Guide for pediatric floor intern:
advertisement
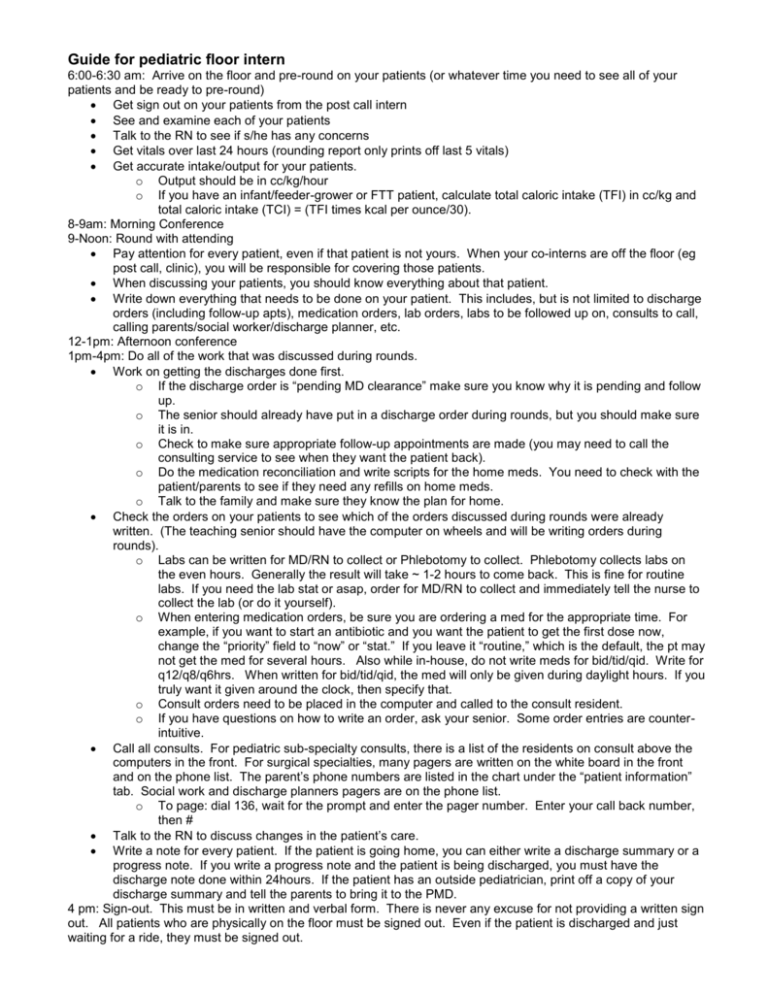
Guide for pediatric floor intern 6:00-6:30 am: Arrive on the floor and pre-round on your patients (or whatever time you need to see all of your patients and be ready to pre-round) Get sign out on your patients from the post call intern See and examine each of your patients Talk to the RN to see if s/he has any concerns Get vitals over last 24 hours (rounding report only prints off last 5 vitals) Get accurate intake/output for your patients. o Output should be in cc/kg/hour o If you have an infant/feeder-grower or FTT patient, calculate total caloric intake (TFI) in cc/kg and total caloric intake (TCI) = (TFI times kcal per ounce/30). 8-9am: Morning Conference 9-Noon: Round with attending Pay attention for every patient, even if that patient is not yours. When your co-interns are off the floor (eg post call, clinic), you will be responsible for covering those patients. When discussing your patients, you should know everything about that patient. Write down everything that needs to be done on your patient. This includes, but is not limited to discharge orders (including follow-up apts), medication orders, lab orders, labs to be followed up on, consults to call, calling parents/social worker/discharge planner, etc. 12-1pm: Afternoon conference 1pm-4pm: Do all of the work that was discussed during rounds. Work on getting the discharges done first. o If the discharge order is “pending MD clearance” make sure you know why it is pending and follow up. o The senior should already have put in a discharge order during rounds, but you should make sure it is in. o Check to make sure appropriate follow-up appointments are made (you may need to call the consulting service to see when they want the patient back). o Do the medication reconciliation and write scripts for the home meds. You need to check with the patient/parents to see if they need any refills on home meds. o Talk to the family and make sure they know the plan for home. Check the orders on your patients to see which of the orders discussed during rounds were already written. (The teaching senior should have the computer on wheels and will be writing orders during rounds). o Labs can be written for MD/RN to collect or Phlebotomy to collect. Phlebotomy collects labs on the even hours. Generally the result will take ~ 1-2 hours to come back. This is fine for routine labs. If you need the lab stat or asap, order for MD/RN to collect and immediately tell the nurse to collect the lab (or do it yourself). o When entering medication orders, be sure you are ordering a med for the appropriate time. For example, if you want to start an antibiotic and you want the patient to get the first dose now, change the “priority” field to “now” or “stat.” If you leave it “routine,” which is the default, the pt may not get the med for several hours. Also while in-house, do not write meds for bid/tid/qid. Write for q12/q8/q6hrs. When written for bid/tid/qid, the med will only be given during daylight hours. If you truly want it given around the clock, then specify that. o Consult orders need to be placed in the computer and called to the consult resident. o If you have questions on how to write an order, ask your senior. Some order entries are counterintuitive. Call all consults. For pediatric sub-specialty consults, there is a list of the residents on consult above the computers in the front. For surgical specialties, many pagers are written on the white board in the front and on the phone list. The parent’s phone numbers are listed in the chart under the “patient information” tab. Social work and discharge planners pagers are on the phone list. o To page: dial 136, wait for the prompt and enter the pager number. Enter your call back number, then # Talk to the RN to discuss changes in the patient’s care. Write a note for every patient. If the patient is going home, you can either write a discharge summary or a progress note. If you write a progress note and the patient is being discharged, you must have the discharge note done within 24hours. If the patient has an outside pediatrician, print off a copy of your discharge summary and tell the parents to bring it to the PMD. 4 pm: Sign-out. This must be in written and verbal form. There is never any excuse for not providing a written sign out. All patients who are physically on the floor must be signed out. Even if the patient is discharged and just waiting for a ride, they must be signed out.