Sample Collecting: body substances: blood, urine, faeces, sweat etc
advertisement
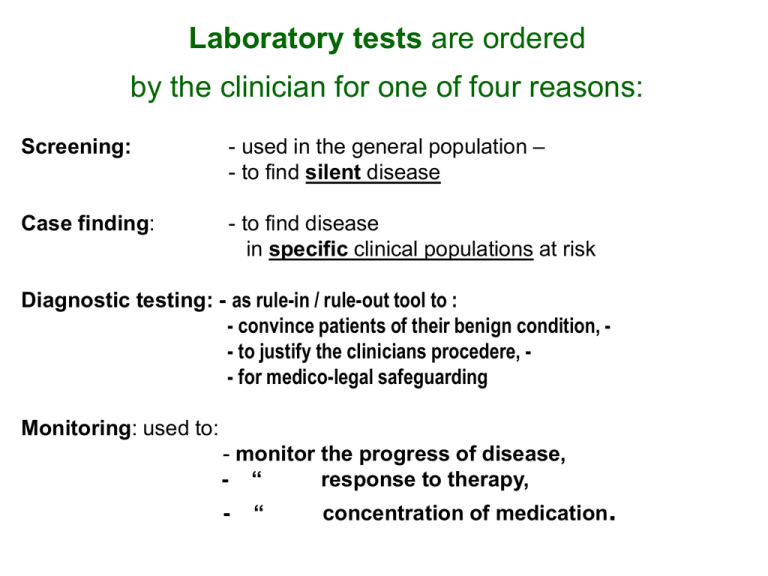
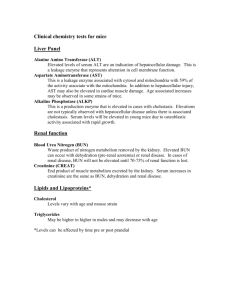
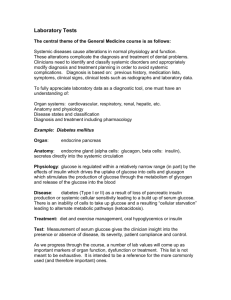
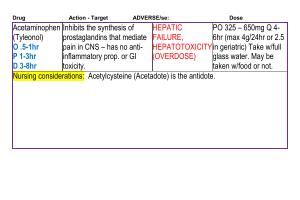
Laboratory tests are ordered by the clinician for one of four reasons: Screening: - used in the general population – - to find silent disease Case finding: - to find disease in specific clinical populations at risk Diagnostic testing: - as rule-in / rule-out tool to : - convince patients of their benign condition, - to justify the clinicians procedere, - for medico-legal safeguarding Monitoring: used to: - monitor the progress of disease, - “ response to therapy, - “ concentration of medication. Sample Collecting: body substances: blood, urine, faeces, sweat etc. collected in : URINE/STOOL/BLOOD - CONTAINERS Phlebotomist’s Equipment : • VACUTAINER TUBES - o EDTA (Lavender) o SST (Gold/ Serum) o SST (Speckled/Serum) o Citrate/Clotting (Lt Blue) o Fluoride Oxalate/Glucose (Grey) o Lithium Heparin (Green) o No Additive (Red) o Sod. Heparin (Dark Blue) VACUTAINER NEEDLES o 21 Gauge (Green) o 21 Butterfly (Green) o 22 Gauge (Black) o 23 Gauge Butterfly (Blue) o VACUTAINER BARREL How can one define a ‘Healthy Population’ • ? Health or Disease diagnosis ~ relies on findings of : true-negatives or true-positives ~ hampered by false-negatives or false positives • Is it possible to find a truly ‘normal individual’ ? – or a healthy population whose physiology is truly perfect ? • Without an ‘ideal population’ – any stated reference range will be falsly broad –( the 95% water-shed); • Optimal metabolic ranges may be quite narrow for many biochemical parameters Laboratory / Path-Lab. Tests • Routine Health Service tests : • Blood Chemistry • Blood Film Examination • Urine-analysis • Microbiology Special Health Service tests: • Cytology • Microscopy • Aspirated Material : - Exsudates - Transudates Blood Chemistry • • • • • Electrolytes Lipid-Profile Diabetes Check, RBS, GTT, HBA1c Renal Profile Hormone Assays Progesteron Estradiol, Testosterone, DHEA, ACTH, Catecholamines • Serum Protein Electrophoresis • Inflammation Markers • Tumor Markers ESR, CRP PSA, AFP, CEA, β-HCG CA153. CA27-29, CA19-9, CA 125, HER-2-neu, • Miscellanious LDH, AP Serum Sodium (Na+) - major extra-cellular cation • regulates blood and volume by its osmotic activity in the plasma (Osmolality) and in the lymphatic tissues • excreted by the kidneys, sweating • increased: Cushing’s Syndrome, drug-effects • decreased: Addison’s Disease, renal failure, metabolic acidosis, malignancies, drugs Serum Potassium (K+) - major intra-cellular cation - distal tubular secretion dependent on: » mineralcorticoids, acid-base balance drugs • major influence on muscle activity • if unbalanced : – diagnosis whether Hypo- or Hyper-kalaemia required – diagnosis whether Hypo- or Hyper-Adrenalism present – risk of metabolic / respiratory alkalosis or acidosis present Plasma Creatinine by-product from Creatine-metabolism • – single most useful measurement of renal function • normally varies little throughout the day • best monitoring tool for : renal secretory function glomerular filtration rate GFR Urea NH2CONH2 • - produced by protein consumption and the formation of ammonia • – raised levels (Uraemia/ Azotaemia) - sign of chronic renal failure, - can have pre-renal, renal and post-renal cause - can lead to Uraemic Syndrome, nausea, confusion . . Uric Acid • - end product of purine metabolism • ~ ↑ (Hper-uricemia) - predictive of gout , • ~ ↑ poly-cystic kidney disease, anemias • ~ ↑ hypothyroidism • ~ ↑ diuretics, salicylate Calcium (Ca2+) • defines clinical diagnosis whether Hypo- or Hypercalcaemia • clinically linked with • “ “ 1-ary Hyper-Parathyroidism, effects of drugs, radiation, malignancy, • clinically linked with Hypo-Parathyroidism : associated with : other endocrine disorders, symptomatically : cramps, spasms, tetany. nail + skin disorders Diabetic Monitoring • Normal Serum Glucose Concentration 75mg-110mg/dl 4.2 - 6.4 (mmol/l • • Glucose Tolerance Test (GTT) (2 hr post-glucose loading analysis) in SI – units < 7.8 (8.9 mmol/l ) n.r. Glycosylated Hemoglobin ( HbA1c) ( 3.8 – 6.4) dependent on circulating erythrocyte (120 days) Further Glycaemic Testing becomes indicated after symptom development: - excessive thirst, glycosuria, skin irritation (if Random BS > 11 mmol/l Diabetes ) - fasting glucose > 7 mmol/l - plasma glucose 2 hrs after GTT-loading > 11.1 - HBA!c, plasma-lipid profile, . . . Serum-Lipids • Cholesterol – insoluble in water – carrier proteins : ‘Lipoproteins’ Total Cholesterol Triglycerides LDL- Cholesterol LDL- Cholesterol desirable borderline high . < 200 200 – 240 > 240 [mg/dl ] 5.2 6.1 [ S.I.] < 150 150 – 200 > 200 1.7 2.25 < 130 130 – 160 > 160 2.6 4.1 > 60 if less than 39 1.5 1. Liver Function Tests • • • • • • • Serum Transaminases Serum Aspartate Transaminase (AST or SGOT) Serum Alamine Aminotransferase (ALT or SGPT) Serum Alkaline Phosphatase (AP) Serum Gamma Glutamyl Transpeptidase (GGT) Serum Bilirubin Serum Albumin Bilirubin ~ waste-product of the erythrocyte degradation cycle → Serum ( free or un-conjugated B. - as ‘bilirubin-albumin complex’ ) ( conjugated in liver - as ‘bilirubin glucoronide’ ) • ↑ conjugated - hepatobiliary disease - obstructive post-hepatic jaundice • ↑ un-conjugated - Gilbert’s Syndrome, neonatal jaundice - haemolysis, pre-hepatic jaundice → Urine (uro-bilinogen) hemolytic anemia, toxic hepatitis, mononucleosis Clinical Hematology examines ( sample bottle EDTA) • • BLOOD CELL DEVELOPMENT of : Red Blood Cells (RBCs, Erythrocytes) White Blood Cells (WCs, Leukocytes) BLOOD CELL COUNTS Units Reported By Automated Counting: (RBCs), (WC), Platelets Complete blood count CBC : HEMOGLOBIN - Variants HEMATOCRIT (PACKED CELL VOLUME) REDCELL- Count - with morphology - MCV, MCH, MCHC, PLATELETS WHITE-CELL- Count with morphology WHITE-CELL- Count with DIFFERENTIAL Count Neutrophils Eosinophils Basophils onocytes Lymphocytes EXAMINATION OF THE PERIPHERAL BLOOD FILM • • Microscopic Examination of the Blood Film Normal Leukocyte Morphology Blood Cell Alterations • • • • ADDITIONAL HEMATOLOGY PROCEDURES Reticulocyte Counts Erythrocyte Sedimentation Rate (ESR) Blood-Coagulation Red-Cell (Erythrocyte) –Population PERIPHERAL BLOOD FILM : differentiation by Color, Shape: Macro-cytosis → Megaloblastic Anemia -normochromic Micro-cytosis → Iron-deficincy-An. - hypochromic - hyperchromic Aniso-cytosis Poikolo-cytosis Presence of : Sickle-cells Target-cells Helmet-cells Spherocytes Hemoglobin Variants S, C, D, E Hemoglobin-Derivatives → Microcirculation (Met-, Oxy-, Carboxy-, Cyanomet- H. ) Smallest integral life forms observed under ‘Darkfield Microscopy’ seen as "tiny white dots" so called Protits; they change according Pleomorphism or the Cyclogenia of Microbes first into: viral forms which can change into spores and fungi. bacterial forms followed by White-Cell (Leukocyte) -Population PERIPHERAL BLOOD FILM : if increased: → (leucocytosis) Neutrophils → (neutrophilia ) Eosinophils → (eosinophilia ) Basophils Monocytes Lymphocytes (⅓) – small, large, reactive → (lymphocytosis) Myeloid Series (⅔) DEFICIENCIES: Leukopenia, Neutropenia, Lymphocytopenia etc … Fatigue • Ongoing fatigue Signs I Symptoms I Findings - reduced daily activity - very limited exercise tolerance • Muscle pain - worse after exercise • Migrating polyarthralgia • Recurrent headaches • Depression • Cognitive disturbances • Low blood pressure / Postural hypotension • Commonly reported Symptoms & Findings from a large number of ‘dys-functional individuals’ : • • • • • • • • Fatigued – easily out of puff Muscle weakness, muscle pain, - worse after exercise Migrating polyarthralgia, joints ache, - feel stiff Sleep disturbance -Insomnia - Hypersomnia Low grade feverishness, sweating disorder, Chronic sore throat, - swollen lymph nodes Recurrent headaches, unexplained depression Cognitive disturbances, - snowflakes, buzzing noises, - crawling sensation, brain fag • Low morning blood pressure, - postural hypotension • Reduced daily activity, - very limited exercise tolerance Disease Labeling or Health Monitoring ? Traditional Lab-testing Functional Lab-Assessment What ? Why? identify single cause Complex InterRelationships Separation of Symptoms Connectedness of Symptoms quantifies Pathology quantifies Function . . is there a shift in the spectrum of diseases that we see and experience ? . . need for new biochemical ( or other ! ) markers ? : - not only to diagnose disease - sensitive to monitor metabolism more dynamically - treatment progress “ • • • • • “ T1 – T2 responses Neurotransmitters, Cytokines, Trace-elements Antioxidfant-Activity, DNA-adducts Endocrine Disruptors , Free pleo-morphic shift of pathogens, life-blood-analysis • Apoptosis Microbial Pathogens • VIRUSES • BACTERIA SINGLE-CELL PARASITES -100 nanometers, multiply through host DNA - at least 10 times larger than viruses, 1 mcmr (1 millionth of a meter) - reproduce independently - at least 100 times larger, 0.1 millimeter long • MULTI CELLULAR - can be seen with the naked eye PARASITES ======================================================= Pleomorphism = theory of dynamic changes and transmutations between pathogens