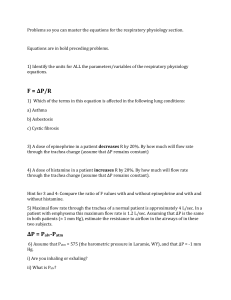
8. Respiratory Worksheet
advertisement
RESPIRATORY SYSTEM WORK SHEET List four key functions of the respiratory system. What is lost from the body through the respiratory system besides carbon dioxide? Distinguish between inspiration and expiration. Name the structures of the upper and lower respiratory system. upper: lower: The Airways of the Conducting System Connect the Lungs with the Environment As gas moves into the airways, the diameter of the airways gets progressively smaller, and the total crosssectional surface area of the airways (increases/decreases?) (Fig. 17-4). The velocity of air flow is highest in the ____________ and lowest in ____________. The Alveoli Are the Site of Gas Exchange Briefly describe and give the functions of the three types of cells in the alveoli. 1) 2) 3) Air is a Mixture of Gases How do you calculate the partial pressure of one gas in a mixture of gases? What happens to the partial pressures of individual gases if dry air is suddenly humidified? Gases Move from Areas of Higher Pressure to Areas of Lower Pressure Air flows from regions _______________________ of to regions of _______________________. What must be present for individual gases to move from one region to another? What role does muscle contraction play in the creation of air flow in the respiratory system? 2 Pressure - Volume Relationships of Gases are Described by Boyle's Law For gases in a closed container, as volume (increases/decreases?), pressure (increases/decreases?). How does the respiratory system create changes in volume? Solubility of Gas in Liquid Depends on the Pressure and Solubility of the Gas and Temperature When a gas is in contact with a liquid, what 3 factors determine how much gas will dissolve in the liquid? 1) 2) 3) If a liquid is exposed to a PCO2 of 100 mm Hg and a PO2 of 100 mm Hg, equal amounts of oxygen and carbon dioxide will dissolve in the liquid. True or false? _________. The more soluble a gas is, the (greater/less?) the partial pressure needed to force the gas into solution. Gases move between liquid and gaseous phases until ______________is reached. Which gas is more soluble in body fluids: O2 or CO2? __________. Inspiration occurs when Intrapulmonary Pressure Decreases What division of the nervous system controls the muscles of ventilation? What neurotransmitter and receptor does this division use? During inspiration, the diaphragm contracts and moves in which direction? _______________________. Expiration occurs when Intrapulmonary Pressure Exceeds Atmospheric Pressure Tick which of these muscles are contracting in passive expiration: External intercostal muscles __, Internal intercostal muscles __ , Diaphragm __, Abdominal muscles __ Tick which of these muscles are contracting in active expiration: External intercostal muscles __, Internal intercostal muscles __, Diaphragm __, Abdominal muscles __, Intrapleural Pressure Changes during Ventilation Explain why the intrapleural pressure is always subatmospheric. (Fig. l7-l0a) Explain why puncturing the pleural membrane (pneumothorax) causes the lung to collapse. (Fig. 17-10 b) Lung Compliance and Elastance may Change in Disease States Define compliance Which is true? A high-compliance lung a) requires additional force to stretch it or; b) is easily stretched? What is elastance? A high compliance lung always has high elastance. True or false? Explain. What happens to compliance and elastance in the disease state of emphysema? 3 Surfactant Decreases the Work of Breathing What creates resistance to stretch in the lung? ______________________________________________. What is the function of surfactant? ________________________________________________________. According to the Law of LaPlace, if two alveoli have equal surface tension, the (larger/smaller?) will have a higher internal pressure. (Fig. 17-11) Which will have a higher concentration of surfactant, a large alveolus or a small one? Explain why. What happens in premature babies who have not produced surfactant (see page 561)? Resistance of the Airways to Air Flow is determined primarily by Airway Diameter Use a familiar formula (p560) to explain the relationship between resistance to air flow, length of airways (L), viscosity of air (n) and radius of airways (r) (Table 17-3). Which factor is most significant? What part of the respiratory system is the site of variable resistance? _____________________________. If the bronchioles constrict, what happens to resistance ________ and air flow_________ into the alveoli? How do each of the following affect bronchiole diameter (bronchodilation or bronchoconstriction?) 1) CO2 _________________ 2) Histamine _________________ 3) Epinephrine ___________________. 4) Parasympathetic neurons ______________. 5) Name the receptors for 3) __________________ and neurotransmitters for 4)___________________? Effectiveness of Ventilation is determined by the rate and depth of breathing Define total pulmonary ventilation in words and give the mathematical expression for it. Give normal average values for breathing rate and tidal volume in an adult male. Using the values above, what is an average value for total pulmonary ventilation? (Give units!) Define anatomic dead space. (page 564 and Fig. 17-14) How is alveolar ventilation different from total pulmonary ventilation? Which is it more accurate? 4 GAS EXCHANGE IN THE LUNGS By what mechanism do gases move between the alveoli and the plasma? __________________________. State the four rules for diffusion of gases (see p 575). 1. 2. 3. 4. Gas composition in the Alveoli varies little during normal breathing What are the PO2 and PCO2 of the atmosphere and the alveoli during normal breathing? PO2 atmosphere _______________. PO2 alveoli ________________. PCO2 atmosphere_______________. PCO2 alveoli _______________. The Partial Pressure Gradient is the Primary Factor Influencing Gas Exchange Give the following partial pressures in a normal person at sea level: (Fig 18-3 and Table 18-1) PO2: Alveoli = ______ Arterial blood = ______ Resting cells = ______Venous blood = ______ PCO2: Alveoli = ______ Arterial blood = ______ Resting cells = ______ Venous blood = ______ Gas Exchange can be affected by changes in the Alveolar membrane What 2 cell layers must gases cross to go from the alveoli to the plasma? 1) _______________________ and 2) __________________________. Explain how emphysema can result in a loss of alveolar surface area. Explain how fibrotic lung diseases can cause decreased oxygen exchange between alveoli and the blood. What is pulmonary edema and how does it alter gas exchange? Hemoglobin Transports Most Oxygen to the Tissues Total blood oxygen content = _______________________ + ________________________. (see p 580). If PO2 is 100 mmHg, then only ____ mL of O2 will dissolve in plasma of 1 L of blood, but ____mL will be carried bound to Hb. Therefore, the total O2 carrying capacity of blood is ____ mL/L blood. 5 Each Hemoglobin molecule binds up to four (4) Oxygen (O2) molecules How many protein subunits are composed Hb molecules of? ___. This group is based around the ______ element that binds weakly to oxygen. Hb bound to O2 is called _______________________. As dissolved O2 diffuses into RBCs, what happens to the PO2 of the surrounding plasma? ____________. Therefore, when O2 binds with Hb, (more/less?) O2 can diffuse from the alveoli into plasma. The amount of O2 bound to Hb at any given PO2 is termed the “__________ ___________ of hemoglobin”. At 100% saturation, all possible binding sites are (bound/free?). ______________. At the cells, dissolved O2 in the plasma (enters/leaves?) ________ the cells. This disturbs the ___________________ so O2 dissociates from hemoglobin, obeying the Law of ____________________. When equilibrium is restored, the PO2 of the plasma reflects the PO2 of the _________________________. The Oxygen-Hemoglobin Dissociation Curve Shows the Relationship between PO2 and Hemoglobin Binding of Oxygen In the oxygen-hemoglobin dissociation curve (Fig. 18-8 and 9), the (PO2/percent saturation of Hb) determines the (PO2/percent saturation of Hb). Hemoglobin-Oxygen Saturation Curve 100 90 80 70 % 60 Hb-O2 Saturation 50 40 30 20 10 0 0 10 20 30 40 50 60 70 80 90 100 PO2 (mm Hg) Below PO2 of 60 mmHg, where the curve is steeper, small changes in PO2 cause relatively (small/large?) releases of O2 from hemoglobin. Temperature, pH, and Metabolites Affect Oxygen-Hemoglobin Binding. Complete the following: An increase in pH (increases/decreases?) hemoglobin's affinity for oxygen. An increase in temperature (increases/decreases?) hemoglobin's affinity for oxygen. An increase in PCO2 (increases/decreases?) hemoglobin's affinity for oxygen. The metabolite 2,3-Diphosphoglycerate (DPG) (increases/decreases?) hemoglobin's affinity for oxygen. A left shift in the curve indicates (increased/decreased?) binding affinity. A right shift in the curve indicates (increased/decreased?) binding affinity. 6 Changes in pH causing a right shift in the Hb-dissociation curve is also known as the ___________ effect. Under what conditions is the cellular production of 2,3-DPG increased? _________________________. Transport of CO2: Dissolved in Plasma, Bound to Hemoglobin, and as Bicarbonate Ions Explain the three ways that CO2 is transported in the blood. (Fig. 18-13, p 584-586) 1) 2) 3) The name for hemoglobin bound to CO2 is _________________________. Write the equation for the bicarbonate buffer. What enzyme catalyzes this reaction? REGULATION OF VENTILATION Respiratory Neurons in the Medulla Control Inspiration and Expiration (p587) Compare the functions of the dorsal and ventral respiratory groups of neurons in the medulla. (Fig. 18-15) Carbon Dioxide, Oxygen, and pH Influence Ventilation List three chemical factors that affect ventilation. Where are the sensory receptors located for each? 1) 2) 3) Peripheral Chemoreceptors - the carotid and aortic bodies Explain the strategic significance of the location of the peripheral chemoreceptors. To what chemical signals (and limited ranges) do the carotid and aortic bodies respond? Central Chemoreceptors How do central chemoreceptors respond to elevated blood Pco2? Central receptors in the medulla mediate ventilation changes in response to ___________. A decrease in Pco2 will trigger a/an (decrease/increase?) in ventilation. A decrease in pH will trigger a/an (decrease/increase?) in ventilation. A decrease in arterial Po2 below mm Hg will trigger a/an (decrease/increase?) An increase in Pco2 will cause a/an (decrease/increase?) in pH, which in turn will trigger a/an (2,3-acidosis (decrease/increase?) in ventilation. What is the primary chemical stimulus for changes in ventilation? ____________. The Hering-Breuer inflation reflex is designed to ___________________________________________. If tidal volume exceeds __________, then ___________ receptors in the lung will signal the brain stem to ______________ inspiration.