Ch5_Resp
advertisement
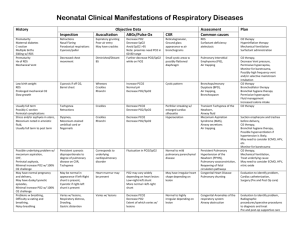
Ch. 5 Ventilation – Perfusion Relationships Review V/Q mismatch animation Oxygen Transport from Air to Tissues P ATM = 760 mm Hg PH20 = 47 mm Hg Pnormal air ~-> 713 mm Hg (760-47) FIO2 (fraction of inspired oxygen) = .21 or 21% PIO2 = 150 mm Hg Since flow is dependent on the change in pressure the inspired oxygen pressure must be significantly higher than the pressure in the alveoli Mouth PO2 = 150 mm Hg PAO2 = 100 mm Hg (pressure of alveolar oxygen) PtissuesO2 = ~ 40 mm Hg (i.e. pressure of venous blood (( remember RBC’s are still ¾ saturated w/ O2 upon return to the pulmonary cap’s)) What determines pressure gradient? o Removal of O2 by pulmonary capillary blood Largely determined by O2 consumption in tissues Once rbc reaches tissue, O2 leaves rbc d/t very low pressure in mitochondria (1 mm Hg) o Continual replenishment by alveolar ventilation (continued inspiratory flow) Primary determinant of PO2 o Fluctuation of PO2 b/t inspi and expi is only 3 mm Hg, i.e. after expi – PAO2 = 97 mm Hg o Any decrease in PO2 results in lower PtissueO2 (also why impaired gas exchange results in rise of PCO2) Four Causes of Hypoxemia o Hypoventilation o Diffusion limitation o Shunt o Ventilation – Perfusion inequality Hypoventilation If the alveolar ventilation is abnormally low, the alveolar PO2 falls and PCO2 rises Causes of hypoventilation: o Drugs – i.e. morphine, barbiturates – depress medulla lower inspiratory drive o Trauma to chest wall (rib fx) o High resitance to breathing (i.e. asthma attack constriction of conducting airways) o PCO2 = (VentilationCO2 / Ventilation alveolar) x K o This means if you decrease alveolar ventilation by ½: PCO2 is doubled Thus, PCO2 is inversely proportional to VAO2 (Ch. 2) Alveolar Gas Equation o PAO2 = PIO2 – (PACO2/R) o R = 0.8 for most U.S. diets, appx. O.7 for high fat diet (dependent on CO2 production via glycolytic pathway) o PACO2 is normally determined by ABG o Thus: o PIO2 = FIO2 x (PATM – PH2O) o PAO2= .21x(713mmHg) - (PACO2 / 0.8) Thus during Hypoventilation – a reduction of PAO2 and PaO2 occurs o Except if person is given oxygen through mask Hypoventilation o Always increases the PCO2 o Decreases the PO2 unless additional O2 is inspired o Hypoxemia is easy to reverse by adding O2 Hyperventilation o Drives down PaCO2 o Large reserves of CO2 in body via H2CO3 – so takes a longer time for blood PO2/CO2 ratio to balance Diffusion With 100 PAO2 mm Hg and 100 PaO2 mm Hg – (ideal conditions) o Blood passes alveoli with oxygen content of 18.73 mL O2/dL blood o Little difference occurs as long as ratio of ventilation/perfusion is proportional i.e. 1/1 5/5 Shunt Means that blood that enters the arterial system essentially bypasses the lungs o Natural shunts: Thebesian veins, pulmonary veins, pulmonary arterio-venous fistula, or atrial septal defect Depresses the arterial PO2 Total amt. of O2 leaving the system is the total flow (Q(dot)T) times the concentration of arterial blood (Cao2)—(normal CaO2 ~ 18.73 ml/dL of blood) QT x CaO2 – must be equal to the sum of the amts. Of O2 in the shunted blood o O2 in shunted blood = Q(dot)S x CV(line)O2; and end-capillary blood (Q(dot)T – Q(dot)S x Cc’O2 o QS/QT = Cc’O2 – CaO2 / CC’O2 – CVlineO2 o Total blood flow (normally 5L/min) x O2 concentration in arterial blood (normally 18.73 ml/dL) = sum of amounts of O2 in shunted blood and end capillary blood o o Hypoxemia cannot be abolished by giving pt 100% O2 to breathe b/c shunted blood bypasses ventilated alveoli some O2 added to capillary blood by diffusion, but only to plasma – Hb is usually saturated (except if cause CO poisoning, sickle cell etc) Could worsen hypoxia b/c increasing the alveolar pressure excessively could further compress capillaries causing a negative PTM I.E. to diagnose if shunt is present in hypoxic pt: Take ABG, treat w/ 100% O2, wait 10 minutes; if PO2 is increased hypoxia is not d/t shunt, if PO2 is unchanged—shunt is present Shunts do not normally cause an increase in PaCO2 Chemoreceptors sense the elevated PaCO2 – hyperventilation to drive down CO2 Shunt o Hypoxemia responds poorly to added inspired O2 (only w/ shunt according to Schwarzstein) o When 100% O2 is inspired, the PaO2 does not rise to the expected level – Dx. Test o If the shunt is caused by mixed venous blood, its size can be calculated from the shunt equation --- (umm sure…) o http://www.medicalexplorer.org/resp_phys1/index.php?ch=5&fig=8B Ventilation – Perfusion Ratio Need balanced flow of pulmonary arterial blood to amt of O2 in alveoli to perfuse If one increases blood flow too much – Hb is not 100% saturated and hypoxia results Alternatively if pressure in Alveoli is too high and blood flow slows – Hb is highly saturated (i.e. 19.11 ml/dL) – usually not a problem unless alveolar pressure causes collapse of capillary (i.e. PA >> Pa>Pc) Effect of altering the ventilation – perfusion Ratio of a lung unit Mixed venous blood: o PCO2 = 40 mmHg – higher pressure of CO2 promotes its exchange across alveoli o PO2 = 100 mmHg Diseases such as pneumonia, heart failure, asthma, and emphysema can worsen V/Q mismatch Nonlinear shape of the oxygen dissociation curve creates a different situation for oxygen content when we mix blood from well ventilated and poorly ventilated alveoli (as occurs w/ V/Q mismatch) Low V/Q ratio produces a PO2 value that corresponds to the steep portion of the oxygen dissociation curve and thus significantly lowers the oxygen content of the outgoing capillary blood High V/Q ratio produces a PO2 value that corresponds to the relatively flat portion of the oxygen dissociation curve and thus does not significantly elevate the oxygen content of outgoing blood http://www.medicalexplorer.org/resp_phys1/index.php?ch=5&fig=8C&w=7 Using the link above, vary the V/Q ratios for three alveoli o Increase the V/Q ratio in one alveolus while decreasing the ratio of another and note hwo the small elevation in oxygen content caused by the high V/Q ratio alveolus does not compensate for the significant decrease in oxygen content caused by the low V/Q ratio alveolus Regional Gas Exchange in the Lung Apex of lung: o high V/Q ratio (hypodiffusion) – too little air in alveoli o PO2: 135 mm Hg o PCO2: 30 mm Hg o pH: 7.51 o Site of Tuberculosis: anaerobic Base of lung: o Low V/Q ratio ( hyperperfusion or wasted perfusion) – lil too much blood in caps o PO2: 90 mm Hg o PCO2: 42 mm Hg o pH: 7.39 Ventilation/Perfusion ratio decreases as one goes from apex to base See chart 5-10 (west) for more data on differences b/t apex and base Effect of Ventilation-Perfusion Inequality on overall gas exchange Lung w/ V/Q mismatch is not able to transfer as much O2 and CO2 as a lung that is uniformly ventilated and perfused Lung w/ V/Q inequality can’t maintain as high PaO2 or as low PaCO2 as regular lung Majority of blood leaving the lungs comes from base --- where PO2 is low depression of Pao2 Alveolar ventilation occurs more evenly from apex to base (but still mostly at base) Note from previous figure: a V/Q mismatch in one alveoli affect the output from the remaining alveoli near b/c output PaO2 is an avg. of cap’s and alveoli’s together (i.e. bomb the first exam, and it’s harder to improve avg.) CO2 has an easier time diffusing b/c it’s saturation curve is essentially linear Distribution of Ventilation-Perfusion Ratios Great – research oriented physiology stuff…. Shoot someone up full of mixed gases Although much of the gas goes to areas w/ equal V/Q ratios; some portion goes to V/Q mismatch areas o Poor V/Q ratios (0.3 to 0.003) This areas are poor at eliminating CO2 o Person had arterial hypoxemia but normal PCO2 (i.e. would be hyperventilating to keep CO2 normal wasted ventilation) Remember ideal V/Q = 1 Ventilation-Perfusion Inequality as a Cause of CO2 retention Note use of term “magical” in text…. With a V/Q mismatch both PO2 and PCO2 are affected Alveolar dead space: the volume of the alveoli that are not being perfused (about 20-50 ml in adults) V/Q ratio determines the gas exchange in any single lung unit Regional differences of V/Q in the upright human lung cause a pattern of regional gas exchange V/Q inequality impairs the uptake or elimination of all gases by the lung Although the elimination of CO is impaired by V/Q inequality, this can be corrected by increasing the ventilation of the alveoli By contrast, the hypoxemia resulting from V/Q inequality cannot be eliminated by increases in ventilation The different behavior of the 2 gases results from the different shapes of their dissociation curves A-aDO2: how you measure V/Q mismatch Subtract arterial PO2 from alveolar PO2 PAO2 – PaO2 = A-a DO2 Normal alveolar-arterial oxygen gradient (breathing room air) Age A-aDO2 1-30 <,= 10 40 <,= 12 50 <,= 15 70 <,= 25 Physiological Causes of Hypoxemia A-aDO2 Response to 100% O2 present at rest Decreased PIO2 (altitude) Normal yes yes Alveolar Hypoventilation Normal yes yes V/Q mismatch Increased Yes yes Shunt Increased NO yes Diffusion abnormality increased yes not usually, unless severe