Severe Acute Respiratory Syndrome (SARS)
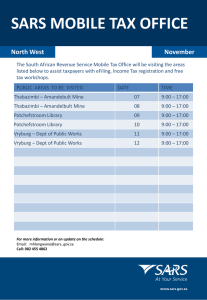
advertisement

Severe Acute Respiratory Syndrome (SARS) From DrGreene.com Definition: Severe Acute Respiratory Syndrome (SARS) is a contagious respiratory infection that was first described on February 26, 2003. It was first identified as a new disease by WHO physician Dr. Carlo Urbani who diagnosed it in a 48-year-old businessman who had traveled from the Guangdong province of China, through Hong Kong, to Hanoi, Vietnam. The businessman died from the illness. Dr. Urbani subsequently died from SARS on March 29, 2003 at the age of 46. In the meantime, SARS began to spread, and within 6 weeks of its discovery, it had infected thousands of people around the world, including people in Asia, Australia, Europe, and North and South America. Schools had closed throughout Hong Kong and Singapore. National economies were affected. The WHO had identified SARS as a global health threat, and issued an unprecedented travel advisory. But it wasn't clear whether SARS would become a global pandemic, or would settle into a less aggressive pattern. SARS is a serious form of atypical pneumonia, resulting in acute respiratory distress and sometimes death. It is a dramatic example of how quickly world travel can spread a disease. It is also an example of how quickly a networked health system can respond to an emerging threat. Alternative Names: SARS Causes And Risk: SARS appears to be caused by a virus or viruses. The first reports from virologists suggested the cause was a new virus in the paromyxovirus family (the same family as RSV, measles, and mumps). Subsequent evidence pointed more strongly to a new member of the coronavirus family (the same family that can cause the common cold). The discovery of these viral particles represents some of the fastest identification of a new organism in history. SARS is clearly spread by droplet contact. When someone with SARS coughs or sneezes, infected droplets are sprayed into the air. With other coronaviruses, the virus can live on hands, tissues, and other surfaces for up to 6 hours in these droplets and up to 3 hours after the droplets have dried. (Also, with other coronaviruses, re-infection is common.) While droplet transmission through close contact was responsible for most of the early cases of SARS, evidence began to mount that SARS might also spread by hands and other objects the droplets had touched. Airborne transmission was a real possibility in some cases. Live virus had even been found in the stool of people with SARS. Preliminary estimates are that the incubation period is usually between 2 and 7 days, although there have been documented cases where the onset of illness was considerably faster or slower. People with active symptoms of illness are clearly contagious, but it is not known how long contagiousness may begin before symptoms appear or how long contagiousness might linger after the symptoms have disappeared. Prevention: Minimizing contact with people with SARS minimizes the risk of the disease. This might include minimizing travel to locations where there is an uncontrolled outbreak. Where possible, direct contact with people with SARS should be avoided until 10 days after the fever and other symptoms are gone. The CDC has identified hand hygiene as the cornerstone of SARS prevention. This might include hand washing or cleaning hands with an alcohol-based instant hand sanitizer. People should be taught to cover the mouth and nose when sneezing or coughing. Respiratory secretions should be considered to be infectious, which means no sharing of food, drink, or utensils. Commonly touched surfaces can be cleaned with an EPA approved disinfectant. In some situations, masks and goggles may be useful for preventing airborne or droplet spread. Gloves might be used in handling potentially infectious secretions. Symptoms: The hallmark symptoms are fever greater than 100.4 F (38.0 C) and cough, difficulty breathing, or other respiratory symptoms. Symptoms found in more than half of the first 138 patients included (in the order of how commonly they appeared): fever chills and shaking muscle aches cough headache Less common symptoms include (also in order): dizziness productive cough (sputum) sore throat runny nose nausea and vomiting diarrhea Signs And Tests: Listening to the chest with a stethoscope (auscultation) may reveal abnormal lung sounds. In most people with SARS, progressive chest X-ray changes or chest CT changes demonstrate the presence of pneumonia. Much attention was given early in the outbreak to developing a quick, sensitive test for SARS. General tests used in the diagnosis of SARS might include: a chest X-ray or chest CT a CBC (people with SARS tend to have a low white blood cell count (leukopenia), a low lymphocyte count (lymphopenia), and/or a low platelet count (thrombocytopenia). clotting profiles (often prolonged clotting) blood chemistries (LDH levels are often elevated. ALT and CPK are sometimes elevated. Sodium and potassium are sometimes low). Treatment: People suspected of having SARS should be evaluated immediately by a physician. Antibiotics are sometimes given in an attempt to treat bacterial causes of atypical pneumonia. Antiviral medications have also been used. High doses of steroids have been employed to reduce lung inflammation. In some serious cases, serum from people who have already gotten well from SARS (convalescent serum) has been given. Evidence of general benefit of these treatments has been inconclusive. Other supportive care such as supplemental oxygen, chest physiotherapy, or mechanical ventilation is sometimes needed. Prognosis: The early death rate in SARS was about 4 percent of those diagnosed. This is expected to change over time, as the virus and available medical care both change. Between 10 and 20 percent of those diagnosed with SARS have been sick enough to require mechanical ventilation. More than that have been sick enough to require ICU care. Complications: respiratory failure liver failure heart failure myelodysplastic syndromes What Is SARS? Provided by Centers for Disease Control and Prevention What is SARS? Severe acute respiratory syndrome (SARS) is a respiratory illness that has recently been reported in Asia, North America, and Europe. The symptoms and signs of SARS The illness usually begins with a fever (measured temperature greater than 100.4 蚌 [>38.0 蚓]). The fever is sometimes associated with chills or other symptoms, including headache, general feeling of discomfort and body aches. Some people also experience mild respiratory symptoms at the outset. After 2 to 7 days, SARS patients may develop a dry, nonproductive cough that might be accompanied by or progress to the point where insufficient oxygen is getting to the blood. In 10 percent to 20 percent of cases, patients will require mechanical ventilation. For more information, see the MMWR dispatch. If I were exposed to SARS, how long would it take for me to become sick? The incubation period for SARS is typically 2 to 7 days; however, isolated reports have suggested an incubation period as long as 10 days. The illness usually begins with a fever (>100.4 蚌 [>38.0 蚓]) (see signs and symptoms, above). What medical treatment is recommended for patients with SARS? CDC currently recommends that patients with SARS receive the same treatment that would be used for any patient with serious community-acquired atypical pneumonia of unknown cause. Is the use of ribavirin (or other antiviral drugs) effective in the treatment of patients with SARS? At present, the most efficacious treatment regimen, if any, is unknown. In several locations, therapy has included antivirals such as oseltamivir or ribavirin. Steroids also have been given orally or intravenously to patients in combination with ribavirin and other antimicrobials. In the absence of controlled clinical trials, however, the efficacy of these regimens remains unknown. Early information from laboratory experiments suggests that ribavirin does not inhibit virus growth or cell-to-cell spread of one isolate of the new coronavirus that was tested. Additional laboratory testing of ribavirin and other antiviral drugs is being done to see if an effective treatment can be found. SARS Symptom Chart Allergic Rhinitis Asthma Cold Flu Pneumonia SARS Body Aches and Pains • •• •• •• •• •• •• • • • Chills/Rigors Cough • • • • Diarrhea • Dizziness • Fatigue/Malaise • ••• ••• •• Fever • ••• ••• •• Headache • •• •• •• •• • Nasal Congestion •• Nausea/Vomiting • Painful Breathing • Productive Cough Shortness of Breath • •• Sneezing • •• Sore Throat • •• • • • • • •• •• • • • KEY ••• •• • Blank = Commonly present, high or severe = Commonly present = Can be present = Not usually present The SARS Virus Provided by Centers for Disease Control and Prevention A new disease called SARS The Centers for Disease Control and Prevention (CDC) is investigating a new disease called severe acute respiratory syndrome (SARS) that has recently been reported in Asia, North America, and Europe. As of April 13, about 190 cases of SARS had been reported in the United States. This fact sheet provides basic information about the disease and what is being done to combat its spread. Symptoms of SARS In general, SARS begins with a fever greater than 100.4 蚌 [>38.0 蚓]. Other symptoms may include headache, an overall feeling of discomfort, and body aches. Some people also experience mild respiratory symptoms. After 2 to 7 days, SARS patients may develop a dry cough and have trouble breathing. How SARS spreads The primary way that SARS appears to spread is by close person-to-person contact. Most cases of SARS have involved people who cared for or lived with someone with SARS, or had direct contact with infectious material (for example, respiratory secretions) from a person who has SARS. Potential ways in which SARS can be spread include touching the skin of other people or objects that are contaminated with infectious droplets and then touching your eye(s), nose, or mouth. This can happen when someone who is sick with SARS coughs or sneezes droplets onto themselves, other people, or nearby surfaces. It also is possible that SARS can be spread more broadly through the air or by other ways that are currently not known. Who is at risk for SARS Cases of SARS continue to be reported mainly among people who have had direct close contact with an infected person, such as those sharing a household with a SARS patient and health care workers who did not use infection control procedures while taking care of a SARS patient. In the United States, there is no indication of community spread at this time. CDC continues to monitor this situation very closely. Possible cause of SARS Scientists at CDC and other laboratories have detected a previously unrecognized coronavirus in patients with SARS. The new coronavirus is the leading hypothesis for the cause of SARS, however, other viruses are still under investigation as potential causes. CDC Lab Sequences Genome of New Coronavirus Provided by Centers for Disease Control and Prevention The Centers for Disease Control and Prevention (CDC) announced that it has sequenced the genome for the coronavirus believed to be responsible for the global epidemic of severe acute respiratory syndrome or SARS. The CDC sequence is nearly identical to that determined by a Canadian laboratory late last week. The significant difference is that the CDC-determined sequence has 15 additional nucleotides, which provides the important beginning of the sequence, CDC scientists said. The results came just 12 days after a team of 10 scientists, supported by numerous technicians, began working around the clock to grow cells taken from a throat culture taken from one of the SARS patients in Vero cells (African green monkey kidney cells) in order to reproduce the ribonucleic acid (RNA) of the disease-causing coronavirus. The new sequence has 29,727 nucleotides, which places it well within the typical RNA boundaries for coronaviruses. Members of this viral family tend to have between 29,000 and 31,000 nucleotides. Identifying the genetic sequence of a new virus is important to efforts to treat or prevent it, said Dr. Julie Gerberding, CDC director. "Research laboratories can use this information to begin to target antiviral drugs, to form the basis for developing vaccines, and to develop diagnostic tests that can lead to early detection." In sequencing the genome, CDC scientists worked closely with coronavirus experts at academic institutions across the United States. "This is an active, working community of scientific experts who have been contributing their knowledge and expertise throughout this investigation," said William Bellini, Ph.D., SARS laboratory team coordinator. The nearly identical findings in the US and Canada are important because they were derived from different individuals who were infected in different countries. This suggests that the virus probably originated from a common source. The CDC's analysis of the virus is far from finished, officials emphasized. Because coronaviruses have the ability to mutate rapidly, scientists will compare the sequences from viruses isolated in cell culture to those obtained from diseased tissues taken from SARS patients. "This is essentially a draft. Now we need to see if what we have identified in the laboratory matches what's causing disease in patients," Bellini said. But the groundbreaking work of isolating the genomic sequence speeds the task of comparison