- Sandhills Center
advertisement
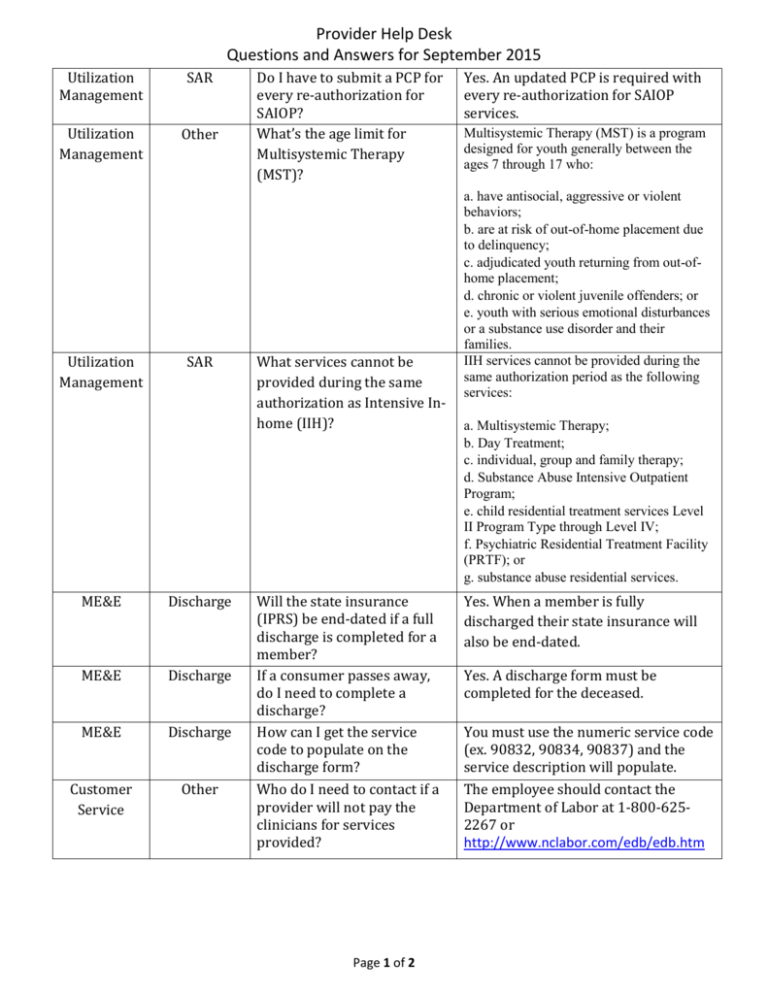
Provider Help Desk Questions and Answers for September 2015 Utilization Management SAR Utilization Management Other Utilization Management SAR ME&E Discharge ME&E Discharge ME&E Discharge Customer Service Other Do I have to submit a PCP for every re-authorization for SAIOP? What’s the age limit for Multisystemic Therapy (MST)? What services cannot be provided during the same authorization as Intensive Inhome (IIH)? Will the state insurance (IPRS) be end-dated if a full discharge is completed for a member? If a consumer passes away, do I need to complete a discharge? How can I get the service code to populate on the discharge form? Who do I need to contact if a provider will not pay the clinicians for services provided? Page 1 of 2 Yes. An updated PCP is required with every re-authorization for SAIOP services. Multisystemic Therapy (MST) is a program designed for youth generally between the ages 7 through 17 who: a. have antisocial, aggressive or violent behaviors; b. are at risk of out-of-home placement due to delinquency; c. adjudicated youth returning from out-ofhome placement; d. chronic or violent juvenile offenders; or e. youth with serious emotional disturbances or a substance use disorder and their families. IIH services cannot be provided during the same authorization period as the following services: a. Multisystemic Therapy; b. Day Treatment; c. individual, group and family therapy; d. Substance Abuse Intensive Outpatient Program; e. child residential treatment services Level II Program Type through Level IV; f. Psychiatric Residential Treatment Facility (PRTF); or g. substance abuse residential services. Yes. When a member is fully discharged their state insurance will also be end-dated. Yes. A discharge form must be completed for the deceased. You must use the numeric service code (ex. 90832, 90834, 90837) and the service description will populate. The employee should contact the Department of Labor at 1-800-6252267 or http://www.nclabor.com/edb/edb.htm Provider Help Desk Questions and Answers for September 2015 Network IT Credentialing How can a provider add a service to an existing contract? How can I get access to the Alpha AlphaMCS Portal? The Network is currently closed. SHC is not adding sites or services to existing contracts. Providers must complete the Alpha Provider Request Form. Contact the Provider Help Desk at 855-777-4652 or providerhelpdesk@sandhillscenter.org to receive the form. Quality Management Other How often is the Post Payment review completed? A Post Payment review is completed once every two years for all providers. Finance Billing Where can I access the checkwrite schedule? To access checkwrite schedule, go to www.sandhillscenter.org, click on For Providers, then choose Provider Forms. The checkwrite schedule will be located under the Finance, Billing and Claims category. Yes. Providers will receive a certified letter from the Network Director indicating the due date for submitting the re-credentialing applications. The assigned credentialing specialist will follow-up immediately after the letter is mailed. Network Credentialing Will providers receive a notice when it is time for recredentialing? Utilization Management SAR Can a SAR include more than one service code? ME&E Discharge Can providers print the discharge form in Alpha? ME&E Enrollment How can a provider complete an enrollment request for a member receiving Health Choice insurance? Page 2 of 2 Yes. After completing the initial service request, select the “Add Service” tab to add additional services to the SAR. No. The discharge form is unable to print in AlphaMCS. However, providers have the ability to view all the discharge forms completed by selecting “All Discharge” in the Discharge tab. Sandhills Center does not manage Health Choice. The provider can contact Value Options at 800-7533224 for assistance.