LABORATORY HEMATOLOGY
advertisement
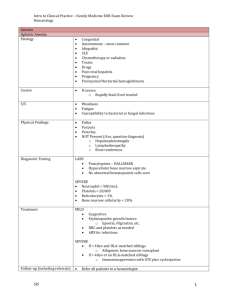
Laboratory Hematology 1 LABORATORY HEMATOLOGY Laboratory plays an indispensable role in the diagnosis and management of almost all hematologic disorders. The purpose here is to introduce you with the common laboratory tests and explain their significance. Some of the common tests in a hematology laboratory are the following but we will discuss only the first 4 tests. Other tests are discussed elsewhere Complete blood count with differential Reticulocyte count Peripheral blood smear evaluation Detection of fetal hemoglobin Serum and urine protein electrophoresis (SPEP & UPEP) Hemoglobin electrophoresis and/or HPLC for hemoglobin Cytochemistry Leukocyte immunophenotyping Coagulation tests COMPLETE BLOOD COUNT: This is the most common of all hematology tests. A standard CBC is referred to the following tests. Some parameters are actual measurements whereas others are just calculated by the analyzer based on other measured values 1. White blood cell (Leukocyte) count (WBC) with – measured 5-part differential count 5-part absolute count 2. Red blood cell (Erythrocyte) count – measured 3. Hemoglobin concentration – measured 4. Hematocrit percentage – measured or calculated 5. Mean cell volume (MCV) – calculated 6. Mean cell hemoglobin (MCH) – calculated 7. Mean cell hemoglobin concentration (MCHC) – calculated 8. Red cell distribution width (RDW) – calculated 9. Platelet count – measured 10. Mean platelet volume (MPV) – calculated An EDTA-anticoagulated blood is usually used for CBC determination. Although a 10 cc or a 5 cc blood collection tube is usually used, the amount of blood utilized for CBC is a very small fraction (<< 1 cc). Any abnormality “flagged” by automated counter triggers a manual review of the peripheral smear and cell counting. The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. Laboratory Hematology 2 AUTOMATED BLOOD ANALYSIS: Several automated hematology analyzers are available for this purpose. One of the most hematology analyzer is the one from Coulter called Coulter counter. Coulter method of cell counting and sizing is based on the detection and measurement of changes in the electrical resistance produced by cells suspended in a conductive liquid and traversing a small aperture. Suspended blood cells are “focused” into a single cell stream and passed through a small aperture with electrodes on either side. The cells act as discrete “nonconductors” or insulators of current as they pass from the electrode and through the aperture. The momentary drop or interruption of current produced by each cell is measured as a pulse. Cell count is proportional to the number of detected signals (or pulses) Cell size is proportional to the magnitude (amplitude) of each signal [This picture is adapted from BLOOD: Principles & Practice of Hematology by Handin et al. Lippincott Press] There are 2 channels of coulter counter. (a) No lytic agent / No shrinkage agent channel – Used for RBC and platelet evaluations (gives accurate RBC and platelet volumes) (b) RBC lytic agent / WBC shrinkage agent – Used for WBC evaluation and Hb measurement Each channel is analyzed by 3 distinct apertures for 4 seconds each. The total time for measurements and calculations is <1 minute. The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. Laboratory Hematology A typical CBC report from a normal count is shown below: The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. 3 Laboratory Hematology Some of the CBC reports from actual patients are shown below: NEUTROPHILIA, absolute and relative: EOSINOPHILIA, absolute and relative: The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. 4 Laboratory Hematology 5 LYMPHOCYTOSIS, absolute and relative: PANCYTOPENIA: White Blood Cell (WBC) evaluation: WBC count measured as number of cells >35 fl remaining in the “lysed” channel. Reported as cells x 109/L The 5-part differential and absolute count is made possible by two modalities (i) Conductivity – distinguishes among cells based on characteristics of the nucleus, granules, and chemical composition of the cells (ii) Light scattering – distinguishes among cells based on characteristics of the cell surface Data generated by all three interrogation modalities are used to generate a 3-D scatter plot to separate different WBCs. The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. Laboratory Hematology 6 Red Blood cell (RBC) evaluation: RBC count [M 4.5 – 5.5 x 1012/L, F 4 – 5 x 1012/L] is measured as number of cells with sizes >36 fl in the “unlysed” channel. WBC are also counted but these represent <0.1% of the cells counted. Reported as cells x 1012/L. RBC count is increased in polycythemia & decreased in decreased production by the marrow. Hemoglobin concentration [Males 13 – 18 g/dl, Females 12 – 16] is measured spectrophotometrically in the “lysed” channel. Reported as g/dl. Increased in polycythemia and decreased in anemia. Mean Cellular Volume (MCV) [80-100 fl] is determined from measured RBC size distribution (histogram) and is reflective of true RBC size. Reported in fl (Femto liter). Increased in macrocytosis such as seen in megaloblastic anemia and decreased in microcytic anemia such as iron deficiency anemia and thalassemia. Reticulocytes are also larger than mature RBCs and thus increased reticulocytes may “artifactually” increase the MCV. In patients with combined macrocytosis and microcytosis as seen in combined nutritional deficiencies of vitamin B12/folate and iron may in the end result in a falsely normal MCV. That is why examination of a peripheral blood smear is so important! Hematocrit [M 42% - 52%, F 37% - 48%] is calculated by coulter counter by a formula = RBC x MCV/10). Reported in %. It is increased in polycythemia and decreased in anemia. It is, however, directly affected by the plasma volume. In dehydrated states, Hct is increased whereas in volume overload is low. Mean cell hemoglobin (MCH) [28 – 33 pg/cell] is calculated by Hb/RBC x 10 and reported in pg (pico grams). It represents the amount of hemoglobin present in one red blood cell! It is decreased in hypochromia. Mean cell hemoglobin concentration (MCHC) [32 – 36 g/dl] is calculated by Hb/Hct x 100 and reported in g/dl. It represents the amount of Hb present in a “population” of red cells and takes into account any variation in the cell size and shape. A low MCHC reflects hypochromia. Red cell distribution width (RDW) [12% – 15%] is the coefficient of RBC size variation, which is calculated from the measured RBC size in histogram. It provides a quantitative expression of the size spread of the RBC populations (anisocytosis). Reported as %. It allows the presence of more than one cell size population to be appreciated quantitatively. The RDW is often used to provisionally distinguish microcytic anemia caused by iron deficiency (in which RDW is increased) and thalassemia (in which RDW is normal). In macrocytic anemia it helps in distinguishing megaloblastic anemia (in which RDW is increased) and other macocytic anemias (in which RDW is often normal). Platelet evaluation: Platelet count [150 – 450 x 109/L] is determined from measurements of number of cells with sizes 2-20 fl in the “unlysed channel” Reported as cells x 109/L Mean platelet volume [6-8 fl] is measured from a histogram and is reflective of the true platelet volume! It is rarely clinically used. Reported in fl The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. Laboratory Hematology [This ptable is adapted from BLOOD: Principles & Practice of Hematology by Handin et al. Lippincott Press] The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. 7 Laboratory Hematology 8 RETICULOCYTE COUNT: Reticulocytes are newly produced RBCs that have extruded their nuclei but still show ribosomal RNA material that imparts a reticulated appearance to RBCs. They constitute about 1-2% of peripheral blood population and can be recognized as slightly larger than normal RBCs and with some blue/purple appearing fine dots (ribosomal RNA) causing polychromasia. The most common method of highlighting reticulocytes is a supravital stain to precipitate intracellular RNA. After staining, a thin peripheral smear is made and reticulocytes are counted by manual method. These cells can also be counted by flow cytometry. Reticulocytes are increased in any condition in which there is increased output of new RBC in the peripheral blood such as a response to bleeding and hemolysis and they are decreased in conditions of decreased production of RBC by the marrow. PERIPHERAL BLOOD EVALUATION: This is an important part of evaluation of many hematologic disorders. A peripheral blood smear is made under four main conditions: (i) The automated Coulter counter “flagged” an abnormality that triggers further evaluation (ii) A physician requests evaluation of peripheral blood smear by a pathologist based on clinical history, and (iii) At a pathologist’s request to further evaluate any hematologic disease process even when the CBC is normal such as suspected presence of parasites in the blood and within cells such as Ehrlichia (iv) As part of routine quality control mechanism by laboratories [The detailed description of a peripheral blood smear will be provided during the session for peripheral blood evaluation toward the end of the course] DETECTION OF FETAL HEMOGLOBIN: (By Kleihauer-Betke test) Detection of fetal hemoglobin (hemoglobin F) in individual RBCs is useful to establish the diagnosis of feto-maternal transfusion and also in the evaluation of Hb-F in patients with hemoglobinopathies. This test is based on the principle that Hb-F is resistant to elution by an acid whereas Hb-A washes off leaving ghosts of cells. A manual count yields the % of F cells present. The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended.