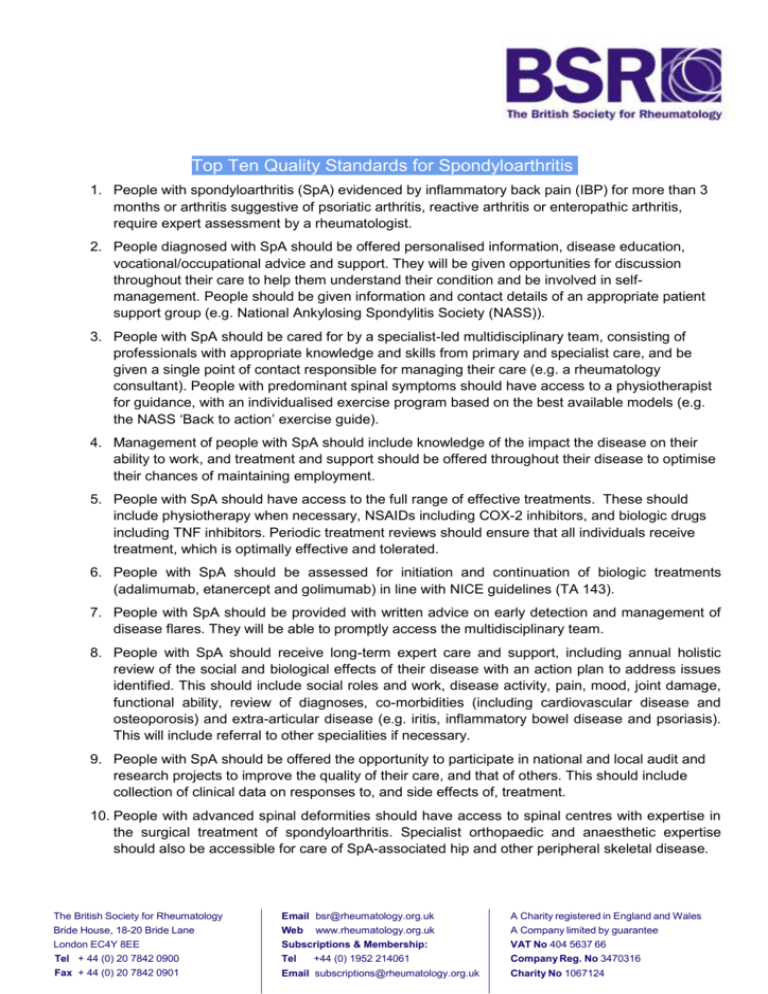
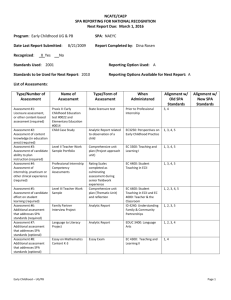
Top Ten Quality Standards for Spondyloarthritis 1. People with spondyloarthritis (SpA) evidenced by inflammatory back pain (IBP) for more than 3 months or arthritis suggestive of psoriatic arthritis, reactive arthritis or enteropathic arthritis, require expert assessment by a rheumatologist. 2. People diagnosed with SpA should be offered personalised information, disease education, vocational/occupational advice and support. They will be given opportunities for discussion throughout their care to help them understand their condition and be involved in selfmanagement. People should be given information and contact details of an appropriate patient support group (e.g. National Ankylosing Spondylitis Society (NASS)). 3. People with SpA should be cared for by a specialist-led multidisciplinary team, consisting of professionals with appropriate knowledge and skills from primary and specialist care, and be given a single point of contact responsible for managing their care (e.g. a rheumatology consultant). People with predominant spinal symptoms should have access to a physiotherapist for guidance, with an individualised exercise program based on the best available models (e.g. the NASS ‘Back to action’ exercise guide). 4. Management of people with SpA should include knowledge of the impact the disease on their ability to work, and treatment and support should be offered throughout their disease to optimise their chances of maintaining employment. 5. People with SpA should have access to the full range of effective treatments. These should include physiotherapy when necessary, NSAIDs including COX-2 inhibitors, and biologic drugs including TNF inhibitors. Periodic treatment reviews should ensure that all individuals receive treatment, which is optimally effective and tolerated. 6. People with SpA should be assessed for initiation and continuation of biologic treatments (adalimumab, etanercept and golimumab) in line with NICE guidelines (TA 143). 7. People with SpA should be provided with written advice on early detection and management of disease flares. They will be able to promptly access the multidisciplinary team. 8. People with SpA should receive long-term expert care and support, including annual holistic review of the social and biological effects of their disease with an action plan to address issues identified. This should include social roles and work, disease activity, pain, mood, joint damage, functional ability, review of diagnoses, co-morbidities (including cardiovascular disease and osteoporosis) and extra-articular disease (e.g. iritis, inflammatory bowel disease and psoriasis). This will include referral to other specialities if necessary. 9. People with SpA should be offered the opportunity to participate in national and local audit and research projects to improve the quality of their care, and that of others. This should include collection of clinical data on responses to, and side effects of, treatment. 10. People with advanced spinal deformities should have access to spinal centres with expertise in the surgical treatment of spondyloarthritis. Specialist orthopaedic and anaesthetic expertise should also be accessible for care of SpA-associated hip and other peripheral skeletal disease. The British Society for Rheumatology Bride House, 18-20 Bride Lane London EC4Y 8EE Tel + 44 (0) 20 7842 0900 Fax + 44 (0) 20 7842 0901 Email bsr@rheumatology.org.uk Web www.rheumatology.org.uk Subscriptions & Membership: Tel +44 (0) 1952 214061 A Charity registered in England and Wales A Company limited by guarantee VAT No 404 5637 66 Company Reg. No 3470316 Email subscriptions@rheumatology.org.uk Charity No 1067124