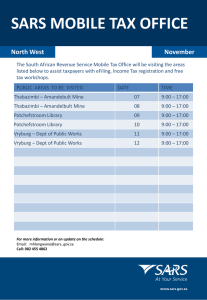
SARS
advertisement

COMMUNICABLE DISEASE MANUAL POLICIES / PROCEDURES SEVERE ACUTE RESPIRATORY SYNDROME (SARS) OBJECTIVE: Control and management of Severe Acute Respiratory Syndrome (SARS). DESCRIPTION: Severe Acute Respiratory Syndrome (SARS) is a viral respiratory illness caused by a coronavirus, called SARS associated coronavirus (SARS-CoV). These viruses are a common cause of mild to severe upper-respiratory illness in humans and animals. Coronaviruses can survive in the environment for as long as three (3) hours. This family of viruses causes the common cold and pneumonia. SARS was first reported in China in February 2003. Transmission of SARS is mainly by close person-to-person contact. The virus that causes SARS is thought to be transmitted by respiratory droplets (droplet spread) produced when an infected person coughs or sneezes. The virus also can spread when a person touches a surface or object contaminated with infectious droplets and the touches his or her mouth, nose, or eye(s). In addition, it is possible that the SARS virus might spread through the air. Close contact in relation to SARS means having cared for, or lived with someone with SARS or having had direct contact with respiratory secretions or body fluids of a patient with SARS. Examples of close contact include kissing or hugging, sharing eating or drinking utensils, talking to someone within three (3) feet, and touching someone directly. Close contact does not include activities like walking by a person or sitting across a waiting room or office for a brief time. SARS is highly contagious and has been spread to health care workers, close personal contacts, schools and communities. The incubation period for SARS is typically 2-7 days and can extend up to ten (10) days. The illness begins with a high fever (temperature greater than 100.4º F or 38º C). The fever often is high, sometimes associated with chills and rigors, and might be accompanied by other symptoms of headache, malaise, and body aches. Some people also have mild respiratory symptoms at the onset of illness. Typically, rash, neurologic and gastrointestinal findings are absent. About 10% to 20% of patients have diarrhea during the febrile prodrome. After 3-7 days, a lower respiratory phase begins with the onset of a dry, non-productive cough and dyspnea. Most patients develop pneumonia that can progress to hypoxemia. In 10% to 20% of cases, the respiratory illness is severe enough to require intubation and mechanical ventilation. The case fatality rate is 9.6%. See the CDC website for the most current recommendations and information at: http://www.cdc.gov/ncidod/sars. EQUIPMENT: MDSS User Manual. Disease specific form found in MDSS. MDCH SARS Screening Form (12-4-03) (Attachment A) and SARS Suspect Illness Case Report (Attachment G) will be found as hard copy in the Communicable Disease Case Forms Notebook in the nursing area. The MDCH website at www.michigan.gov/mdch and www.michigan.gov/cdinfo and CDC website at www.cdc.gov/ncidod/sars will have the most recent updates posted. POLICY: Legal Responsibility: Public Health Code, MCL 333.1101 et. Seg. And rules thereunder. NOTIFY MDCH IMMEDIATELY via fax (517-335-8263) or phone (517-335-8165) of possible suspect case. Follow up within 24 hours and fax or call currently available information to MDCH promptly. Also enter into MDSS within 24 hours of receipt of referral. D:\687285844.docPage 1 of 3 PROCEDURE: A. Case Investigation 1. Referral received from hospital, medical doctor, laboratory, or automatically through MDSS. 2. Notify MDCH (see above); notify CD Supervisor, Medical Director and HD Emergency Manager. 3. Document all case investigation proceedings. 4. Contact client or physician to start process of completing MDCH SARS Screening Form (12-4-03) and SARS Suspect Illness Case Report if needed.. 5. Continue to keep MDCH, Medical Director , HD Emergency Manager, Regional Epidemiologist and CD Supervisor updated. B. Updated Interim U.S. Case Definition of Severe Acute Respiratory Syndrome (SARS), (12-12-03) (See Attachment B - 3 pages) 1. The most recent version will be posted at: http://www.cdc.gov/ncidod/sars/casedefinition.htm C. Laboratory and Specimens 1. MDCH and CDC continue to update their information on diagnosis, specimens, etc. The most recent updates will be posted at: http://www.cdc.gov/ncidod/sars/diagnosis.htm. See Collection of Specimens from Potential SARS in Michigan (Attachment C - 8 pages). 2. Initial diagnostic testing for suspected SARS patients should include chest x-rays of recent cases of atypical pneumonia, pulse oximetry, blood cultures, sputum Gram's stain and culture, and testing for viral respiratory pathogens, notably Influenza A and B and respiratory syncytial virus. A specimen for Legionella and pneumococcal urinary antigen testing should also be considered. Clinicians should save any available clinical specimens (respiratory, blood, and serum) for additional testing until a specific diagnosis is made. Acute and convalescent (greater than 28 days after onset of symptoms) serum samples should be collected from each patient who meets the SARS case definition. Paired sera and other clinical specimens can be forwarded through State and local health departments for testing at CDC. Specific instructions for collecting specimens from suspected SARS patients are available. For information about testing of specimens at laboratories other than CDC, please refer to the consent forms and other documents for coronavirus antibody testing at state public health laboratories and RTPCR testing at the Laboratory Response Network (Attachment D-4 pages). Clinicians evaluating suspected cases should use standard precautions (e.g., hand hygiene) together with airborne (e.g., N-95 respirator) and contact (e.g., gowns and gloves) precautions (see the Updated Interim Domestic Infection Control Guidance in the Health-Care Community Setting for Patients with Suspected SARS). Until the mode of transmission has been defined more precisely, eye protection also should be worn for all patient contact. As more clinical and D:\687285844.docPage 2 of 3 epidemiologic information becomes available, interim recommendations will be updated. D. Control Measures 1. See SARS Infection Control and Exposure Management at http://www.cdc.gov/ncidod/sars/ic.htm. On this website, CDC provides guidance for infection control for individuals in a variety of health care and non-health care settings. 2. Details of travel advisories can be found at http://www.cdc.gov/ncidod/sars/traveladvice.htm. 3. MDCH has developed a screening tool, which may be used by clinicians to assist them in determining if a patient can be considered a probable SARS case. They also have developed a flowchart to assist with management of possible exposure to SARS (Attachment E). These forms are located on the MDCH website at: http://michigan.gov/mdch/sars. The CDC Appendix C3: Algorithm for Evaluation and Management of Patients Hospitalized with CXR Evidence of Pneumonia in the Absence of Known SARS Activity Worldwide (12-4-03) is located at: www.cdc.gov/ncidod/sars (Attachment F). 4. See Michigan Guidance to SARS located in Notebook in nursing area. E. Complete case investigation using either the new case forms or the disease specific forms of MDCH SARS Screening Form (12-4-03) and SARS Suspect Illness Case Report. Copy and fax all updated information to MDCH. F. References 1. Refer to current Redbook and current Control of Communicable Diseases Manual. 2. MMWR, December 12, 2003; Volume 52, Number 49, 1202-1206. 3. MDCH website: http://michigan.gov/mdch/sars and www.michigan.gov/cdinfo CDC website: http://www.cdc.gov/ncidod/sars WHO website: http://www.who.int/csr/sarscountry/en BCHD website: http://www.berriencounty.org/healthdept/ berrienhealthupdates/sarsinfo.htm 4. Michigan Guidance to Severe Acute Respiratory Syndrome (SARS) located in each office in the nursing area. D:\687285844.docPage 3 of 3