Efficacy of Enzyme Replacement Therapy in Fabry`s Disease
advertisement

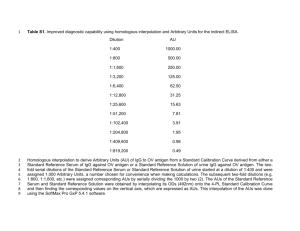
A MULTIDRUG, ANTIPROTEINURIC APPROACH TO ALPORT SYNDROME: A TEN-YEAR COHORT STUDY SUPPLEMENTAL MATERIAL Treatment Period MONTH-1: ACE-INHIBITOR THERAPY – Eligible patients were given 10 mg/day of benazepril. If treatment was well tolerated (see safety evaluations), one week later the dose was up-titrated to 20 mg/day and then maintained up to completion of the treatment period (Figure 1). MONTH 2: ARB ADD-ON THERAPY – Patients were given 80 mg of valsartan. If treatment was well tolerated, one week later the dose was up-titrated to 160 mg/day and then maintained up to completion of the treatment period. MONTH 3: I. NDCCB ADD-ON THERAPY – If systolic/diastolic BP was >120/80 mmHg, the heart rate was >50/min and PQ<20 msec, patients were given 60 mg/day of diltiazem. If treatment was well tolerated, the dose was up-titrated to 120 mg/day and eventually to 180 mg/day and then maintained up to completion of the treatment period. II. HMGCOA REDUCTASE INHIBITOR ADD-ON THERAPY – Patients not receiving diltiazem therapy were given 40 mg/day of fluvastatin. If ten days later liver transaminases and creatinphosphokynase serum levels were in normal range, the dose was up-titrated to 80 mg/day. In case of liver, muscular or renal toxicity, fluvastatin was back-titrated to 40 mg/day or withdrawn as deemed appropriate. MONTH 4: HMGCOA REDUCTASE INHIBITOR ADD-ON THERAPY – Fluvastatin was introduced also to patients receiving diltiazem. Recovery period At completion of the 4-month treatment period, all study treatments (benazepril, valsartan, diltiazem and fluvastatin) were withdrawn and patients were actively followed up to completion of the onemonth Recovery period (Figure 1). Extension After the recovery period, - patients were actively followed up until July, 2014 or until progression to an endpoint (ESRD or last available visit for those prematurely withdrawing from the study) by 3-6 monthly evaluations of. blood pressure, routine laboratory tests including safety parameters, serum lipids, urinary albumin excretion and spot urine A/C ratio (Table 1). During this long-term observation period all of them were maintained on the same treatment regimen that during the Treatment Period was associated with the largest antiproteinuric effect (Month 4, Figure 1). Measurements Blood pressure was recorded as the mean of 3 values taken 2 min apart, after 5-min rest in the sitting position, on the same (dominant) arm by a standard sphygmomanometer. Albuminuria was measured in three consecutive overnight urine specimens collected during the three days prior the day visit. The average value of the three collections was considered for the analyses. Serum creatinine was measured using a modified Jaffe’s method. CLEARANCE STUDIES - Before treatment initiation (month 0), at the end of the Treatment (month 4) and Recovery (month 5) periods, patients were admitted at the Department of Renal Medicine of the Clinical Research Center to have their GFR and RPF measured by the mean of three consecutive inulin and para-aminohippuric acid (PAH) renal clearances [1], respectively. Inulin and PAH concentrations in plasma and urine samples were determined using previously described colorimetric assays [2,3]. Clearance data were adjusted per 1.73 2 m2 of body surface area. Filtration fraction (FF) and renal vascular resistances (RVR) were calculated by standard formulas: FF = GFR/RPFx100; RVR = MAP/RPF To account for possible hematocrit changes associated with RAS inhibitor therapy, we also calculated the effective renal blood flow (eRBF) and the RVR as a function of eRBF (eRVR) by the following formulas: eRBF = RPF/ (1-hematocrit); eRVR = MAP/eRBF. SERUM AND URINARY PROTEIN MEASUREMENTS - Albumin and IgG concentrations in plasma and urine samples were determined using a sensitive enzyme-linked immunosorbent assay (ELISA). Briefly, diluted samples were placed in polystyrene wells coated with antibodies to human albumin (Sigma Chimica, Milan, Italy), IgG or IgM (Boehringer Mannheim, Milan, Italy). Goat anti-human albumin (American Qualex, La Miranda, CA) or IgG (Sigma Chimica) conjugated with alkaline phosphatase were added, followed by alkaline phosphatase substrate (Sigma Chimica), and optical density of wells read using a micro-ELISA reader. Fractional clearances of albumin-IgG were computed as: JAlb or IgG = (U/P) Alb or IgG/(U/P)IN Where (U/P) Alb or IgG and (U/P)IN are the urine-to-plasma concentration ratios of Albumin or IgG and inulin respectively. Other laboratory measurements were performed using routine laboratory techniques. Safety Evaluations and Concomitant Medications Blood pressure, serum potassium and creatinine and venous pH were measured within 7-10 days after first benazepril or valsartan administration and after each drug up-titration. Additional measurements were performed whenever deemed clinically appropriate. In case of symptomatic hypotension, hyperkalemia (serum potassium ≥5.5 mEq/L despite adequate correction of metabolic acidosis) or serum creatinine increase by more than 30% after any benazepril or valsartan up-titration, the dose of 3 the drug was back-titrated to the previous step or withdrawn. Throughout the whole treatment period, treatment was aimed at achieving and maintaining systolic and diastolic BP <120 and <80 mmHg, respectively. Concomitant BP lowering treatment with medications that do not directly affect glomerular sieving function (i.e., carvedilol, clonidine, doxazosine or diuretics) and therefore were not expected to interfere with the primary efficacy variable of the study was allowed. Treatment could be back-titrated or withdrawn to avoid symptomatic hypotension during the Remission Clinic treatment period and could be up-titrated to avoid BP values exceeding the safety threshold of 130/90 mmHg during the Run-in and Recovery periods, respectively. References 1. Campbell R, Sangalli F, Perticucci E, Aros C, Viscarra C, Perna A, Remuzzi A, Bertocchi F, Fagiani L, Remuzzi G, Ruggenenti P: Effects of combined ACE inhibitor and angiotensin II antagonist treatment in human chronic nephropathies. Kidney Int 2003;63: 1094-1103. 2. Perico N, Remuzzi A, Sangalli F, Azzollini N, Mister M, Ruggenenti P, Remuzzi G: The antiproteinuric effect of angiotensin antagonism in human IgA nephropathy is potentiated by indomethacin. J Am Soc Nephrol 1998;9: 2308-2317. 3. Remuzzi A, Perticucci E, Ruggenenti P, Mosconi L, Limonta M, Remuzzi G: Angiotensin converting enzyme inhibition improves glomerular size-selectivity in IgA nephropathy. Kidney Int 1991;39: 1267-1273. 4