SARS article group 1 - ismarul-epid
advertisement
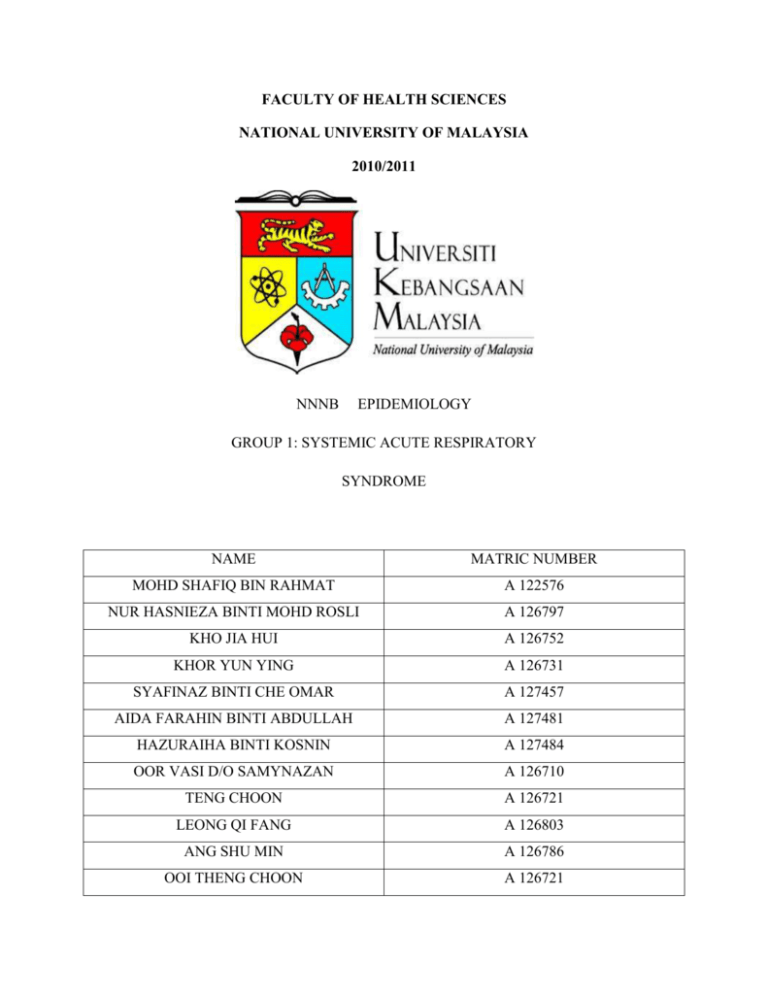
FACULTY OF HEALTH SCIENCES NATIONAL UNIVERSITY OF MALAYSIA 2010/2011 NNNB EPIDEMIOLOGY GROUP 1: SYSTEMIC ACUTE RESPIRATORY SYNDROME NAME MATRIC NUMBER MOHD SHAFIQ BIN RAHMAT A 122576 NUR HASNIEZA BINTI MOHD ROSLI A 126797 KHO JIA HUI A 126752 KHOR YUN YING A 126731 SYAFINAZ BINTI CHE OMAR A 127457 AIDA FARAHIN BINTI ABDULLAH A 127481 HAZURAIHA BINTI KOSNIN A 127484 OOR VASI D/O SAMYNAZAN A 126710 TENG CHOON A 126721 LEONG QI FANG A 126803 ANG SHU MIN A 126786 OOI THENG CHOON A 126721 1.0 INTRODUCTION On 12 March 2003, the World Health Organization (WHO) issued a global alert on the outbreak of a new form of pneumonia-like-disease. The illness, officially known as severe acute respiratory syndrome (SARS), is potentially fatal and highly contagious, and has spread quickly to many parts of the world in a matter of a few weeks. Aided by globalization and the ease of air travel today, the disease has been reported in many countries such as China, Hong Kong, Vietnam, Singapore, Canada, US, with a large number of infections and a significant number of deaths. Since SARS is transmitted person-to – person, extermination of the agents of transmission would not be a plausible solution. There are three main factors that make SARS a particularly difficult problem to deal with. First, victims who suffer from the illness display symptoms that are very much similar to those of the common flu. It usually begins with a high fever (over 38ºC), accompanied by symptoms such as headache, sore throat, shortness of breath and dry cough. This makes it difficult to distinguish SARS from the typical cold. Before the alert on the disease was sounded, many initial cases were wrongly diagnosed as common flu; and general practitioners sent patients home prescribing them with regular antibiotics. The second worrying characteristic of SARS is that it spreads from person-to person with ease. Experts have established that the illness is spread by “close contact”. The virus is believed to have the resilience to survive out of the human body for a few hours. Hence, an infected person can release droplets of bodily fluids containing the virus into the air when coughs, or when he rubs his mouth or nose and touches an object. The virus can be passed on to a second person who breathes in the droplets, or who touches a contaminated object such as door knob and rubs his face. The ease of infection has led to a great number of people being infected at the onset of the outbreak. Investigations have shown that most of the infected are mostly family members and friends of the victim, or health workers. Lastly, SARS is dangerous because with an incubation period of less than ten days, it acts fast-and in some cases, kills fast. Although its fatality rate is not exceptionally high at 4%, its 1 high infection rate can result in a significant number of deaths. SARS is also more dangerous for older people who have weaker immune systems or are already suffering from health complications like heart problems, diabetes and high blood pressure. Most of the victims who killed by SARS were idle-aged or older folks with inherent health problems. For this group of people, SARS has the capability to rapidly complicate their existing health problems and cause their physical conditions to deteriorate rapidly. However, there were also a few cases whereby fit and young adults fell ill quickly and have to breathe with the aid of respirators within a week of infection. The new coronavirus was isolated in Vero E6 cells from nasal and throat swab specimens of two patients in Thailand and Hong Kong with suspected SARS. The isolate was identified initially as a coronavirus by electron microscope (EM). The little hooks sticking out of the viral body are the telltale characteristics that help classify the pathogens as members of the coronavirus family. The identity was corroborated by results of immunostaining, indirect immunofluorescennce antibody (IFA) assays, and reverse transcriptase-polymerase chain reaction (RT-PCR) with sequencing of a segment of the polymerase gene. IFA testing of sera and RT-PCR analysis of clinical specimen from SARS cases were positive for the new coronavirus. Coronavirs particles were also identified by EM in cells obtained by bronchial lavage from a patient with SAS. Sequence analysis suggested that this new agent is distinct from other known coronavirus. As of today, the spread of SARS has been fully contained, with the last infected human case seen in June 2003 (disregarding a laboratory induced infection case in 2004). However, SARS is not claimed to have been eradicated (unlike smallpox), as it may still be present in its natural host reservoirs (animal populations) and may potentially return into the human population in the future. In late May 2003, studies from samples of wild animals sold as food in the local market in Guangdong, China found that the SARS coronavirus could be isolated from palm civets(Paguma sp.), but the animals did not always show clinical signs. The preliminary conclusion was that the SARS virus crossed the xenographic barrier from palm civet to humans, and more than 10,000 masked palm civets were destroyed in Guangdong Province. Virus was 2 also later found in raccoon dogs (Nyctereuteus sp.), ferret badgers (Melogale spp.) and domestic cats. In 2005, two studies identified a number of SARS-like coronaviruses in Chinese bats Phylogenetic analysis of these viruses indicated a high probability that SARS coronavirus originated in bats and spread to humans either directly, or through animals held in Chinese markets. 2.0 EPIDEMIOLOGY 2.1 Malaysia In Malaysia, the outbreak resulted is two deaths due to the probability of SARS in Jerantut, Pahang and Penang. The victim who involved with history has ever visited China or Singapore. The total number of cases includes those who've recovered or died.This Table shows the incidence of SARS in Malaysia since WHO records began. Infection Mortality Recovered Reclassified 8 2 5 2 “Table 1. Showing number of infection, mortality, recovered and reclassified cases of SARS in Malaysia from 5 April to 24 May 2003.” 2.2 Asia In 2003, SARS became an outbreak of cases in the hospital systems of Hong Kong, Vietnam, Singapore and been transmitted to many county in Asia. The infection has possibility start from Guangdong, China. 2.2.1 Hong Kong The Hong Kong index patient (the physician from Guangdong, China) infected 12 other persons who had been staying at the same hotel. Two of these individuals were subsequently responsible for outbreaks in two local hospitals. The Hong Kong health authorities immediately implemented enhanced infection-control procedures in all hospitals in Hong Kong, including 3 stringent barrier and respiratory protection for healthcare workers, daily environmental disinfection of affected wards, and cohorting of SARS patients. Towards the end of March 2003, a further SARS outbreak occurred among residents of Amoy Gardens, Hong Kong, with a total of 320 SARS cases in less than three weeks. The probable index patient was a patient suffering from chronic renal failure; in addition to person-to-person spread and to the use of communal facilities such as lifts and staircases, the SARS virus may have been spread through the sewage systems of the buildings (Government of Hong Kong Special Administrative Region). “Figure 1.Epidemic curve, Hong Kong.” After the initial phase of exponential growth, the rate of confirmed SARS cases fell to less than 20 per day by April 28. The Hong Kong epidemic seems to have been under control even earlier, by early April 2003, in the sense that each case had, already by then, failed to replace itself. The main reason for this would have been the reduction in the contact rate between infectious individuals and the rest of the population. At the beginning of June, public hospitals attempted to resume normal service, grappling with a backlog of an estimated 16 000 postponed operations because of the suspension of 30% of 4 the medical services during the SARS crisis. By June 16, 1755 cases of SARS had been diagnosed in Hong Kong. 295 patients (16.8%) had died. 1386 patients (79.0%) had recovered. Around 30% of cases occurred in healthcare workers. Among these, nurses were the most exposed category, accounting for about 55% of all infected healthcare workers. 15% were doctors, 27% support staff. Eight medical workers had died by June 2.On June 23, the WHO removed Hong Kong from its list of areas with recent local transmission of SARS. 2.2.2 Vietnam The outbreak in Vietnam began on February 26, when a 48-year-old Chinese-American businessman was admitted to the French hospital in Hanoi with a 3-day history of high fever, dry cough, myalgia and a mild sore throat. He had previously been in Hong Kong, where he visited an acquaintance staying on the 9th floor of the hotel where the Guangdong physician was a guest. By March 5, secondary probable SARS cases were identified among health care workers in Hanoi, and subsequently 63 people were infected. On April 28, the WHO removed Vietnam from the list of affected areas, making it the first country to successfully contain its SARS outbreak. The absence of any new cases for a continuous 20-day period (the duration of two incubation periods) was an encouraging indicator that appropriate detection and protection measures, as recommended by the WHO, were able to contain outbreaks and prevent their further spread: Prompt identification of persons with SARS, their movements and contacts; Effective isolation of SARS patients in hospitals; Appropriate protection of medical staff treating these patients; Comprehensive identification and isolation of suspected SARS cases; Exit screening of international travelers; Timely and accurate reporting and sharing of information with other authorities and/or governments. 5 2.2.3 Singapore Close contact is usually required for transmission in most cases. The index case of SARS in Singapore was a previously healthy 23-year-old woman of Chinese ethnicity who had been staying on the 9th floor of Hotel M during a vacation to Hong Kong from February 20-25, 2003. She developed fever and a headache on February 25 and a dry cough on February 28. She was admitted to a hospital in Singapore on March 1. At that time, SARS had not yet been recognized as a new disease easily spread in hospitals. As a result, hospital staffs were unaware of the need to isolate patients and protect them. Over a period of several days, the index patient infected at least 20 other people. No further transmission from this patient was observed after strict infection control measures were implemented. The virus initially spread rapidly among hospital staff, patients, visitors, and their close family contacts. Later on, spread of infection between hospitals occurred when patients with underlying disease - which masked the symptoms of SARS - were transferred to other hospitals, placed in rooms with other patients, and managed without adequate protective equipment (WHO). The outbreak in Singapore was amplified by several so-called "super spreaders. 144 of Singapore's 206 probable cases have been linked to contact with only 5 individuals (WHO). 6 “Figure2.Probable cases of severe acute respiratory syndrome, by reported source of infection Singapore, February 25-April 30, 2003.” On April 20, after the identification of a cluster of illness among employees at a crowded wholesale market, the market was closed for 15 days and more than 400 persons were placed in home quarantine. The spread of infection was limited to only 15 other persons.In Singapore, 76% of infections were acquired in a healthcare facility; the remainder either had household, multiple, or unknown exposures. Due to rigorous contact tracing and isolation procedures, 81% of probable SARS cases had no evidence of transmission to other persons with a clinically identifiable illness. Of the 84 (42%) healthcare workers with probable SARS, 49 were nurses; 13, physicians; and 22, persons with other occupations (attendants, radiographers, housekeepers, a porter, and a cleaning supervisor); no SARS cases have been reported among laboratory workers or pathologists.238 cases of SARS were diagnosed in Singapore; 33 patients died. On May 31, Singapore was removed from the list of areas with recent local transmission (WHO). 2.2.4 China Up until mid-April, the Chinese authorities underestimated the magnitude of the epidemic in Beijing, with only 37 cases having been reported by April 19. In the following two days, the Chinese authorities announced more than 400 new SARS cases. Additional reports indicated that 7 SARS had spread to other provinces, including western Guangxi, northern Gansu, and Inner Mongolia. On April 23, the WHO extended its SARS-related travel advice to Beijing and the Shanxi Province of China, recommending that persons planning to travel to these destinations consider postponing all but essential travel. Four days later, the Chinese Authorities closed theaters, Internet cafes, discos and other recreational activities and suspended the approval of marriages in an effort to prevent gatherings where SARS could be spread. To date, the epidemic in China seems to be under control. 5,327 cases of SARS have been diagnosed, 349 patients have died. On June 24, Beijing was removed from the list of areas with recent local transmission. 2.2.5 Taiwan The first two suspected SARS cases were diagnosed in a couple on March 14. The man had a history of travel in February to the Guangdong Province and to Hong Kong. On March 26, a Taiwanese resident of Hong Kong's Amoy Gardens flew to Taiwan and took a train to Taichung to celebrate the traditional festival, Qing Ming. The man's brother became Taiwan's first SARS fatality, and a fellow passenger on the train was also infected. Suddenly, in the last 10 days of April, the number of cases began to increase steadily, which would have made Taiwan's epidemic the third-worst in the world after China and Hong Kong. The origin of the outbreak was a laundry worker aged 42 years with diabetes mellitus and peripheral vascular disease who was employed at hospital A. On April 12, 14, and 15, he had a fever and diarrhea and was evaluated in the emergency department. The patient remained on duty and interacted frequently with patients, staff, and visitors. The patient had sleeping quarters in the hospital's basement and spent off-duty time socializing in the emergency department. On April 16, because of worsening symptoms, the patient was admitted to the hospital with a diagnosis of infectious enteritis. On April 18, the patient became short of breath. A chest radiograph showed bilateral infiltrates, and the patient was transferred to an isolation room in the intensive care unit with suspected SARS. Because the index patient had been symptomatic for 6 days before SARS was diagnosed, the number of potentially exposed persons was estimated at 10,000 patients and visitors and 930 staff. On April 24, hospital A was contained, and all patients, visitors, and staff were quarantined within the building. Healthcare worker clusters at eight additional hospitals in Taiwan have been linked to the initial outbreak at hospital A. Preliminary data suggest that many of these clusters 8 occurred when pre-symptomatic patients or patients with SARS symptoms attributed to other causes were discharged or transferred to other healthcare facilities. SARS later extended to multiple cities and regions of Taiwan, including several university and private hospitals. Four of these hospitals, including a 2,300-bed facility in southern Taiwan, discontinued emergency and routine services. Sporadic community cases also were reported in Taipei and southern Taiwan. The April outbreak in Taiwan may serve as an example of the far-reaching consequences of one single unrecognized SARS case. On July 5, Taiwan was removed from the list of areas with recent local transmission (WHO). 2.3 Worldwide The disease began spreading around the world along international air travel routes to Canada and other cities in the world (WHO. SARS: Status of the Outbreak) 2.3.1 Canada SARS was introduced to Toronto by a woman of Hong Kong descent who had traveled home to visit relatives from February 13 to February 23, 2003. Whilst visiting their son in Hong Kong, she and her husband stayed at Hotel M from February 18 until February 21, at the same time and on the same floor as the Guangdong physician from whom the international outbreak originated. The woman and her husband only stayed in the hotel at night, and spent the days visiting their son. They returned to their apartment in Toronto, which they shared with two other sons, a daughter-in-law and a five-month-old grandson on February 23, 2003. Two days later, the woman developed fever, anorexia, myalgia, a sore throat, and a mild non-productive cough. She died nine days after the onset of the illness. On March 8 and 9, five out of the six adult family members presented with symptoms of SARS. By mid-May, the Toronto epidemic was thought to be over after the initial outbreak had mostly come under control. However, an undiagnosed case at North York General Hospital led to a second outbreak among other patients, family members and healthcare workers.The new outbreak spread from the SARS ward on the eighth floor of North York General Hospital, where a 96 year old man undergoing surgery for a fractured pelvis on 19 April is believed to have 9 contracted the disease. The man developed pneumonia-like symptoms after his surgery but was not suspected of having SARS. He died on 1 May.A woman from the hospital's orthopedic ward, who was transferred to St John's Rehabilitation Hospital on 28 April, was later recognized as having a mild case of SARS, and five other SARS cases then appeared at St John's Hospital. The second Toronto outbreak demonstrates that spread among health care workers can occur despite knowledge about the epidemiology and transmission of SARS. SARS patients with chronic illnesses occurring concurrently with fever and/or pneumonia with a plausible diagnosis are extremely challenging to the public health and healthcare systems. On July 2, the WHO removed Toronto from its list of areas with recent local transmission. To date, 251 cases of SARS have been diagnosed in Canada, most of them in the Toronto area. 43 patients have died. 2.3.2 Other country Country Cumulative number case(s) of Number of deaths Case fatality ratio (%) Australia 6 0 0 Canada 251 43 17 China 5327 349 7 France 7 1 14 Germany 9 0 0 Hong Kong 1755 299 17 India 3 0 0 Indonesia 2 0 0 Italy 4 0 0 Kuwait 1 0 0 10 Macao 1 0 0 Malaysia 5 2 40 Mongolia 9 0 0 New Zealand 1 0 0 Philippines 14 2 14 Republic of Ireland 1 0 0 Republic of Korea 3 0 0 Romania 1 0 0 Russian Federation 1 0 0 Singapore 238 33 14 South Africa 1 1 100 Spain 1 0 0 Sweden 5 0 0 Switzerland 1 0 0 Taiwan 346 37 11 Thailand 9 2 22 United Kingdom 4 0 0 United States 29 0 9 Vietnam 63 5 8 Total 8098 774 9.6 11 “Table 2 .The official number of SARS cases reported from countries over the time period November 1, 2002 to July 31, 2003, is shown in the table. “Notes: The cumulative number of cases includes the number of deaths. 3.0 SIGN AND SYMPTOMS SARS or Severe Acute Respiratory Syndrome, is a contagious respiratory infection that presents a number of symptoms and signs. Signs and symptoms of SARS disease typically develop within two to 10 days after exposure to the virus. The SARS illness usually begins with a fever (measured temperature greater than 100.4°F [>38.0°C]). The fever is sometimes associated with fever, chills or other symptoms, including headache, dry coughing, general feeling of discomfort, and body aches. Less common symptoms are also possible and sometimes can be seen such as diarrhea, dizziness, nausea and vomiting. Some people also experience mild respiratory symptoms at the outset. In some patients, body aches and headaches may appear 12 to 24 hours before fever. Some people also have mild respiratory symptoms (sore throat or runny nose) at the outset. About 10 to 20 percent of patients with symptoms of SARS have diarrhea. After two to seven days, SARS patients may develop a dry cough and shortness of breath. These SARS symptoms may be accompanied by or progress to a condition in which the oxygen levels in the blood are low (hypoxia). In 10 to 20 percent of cases, patients require mechanical ventilation as they develop severe difficulty breathing, the result of insufficient oxygen in blood. Severe respiratory illness may occur before abnormalities are noted on chest X-ray. There might be radiographic (X-ray) findings of pneumonia or acute respiratory distress syndrome. Most people will recover within 1 to 2 weeks. SARS may be associated with other symptoms such as malaise, loss of appetite, confusion and sometimes even rash. For children and young infants, they might not follow the exact pattern that is seen in adults. Doctors should look for atypical symptoms in very young infants. 12 4.0 DIAGNOSIS AND INTERVENTION 4.1 Diagnosis Before the actual case of SARS can be ascertained, all diagnoses are based primarily on clinical symptoms and using laboratory test results as a secondary basis. SARS can also be diagnosed based on the history of recent travel to high risk areas or history of close contacts with person with SARS and also by chest x-ray. The symptoms of SARS are high fever, shivering, cough, extreme lethargy, muscle aches, flu symptoms, diarrhea and general malaise. Table 1 - Clinical symptoms at presentation (in %) Lee et al. Peiris et Donnelly et Booth et n=138 al. al. al. n=50 n > 1250 n=144 100 94 99 or 73 74 65* 28* Cough 57 62 50 69 Myalgia 61 54 51 49 Malaise n.a. 50 64 31 Runny nose 23 24 25 2 Sore throat 23. 20 23 12 Shortness of n.a. 20 31 n.a. Fever Chills 100 rigors breath Diarrhea 20 10 27 24 Headache 56 20 50 35 13 *chills Scientists from the Chinese University of Hong Kong and the Prince of Wales Hospital have pinpointed the cause of this mysterious respiratory illness to that of viral origin. By examining extracted tissue samples from SARS infected patients and analyzing them, the virus was initially believed to belong to the paramyxoviridae family. However, further studies showed that it is more likely to be a type of coronavirus. The researchers estimate the incubation period of the virus to be between three to seven days. This has prompted authorities to impose “10-day quarantines” for suspected cases. During the course of illness, abnormal hematological values are common. Early studies have shown lymphopenia and thrombocytopenia to be frequent in SARS patients. There is now one study which analyzed the hematological changes during SARS in more detail. Progressive lymphopenia was found in the peripheral blood of 153/157 (98 %) patients with SARS, reaching its lowest point in the second week. Lymphopenia was also shown in hemato-lymphoid organs at postmortem examination. The lymphocyte count commonly recovered in the third week, but about 30% of patients were still lymphopenic by the fifth week of SARS. Most patients had reduced CD4 and CD8 T cell counts during the early phase of illness, with mean CD4 and CD8 T cell counts of 287 cells/µl (normal: 410 to 1590 cells/µl) and 242 cells/µl (normal: 62 to 559 cells/µl), respectively. Low CD4 and CD8 lymphocyte counts at presentation were associated with an adverse outcome in this study. Transient leucopenia was found in 64% of patients during their first week of illness. However, during the second and third week of illness, 61% developed leucocytosis. Neutrophilia (> 7.500/µl) developed in 82% of patients, possibly reflecting the wide use of corticosteroids. In total, 55% of patients developed a self-limiting thrombocytopenia, possibly caused by an immune mechanism. With the exception of 2% of patients, the degree of thrombocytopenia was mild (platelet counts >50.000/µl), reaching a low point at the end of the first week. No patient had major bleeding or required platelet transfusion. For the laboratory findings, common electrolyte and biochemical abnormalities include elevated levels of lactate dehydrogenase (LDH), aspartate and alanine aminotransferases and creatine kinase are usually obtained. (Table 2) Since high lactate dehydrogenase levels are often 14 seen in association with tissue damage, some authors propose that this finding indicates extensive lung injury. However, it seems possible that elevated levels of lactate dehydrogenase and transaminases may be, at least partially, secondary to the hemolytic effect of ribavirin treatment. In a multivariate analysis, elevated LDH was an independent predictor for poor outcome in SARS patients. A substantial proportion of patients demonstrate low calcium, phosphorus, magnesium, sodium and potassium levels. These abnormalities tend to worsen during hospitalization. Again, it remains unclear whether these changes reflect the natural course of the infection or whether they are secondary to the effects of treatment with ribavirin or other agents that affect renal tubular function. There is evidence that the clotting profile (prothrombin time, activated partialthromboplastin time, international normalized ratio, and D-dimer) may be deranged in a substantial number of patients. Table 2 - Laboratory findings at presentation (in %) Lee, n=138 Leukopenia (< 3.5 x 34 et al. Peiris, n=50 26 109/l) Lymphopenia (< 1.0 x 70 68 109/l) Thrombocytopenia 45 40 Alanine 23 34 32 26 aminotransferase Ý Creatine kinase Ý 15 et al. LDH Ý 71 n.a. Hyponatremia 20 n.a. Hypokalemia 25 n.a. D-dimer levels Ý 45 n.a. activated 43 n.a. Prolonged partial-thromboplastin time n.a. = not available. The new coronavirus was isolated in Vero E6 cells from nasal and throat swab specimens of two patients in Thailand and Hong Kong with suspected SARS. The isolate was identified by electron microscopy (EM). The identification was corroborated by results of immunostaining, indirect immunofluorescence antibody (IFA) assays, and reverse transcriptase-polymerase chain reaction (RT-PCR) with sequencing of a segment of the polymerase gene. Coronavirus particles were also identified by EM in cells obtained by bronchial lavage from a patient with SARS. In order to prove beyond doubt that a candidate virus is causing SARS, “gold-standard” tests will be needed. One such test is the enzyme-linked immunosorbent assay (ELISA), which can detect antibodies produced by the patient’s immune system to fight a particular virus. The diagnosis of SARS can be done by PCR testing, Seroconversion by ELISA or IFA and virus isolation. 16 4.1.1 PCR testing For PCR testing, there are at least 2 different clinical specimens needed for example from the nasopharyngeal and stool. Besides that, there can also be the same clinical specimen collected on 2 or more days during the course of the illness for example 2 or more nasopharyngeal aspirates are obtained for diagnosis The peak detection rate for SARS-associated coronavirus occurred at week 2 after illness onset for respiratory specimens, at weeks 2 to 3 for stool or rectal swab specimens, and at week 4 for urine specimens. The latest stool sample that was positive by reverse transcriptionpolymerase chain reaction was collected on day 75 while the patient was receiving intensive care. Tracheal aspirate and stool samples had a higher diagnostic yield (RT-PCR average positive rate for first 2 weeks: 66.7% and 56.5%, respectively). Pooled throat and nasal swabs, rectal swab, nasal swab, throat swab, and nasopharyngeal aspirate specimens provided a moderate yield (29.7%-40.0%), whereas throat washing and urine specimens showed a lower yield (17.3% and 4.5%). The collection procedures for stool and pooled nasal and throat swab specimens were the least likely to transmit infection, and the combination gave the highest yield for coronavirus detection by RT-PCR. . If a positive PCR result has been obtained, it should be confirmed by repeating the PCR using the original sample or having the same sample tested in a second laboratory. Amplifying a second genome region could further increase test specificity. Clinicians should save any available clinical specimens (respiratory, blood, and serum) for additional testing until a specific diagnosis is made. Acute and convalescent (greater than 21 days after the onset of symptoms) serum samples should be collected from each patient who meets the definition criteria for SARS. Specific instructions for collecting suspected patients infected with SARS are needed. 17 4.1.1a Collecting Respiratory Specimens Eight types of respiratory specimens may be collected for viral and/or bacterial diagnostics: 1) Nasopharyngeal wash or aspirates 2) Nasopharyngeal swabs 3) Oropharyngeal swabs 4) Broncheoalveolar lavage 5) Tracheal aspirate 6) Pleural fluid taps 7) Sputum 8) Post-mortem tissue. Nasopharyngeal wash/aspirates are the specimen of choice for detection of most respiratory viruses and are the preferred specimen type for children under age 2 years. In contrast to most respiratory pathogens for which respiratory specimens are optimally collected within 72 hours after the onset of symptoms, levels of SARS-CoV may be higher later in the course of the illness. i) Collecting specimens from the upper respiratory tract Nasopharyngeal aspirates or swabs. Have the patient sit with head tilted slightly backward. Instill 1 ml-1.5 ml of non bacteriostatic saline (pH 7.0) into one nostril. Flush a plastic catheter or tubing with 2 ml-3 ml of saline. Insert the tubing into the nostril parallel to the palate. Aspirate nasopharyngeal secretions. Repeat this procedure for the other nostril. Collect the specimens in sterile vials. Label each specimen container with the patient’s ID number 18 and the date collected. If shipping domestically, use cold packs to keep the sample at 4°C. If shipping internationally, pack in dry ice. Nasopharyngeal or oropharyngeal swabs Use only sterile dacron or rayon swabs with plastic shafts. Do not use calcium alginate swabs or swabs with wooden sticks, as they may contain substances that inactivate some viruses and inhibit PCR testing. Nasopharyngeal swabs -- Insert a swab into the nostril parallel to the palate. Leave the swab in place for a few seconds to absorb secretions. Swab both nostrils. Oropharyngeal swabs -- Swab the posterior pharynx and tonsillar areas, avoiding the tongue. Place the swabs immediately into sterile vials containing 2 ml of viral transport media. Break the applicator sticks off near the tip to permit tightening of the cap. Label each specimen container with the patient’s ID number and the date the sample was collected. If shipping domestically, use cold packs to keep sample at 4°C. If shipping internationally, pack in dry ice. ii) Collecting specimens from the lower respiratory tract Broncheoalveolar lavage, tracheal aspirate, pleural fluid tap Centrifuge half of the specimen, and fix the cell pellet in formalin. Place the remaining unspun fluid in sterile vials with external caps and internal O-ring seals. If there is no internal O-ring seal, then seal tightly with the available cap and secure with Parafilm®. Label each specimen container with the patient’s ID number and the date the sample was collected. If shipping domestically, use cold packs to keep sample at 4°C. If shipping internationally, ship fixed cells at room temperature and unfixed cells frozen. Sputum 19 Educate the patient about the difference between sputum and oral secretions. Have the patient rinse the mouth with water and then expectorate deep cough sputum directly into a sterile screw-cap sputum collection cup or sterile dry container.If shipping domestically, use cold packs to keep sample at 4°C. If shipping internationally, pack in dry ice. 4.1.1b Collecting Blood Components Serum and blood (plasma) should be collected early in the illness for RT-PCR testing. The reliability of RT-PCR testing performed on blood specimens decreases as the illness progresses. Both acute and convalescent serum specimens should be collected for antibody testing. To confirm or rule out SARS-CoV infection, it is important to collect convalescent serum specimens >28 days after the onset of illness. A. Collecting serum for antibody or RT-PCR testing Collect 5 ml-10 ml of whole blood in a serum separator tube. Allow the blood to clot, centrifuge briefly, and collect all resulting sera in vials with external caps and internal O-ring seals. If there is no internal O-ring seal, then seal tightly with the available cap and secure with Parafilm ®. The minimum amount of serum preferred for each test is 200 micro liters, which can easily be obtained from 5 mL of whole blood. A minimum of 1 cc of whole blood is needed for testing of pediatric patients. If possible, collect 1 cc in an EDTA tube and in a clotting tube. If only 1cc can be obtained, use a clotting tube. Label each specimen container with the patient’s ID number and the date the specimen was collected. If unfrozen and transported domestically, ship with cold packs to keep the sample at 4°C. If frozen or transported internationally, ship on dry ice. B. Collecting EDTA blood (plasma) for RT-PCR 20 Collect 5 ml-10 ml of blood in an EDTA (purple-top) tube. Transfer to vials with external caps and internal O-ring seals. If there is no internal O-ring seal, then seal tightly with the available cap and secure with Parafilm®. Label each specimen container with patient’s ID number and date of collection. Store and ship blood specimens with cold packs to keep the sample at 4°C. 4.1.1c Collecting Stool Specimens for PCR Begin collecting stool specimens as soon as possible in the course of the illness. Although collecting earlier specimens is ideal, SARS-CoV has been detected in stool as late as one month after the onset of symptoms. Place each stool specimen -- as large a quantity as can be obtained (at least 10 cc) -- in a leak-proof, clean, dry container, and refrigerate at 4°C. Patients may drape plastic kitchen wrap across the back half of the toilet, under the toilet seat, to facilitate collection of stool specimens. IMPORTANT: Refrigerate or freeze tubes after specimens are placed in them. If specimens will be examined within 48 hours after collection, they can be refrigerated. If specimens must be held longer than 48 hours, freeze them as soon as possible after collection. Although storage in an ultra-low freezer (-70°C) is preferable, storage in a home-type freezer (if properly set at 20°C) is acceptable for short periods. 4.1.2 Seroconversion by ELISA or IFA: ELISA or IFA is a negative antibody test on acute serum followed by positive antibody test on convalescent serum. Antibodies against SARS-CoV become detectable with high sensitivity around 10 days after the onset of infection, but they can be undetectable prior to this by current testing methods. Positive antibody test results indicate that there has been an infection with SARS-CoV. Seroconversion from negative to positive, or a four-fold rise in antibody titre in the serum of a convalescent patient compared with that patient’s serum during acute illness, denotes a recent infection. A negative serological result 21 days after onset of symptoms indicates absence of 21 SARS-CoV infection. Cross-reactions with antibodies to other agents (including the human coronaviruses HCoV-229E and HCoV-OC43) are not known. Several serological studies with SARS patient sera have been reported and these show varying sensitivities and specificities. Serological studies with SARS patient sera using immunofluorescence tests (IIFT) or ELISA showed sensitivities between 92 and 99%. The reference serological method is the neutralization test and this was compared to enzyme linked immunosorbent assay (ELISA), immunofluorescence assays (IFA) and the immunochromatic test (ICT). Antibody determination using IFA or ELISA was the most reliable method for identifying infections with SARS-CoV. The ICT had a poor sensitivity. 4.1.3 Virus isolation Patient specimens such as respiratory secretions, blood, or stool can be inoculated in suitable cell lines for growth of the infectious agent. Cell culture requires considerable expertise, is time consuming and quite demanding. Vero cells have been used for culture. After isolation, the virus has to be confirmed and this is usually done with nucleic acid based tests. Positive results indicate presence of viable SARSCoV, whilst negative cell culture results do not exclude SARS. These viruses were originally isolated in organ cultures of human embryonic trachea and subsequently grown in tissue culture in fibroblasts. Although most coronaviruses are highly species specific, under certain experimental conditions some human strains may infect different species though, for example, intra-cerebral inoculation of African green monkeys. Serial passaging in heterologous cell lines can extend the host range. This leads to the virus being able to employ a larger variety of receptors on the cell surface. Coronaviruses show a marked degree of tissue tropism. Closely related viruses may show different tropism, some tending towards respiratory infections and others to gastrointestinal infections. These tropisms are influenced by both host cell surface characteristics and by viral Sglycoprotein variation. Although coronaviruses replicate in the cytoplasm the role of the nucleus 22 in this respect is unknown. Coronaviruses usually cause lytic infections although persistent infections are also known to occur depending on the particular virus strain and host cell. 4.1.4 Imaging Imaging plays an important role in the diagnosis of SARS and monitoring of response to therapy. A predominant peripheral location, a progression pattern from unilateral focal air-space opacity to unilateral multifocal or bilateral involvement during treatment, and lack of cavitation, lymphadenopathy, and pleural effusion are the more distinctive radiographic findings (Wong 2003b). At the onset of fever, 70-80 % of the patients have abnormal chest radiographs (Booth, Wong 2003b, Peiris 2003b). It should be noted that, in a substantial proportion of cases, chest radiographs may be normal during the febrile prodrome, as well as throughout the course of illness. In other cases, radiological evidence of pneumonic changes may precede the fever (Rainer), particularly in individuals with co-morbidities who may be impaired in their ability to mount a fever (Fisher 2003a). Chest X-ray findings typically begin with a small, unilateral, patchy shadowing, and progress over 1-2 days to become bilateral and generalized, with interstitial or confluent infiltrates. Air-space opacities eventually develop during the course of the disease. In patients who deteriorate clinically, the air-space opacities may increase in size, extent, and severity (Tsang, Lee). In the first large cohort from Hong Kong, 55 % of the patients had unilateral focal involvement and 45 % had either unilateral multi-focal or bilateral involvement at the onset of fever (Lee). Within a prospective cohort, initial involvement was confined to one lung zone in 49% and was multi-zonal in 21% of the patients (Peiris 2003b). The initial radiographic changes may be indistinguishable from those associated with other causes of bronchopneumonia. The research group from Hong Kong suggested that chest radiographs might offer important diagnostic clues, in particular when, after approximately one 23 week, unilateral, predominantly peripheral areas of consolidation progress to bilateral patchy consolidation, and when the extent of the lung opacities is correlated with the deterioration in respiratory function (Lee). There seems to be a predominant involvement of the peripheral-zone. Pleural effusions, cavitation, and hilar lymphadenopathy are usually absent. Respiratory symptoms and positive auscultatory findings are disproportionally mild compared with the chest radiographic findings (Lee). One large study focused on radiographic appearances and the pattern of progression (Wong 2003b). Within this cohort of 138 patients, four patterns of radiographic progression were recognized: type 1 (initial radiographic deterioration to a peak level, followed by radiographic improvement) in 70.3%, type 2 (fluctuating radiographic changes) in 17.4%, type 3 (static radiographic appearance) in 7.3%, and type 4 (progressive radiographic deterioration) in 5.1% of the patients. Findings during deterioration are compatible with the radiological features of acute respiratory distress syndrome. The predominant abnormalities found on initial CT scans are areas of sub-pleural focal consolidation with air bronchograms and ground-glass opacities (Tsang). The lower lobes are preferentially affected, especially in the early stages. Patients with more advanced cases show a more bilateral involvement (Wong 2003a). The lesions tend to be peripheral and smaller in the less severely affected lungs, also suggesting an earlier stage of the disease. In patients with more advanced cases, there is involvement of the central, perihilar regions by larger (>3 cm) lesions. The majority of the lesions contained an area of ground-glass opacification with or without consolidation. Other findings include intralobular thickening, interlobular septal thickening, a crazy-paving pattern, and bronchiectasis (Wong 2003a). Obvious bronchial dilatation is generally not found (Lee). Radiographically, SARS may be indistinguishable from other severe forms of pneumonia. It also shares CT features with other conditions that result in subpleural air-space disease, such as the pneumonia of bronchiolitis obliterans and acute interstitial pneumonia (Tsang). 24 Radiologists from the Prince of Wales Hospital, Hong Kong, recommend the following protocol for diagnostic imaging of suspected SARS patients (Wong 2003a): Patients with symptoms and signs consistent with SARS and with abnormalities on chest radiographs are followed up with serial radiography. CT scanning is not required for diagnosis. Patients with symptoms and signs consistent with SARS and with a normal chest radiograph undergo thin-section CT to confirm the diagnosis. They subsequently undergo serial radiography for follow-up. Identifying hospitalized patients with SARS is difficult, especially when no epidemiological link has been recognized and the presentation of symptoms is non-specific. Patients with SARS might develop symptoms common to hospitalized patients (e.g., fever or prodromal symptoms of headache, malaise, and myalgia), and diagnostic testing to detect cases is limited (MMWR 52: 547-50). Unless specific laboratory tests (PCR, detection of SARS antibodies; see Chapter 7: Diagnostic Tests) confirm the initial suspicion of SARS infection, the diagnosis of SARS is based on the clinical findings of an atypical pneumonia not attributed to any other cause, as well as a history of exposure to a suspect or probable case of SARS, or to their respiratory secretions or other body fluids. As mentioned above, during the early stages, SARS may be difficult to differentiate from other viral infections, especially when symptoms are unspecific (Rainer). The initial diagnostic testing for suspected SARS patients should include chest radiography, pulse oximetry, bacterial cultures of blood, sputum, and urine, serology for mycoplasma, chlamydia, influenza, parainfluenza, respiratory syncytial and adenoviruses, nasopharyngeal aspirates for viral cell cultures, and direct sputum smear for Pneumocystis jiroveci by silver stain. A specimen for Legionella and pneumococcal urinary antigen testing should also be considered. The radiographic appearance of peripheral air-space opacities is indistinguishable from other causes of atypical pneumonia, such as Mycoplasma, Chlamydia, and Legionella, and overlaps with other types of viral pneumonia. The presence of air-space opacity on chest radiographs has been helpful in the confirmation of the diagnosis (Wong 2003b). 25 4.2 Intervention The 2003 outbreak of severe acute respiratory syndrome (SARS) was contained largely through traditional public health interventions, such as finding and isolating case-patients, quarantining close contacts, and enhanced infection control. The independent effectiveness of measures to "increase social distance" and wearing masks in public places requires further evaluation. Limited data exist on the effectiveness of providing health information to travelers. Entry screening of travelers through health declarations or thermal scanning at international borders had little documented effect on detecting SARS cases; exit screening appeared slightly more effective. The value of border screening in deterring travel by ill persons and in building public confidence remains unquantified. Interventions to control global epidemics should be based on expert advice from the World Health Organization and national authorities. In the case of SARS, interventions at a country's borders should not detract from efforts to identify and isolate infected persons within the country, monitor or quarantine their contacts, and strengthen infection control in healthcare settings. A variety of intervention measures exist to prevent and control diseases with pandemic potential like SARS or pandemic influenza. They differ in their approach and effectiveness in reducing the number of cases getting infected. The effects of different intervention measures were investigated by a mathematical modelling approach, with comparisons based on the effective reproduction number (Re). The analysis showed that early case detection followed by strict isolation could control a SARS outbreak. Tracing close contacts of cases and contacts of exposed health care workers additionally reduces the Re. Tracing casual contacts and measures aiming to decrease social interaction were less effective in reducing the number of SARS cases. The study emphasizes the importance of early identification and isolation of SARS cases to reduce the number of people getting infected. However, doing so transfers cases to health care facilities, making infection control measures in hospitals essential to avoid nosocomial spread. The modelling approach applied in this study is useful for analysing interactions of different intervention measures for reducing the Re of SARS. 5.0 TREATMENT 26 Treatment for SARS is prescribed as the same line as for any other unknown form of atypical pneumonia and largely involves provision of ventilator support, anti-pyretics, and supplemental oxygen. The first development treatment strategies for SARS were based on theoretical, from clinical observations and inferences. Prospective randomized controlled treatment trials were understandably lacking during the first epidemic of this disease. The mainstream therapeutic interventions for SARS involve broad-spectrum antibiotics and supportive care, as well as antiviral agents and immunomodulatory therapy. 5.1 Antibiotic therapy Rapid laboratory tests that can be used to diagnose the SARS-CoV virus in the first few days of infection are not yet available. Anti-bacterial agents are routinely prescribed for SARS because it has non-specific features. Appropriate empirical antibiotics are needed to cover against common respiratory pathogens as per national or local treatment guidelines for community-acquired or nosocomial pneumonia. Some antibiotics are known to have immunomodulatory properties, in addition to their antibacterial effects. For example, quinolones and macrolides. Their effect on is still undetermined. 5.2 Antiviral therapy Scientific institutions worldwide have been vigorously identifying or developing an efficacious antiviral agent with the discovery of the SARS-CoV as the etiologic agent. Intensive in vitro susceptibility tests are underway. 5.2.1 Ribavirin Ribavirin is a nucleoside analogue which was widely chosen as an empirical therapy for SARS because it has broad-spectrum antiviral activity against many DNA and RNA viruses. It has since become the most frequently administered antiviral agent for SARS and it was commonly used with corticosteroids. The use of ribavirin has caused a lot of criticism due to its unproven efficacy and undue of side effect. Ribavirin has no direct in vitro activity against SARS-CoV at non-toxic concentration. Based on clinical experience, including quantitative reverse transcriptase polymerase chain reaction (RT-PCR) monitoring the nasopharyngeal viral load, has also not been able to suggest any substantial in vivo antiviral effect from this drug. 27 The prevalence of side effects from this drug is dose-related. High doses often have more adverse effects. For example, hemolytic anemia, elevated transaminase levels and bradycardia. Lower doses of ribavirin did not show clinically significant adverse effects. In elderly, side effects have also been observed frequently. 5.2.2 Neuraminidase inhibitor Oseltamivir phosphate, neuraminidase inhibitor used for treatment of both influenza A and B viruses. There is no evidence that neuraminidase inhibitor has any efficacy against SARS-CoV. So it is normally not a recommended treatment apart from in its role as an empirical therapy to cover possible influenza. 5.2.3 Protease inhibitor Lopinavir-ritonavir co-formulation, a protease inhibitor preparation which is used to treat human immunodeficiency virus (HIV) infection. Protease inhibitor has been used in combination with ribavirin in several Hong Kong hospitals, which is hope it can inhibit the coronaviral proteases, then blocking the processing of the viral replicase polyprotein and preventing the replication of viral RNA. Preliminary results show that the addition of lopinavir-ritonavir to the contemporary use of ribavirin and corticosteroids, especially when administered early might reduce intubation and mortality rates. 5.2.4 Human interferons Interferons, a family of cytokines which is important in the cellular immune response. They are classified into two types. Type I (interferon α and β, sharing components of the same receptor) and type II (interferon γ which binds to a separate receptor system) which have different antiviral potentials and immunomodulatory activities. As reported from China and Canada, the use of interferons in the treatment of SARS are limited to interferons α. In the small Canadian series using interferon alfacon-1, faster recovery was observed. It is also known as consensus interferon, which shares 88% homology with interferon α -2b and about 30% homology with interferon β . In Germany, In vitro testing of recombinant interferons against SARS-CoV was recently carried out using interferon α -2b, interferon β -1b and 28 interferon γ -1b. Interferon β was found to be far more potent than interferon α or γ , and it remained effective even after viral infection. Interferon α selectivity index was 50-90 times lower than that of interferon β, although it can effectively inhibit SARS-CoV replication in cell cultures. These in vitro results show that interferon β is promising and can be used in future treatment trials. 5.2.5 Human immunoglobulin It was used in some hospitals in China and Hong Kong. An IgM-enriched immunoglobulin product was tried in selected SARS patients. However, their effectiveness in SARS remains uncertain as there was often concomitant use of other therapies such as corticosteroids. An experimental treatment tried in Hong Kong which is convalescent plasma is collected from recovered patients. Neutralizing immunoglobulins in convalescent plasma were believed can curb increases in the viral load. 5.2.6 Alternative medicine Traditional herbal medicine has been frequently used in conjunction with Western medicine to treat SARS, and is believed to be effective which is used in China. Glycyrrhizin, an active component derived from liquorice roots, was tested against SARS-CoV in vitro. Before this, it has been used in the treatment of HIV and hepatitis C virus infections, and was found to be relatively non-toxic with infrequent side effects, for example, hypertension and hypokalemia. It can inhibit the adsorption, penetration and replication of SARS-CoV in Vero cell cultures and was most effective when administered both during and after viral adsorption. But glycyrrhizin can only act against SARS-CoV at very high concentrations, so its clinical dosing and utility remain uncertain. Perhaps it can be explored as an adjunct therapy for SARS, or continued as an ingredient or base in herbal preparations. 5.6 Immunomodulatory therapy Acute infections in general can stimulate the release of proinflammatory cytokines. There may be an excessive host response or cytokine dysregulation in SARS. Clinical deterioration can paradoxically occur despite a fall in the viral load as IgG seroconversion takes place as well as from autopsy findings which demonstrate a prominent increase in alveolar macrophages with 29 hemophagocytosis. A tri-phasic model of pathogenesis was proposed comprising viral replicative, immune hyperactive and pulmonary destructive phase. Immunomodulatory is carefully applied during the hyper-immune phase can be an important treatment component in SARS. 5.6.1 Corticosteroids As described in many Chinese and Hong Kong reports, corticosteroids timely used often led to early improvement in terms of subsidence of fever, radiographic infiltrates resolution and better oxygenation. However, based on their effectiveness, adverse immunosuppressive effects and impact on final patient outcomes, there are a lot of skepticism and controversy about the use of this substance. Corticosteroids showed no benefits at an early Singaporean report on five patients on mechanical ventilation. It concluded that two-thirds progressed after early use of ribavirin and corticosteroids, but only about half of these subsequently responded to pulsed doses of methylprednisolone from a retrospective series of over 320 patients from a regional hospital in Hong Kong. 80% of patients had recurrence of fever and radiological worsening in a cohort study. The inconsistencies of treatment outcomes in SARS (or other illnesses) could be due to differences in the dosing, timing and duration of corticosteroid use. The following points have been emphasized : Use of corticosteroids too early may theoretically prolong the viral replicative phase and increase the viral burden, whereas delayed administration may not be able to halt the cytokine storm and can prevent immunopathological lung damage. It supposed to be adjusted based on individual body weight and disease severity. Adequate duration of corticosteroids is needed to maintain the optimized immune balance. Too short may result in a rebound of cytokine storm with lung damage, whereas protracted usage will cause the patient is at risk of various corticosteroid complications. Corticosteroids is beneficial but it has its own risk. It is not only facilitates coronaviral replication in the absence of an effective antiviral agent, but also can invites bacterial sepsis and opportunistic infections. A SARS patient who died from systemic fungal infection have been reported. 30 If the patient remains clinically stable, it is likely that an optimal immune balance has been reached. Moreover, most radiological infiltrates will resolve gradually on a diminishing course of corticosteroids over 2-3 weeks. Differentiate Radiographic abnormalities arising from a superimposed bacterial pneumonia from the progressive immunopathological lung damage of SARS, would result in adding further corticosteroids. Other immunomodulator that can be use is Thymosin alpha 1.In some Chinese hospitals, Thymosin alpha 1 is used in the treatment of chronic viral hepatitis B and C, and has also been administered to SARS patients. It is a safe product and may augment T-cell function. The role and effectiveness in SARS has not yet been determined. Tumor necrosis factor blocking agents, namely etanercept and infliximab and some other compounds like cyclophosphamide, azathioprine, cyclosporin and thalidomide are other immunomodulatory agents in anecdotal use. 5.6.2 Assisted ventilation Some SARS patients still develop acute hypoxemic respiratory failure. 20-30% of SARS warranted admission into intensive care units, and 10-20% eventually required intubation and mechanical ventilation according to the current literature. 5.6.2a Non invasive ventilation Non invasive ventilation is a valuable treatment for acute respiratory failure of various causes, and can avoid complications related to intubation and invasive ventilation. Its application in SARS may be of particular benefit since patients are normally treated with high dose corticosteroids, which exposed them to infections including ventilator-associated pneumonia. It was commonly employed in many Chinese and Hong Kong hospitals. It can improve oxygenation and tachypnea within an hour, and it can help to prevent adding further corticosteroids for respiratory failure. Generally, it was found to be able to avoid intubation and invasive ventilation in up to two-thirds of SARS patients with deterioration. In contrast, the scenarios for non-SARS-related acute respiratory distress syndrome, higher pressures were generally not necessary and should be avoided whenever possible, because 31 not only was there usually no additional clinical improvement observed, but it can also add to the risk of pneumothorax and pneumomediastinum. Although it can improved patient outcome, the infective risks associated related to aerosol generation have decreased its use in many hospitals. 5.6.2b Invasive ventilation SARS-related respiratory failure patients who continue to deteriorate while on non invasive ventilation, or in whom non invasive ventilation is contraindicated, supposed to be promptly intubated and mechanically ventilated. The actual endotracheal intubation procedure can cause a high infective risk and healthcare workers must strictly adhere to all infection control measures. The procedure is best performed by highly skilled personnel using rapid sequence induction to minimize the risk. It has been recommended to use other approaches like a "modified awake" intubation technique and elective intubation upon recognizing signs of imminent need for airway management. Ventilation method and settings with reference to the strategies for acute respiratory distress syndrome (ARDS) are used by most centers. The pressure and volume control ventilation can be employed. The tidal volume should be maintained low at 5-6 ml per Kg of the predicted body weight, and plateau pressures are maintained less than 30 cm H2O. Adequate sedation should be applied to ventilated patients and a short-term neuromuscular blockade might required for permissive hypercapnia mechanically. 6.0 Control of SARS Prevention and control measures were initiated by the Ministry Of Health(MOH) SARS Task Force, which was formed on 15 March 2003 and chaired by the Director of medical service(DMS). Its members included the chief executive officers of all hospitals, chairmen of medical boards, infectious disease physicians, epidemiologists and virologists. Strategies to contain the rapid nosocomial transmission were discussed, formulated and effectively implemented across all healthcare institutions through the Infectious Diseases Act and Private Hospitals and Medical Clinics Act. The Ministerial Committee on SARS (chaired by the Minister for Home Affairs) was established on 7 April to provide political guidance and quick strategic decisions to minimise the 32 socioeconomic impact of SARS. The Executive Group, comprising permanent secretaries of the relevant ministries, was responsible for the overall coordination and implementation of multiagency issues outside the healthcare setting, while an Inter-Ministry SARS Operations Committee ensured that cross-ministry operational issues on SARS were well coordinated. A Ministerial SARS Combat Unit was also appointed on 20 April; 3 of its members were medical doctors. It worked closely with the public and private hospitals and other healthcare institutions to prevent and control SARS transmission in these facilities. Key measures implemented were directed at the prevention and control of SARS in the community, healthcare institutions and the borders. Community In the prevention and control of SARS within the community, the key strategy was to detect persons with suspected or probable SARS as early as possible and isolate them in. At the same time, the Infectious Diseases Act was reviewed and amended to ensure that all necessary public health measures could be taken to control the outbreak; e.g., handling and disposal of bodies due to SARS within 24 hours of death. Early identification of SARS cases was done through several ways, including active contact tracing for all contacts within 24 hours of notification of a case, mandatory home quarantine enforced through the use of electronic cameras, and intensive education of healthcare professionals and the public. To allay the concern of parents, all preschools, primary and secondary schools were closed for 2 to 3 weeks at the end of March to early and mid-April 2003. Healthcare Institutions The MOH implemented very stringent infection control procedures to prevent and contain outbreaks in hospitals, nursing homes and other healthcare institutions. At the first point of contact with healthcare facilities [accident and emergency (A&E) departments, specialists outpatient clinics], triage was carried out to separate out febrile patients. To widen the surveillance net, the WHO’s definition for suspected and probable SARS was expanded to include any HCW with fever and/or respiratory symptoms (particularly in a cluster of 3 or more febrile cases), inpatients (>16 years old) with atypical pneumonia under investigation, sudden unexplained deaths with respiratory symptoms, and in patients with fever (>38 o C) of more than 72 hours and with relevant travel history but without known causes. Case finding was further intensified with the introduction of thrice-daily temperature surveillance of all health care worker (HCW)s in every institution and active surveillance for cluster of febrile 33 person especially , among the immunocompromised, who tend to have atypical clinical presentations, and staff from the same work area. Sick leave of HCWs was centrally monitored. Audits were periodically conducted to ensure that the directives and guidelines issued by the MOH were strictly enforced. Strict enforcement of the proper use of personal protective equipment (PPE) (test-fitted N95 mask, gowns, gloves and goggles/protective eye gear if managing suspicious cases, and powered air purified respirator for high-risk procedures such as intubation), control of visitors, restriction of movements of health care workers s (including confining their practice to one institution) and patients (readmission to the same hospital within 21 days after discharge), and close monitoring of discharged patients from SARS-affected wards. In addition to issuing a health alert advising travellers to avoid SARS-affected countries, unless absolutely necessary, MOH took various measures to minimize the risk of imported case. These measures were implemented in phases. Health alert notices were issued at the airport to inbound air passengers from SARS-affected countries to highlight the signs and symptoms of SARS and the need to seek immediate attention if fever developed. Health screening of all incoming air and sea passengers and crew from affected areas was carried out through temperature checks using thermal imaging scanners. Travellers picked up by the scanners had their temperature re-checked by nurses who would refer them for further examination by doctors at the air and sea terminals if they were confirmed to have a fever. Those who were suspected of having SARS were sent to hospital for further assessment and admission for isolation and treatment if necessary. Incoming bus passengers at the land checkpoints were also screened with the thermal scanners. Screening was progressively extended to travellers coming in via other vehicles at the land checkpoints. All visitors through air, sea and land checkpoints were required to complete a SARS health declaration card to facilitate contact tracing. However, not a single case of SARS was detected through these measures. Very stringent steps were taken to minimise the possibility of exporting cases to other countries. These measures included the rapid containment of outbreaks, and mandatory temperature screening of all outgoing travellers. In addition, special bilateral arrangements on the exchange of information necessary to conduct contact tracing and quarantine was set up with Malaysia and Indonesia. 34 7.0 EXAMPLE OF SARS CASES 7.1 SARS OURBREAK IN CHINA Beijing, China, experienced the largest outbreak of SARS in the world with a total of 2,521 reported probable cases, according to background information in the article. The outbreak began March 5, 2003, with the importation of several cases among travelers from other SARS-affected areas and soon accelerated as multiple SARS cases occurred in health care facilities, peaking in late April when more than 100 new patients with SARS were being hospitalized daily. During the first week of May, the number of new cases dropped steeply and then declined steadily during the next few weeks, with the onset of the last probable case on May 29, 2003. The onset of the last case occurred only 6 weeks after the peak of the outbreak. Xinghuo Pang, M.D., of the Beijing Center for Disease Prevention and Control, and colleagues evaluated the measures taken to rapidly control the SARS outbreak in Beijing and assess the effectiveness of some of these measures. The researchers reviewed data from standardized surveillance forms from SARS cases (2,521 probable cases) and their close contacts observed in Beijing between March 5, 2003, and May 29, 2003. Procedures implemented by health authorities were investigated through review of official documents and discussions with public health officials. The researchers found that healthcare worker training in use of personal protective equipment and management of patients with SARS and establishing fever clinics and designated SARS wards in hospitals predated the steepest decline in cases. During the outbreak, 30,178 persons were quarantined. Among 2,195 quarantined close contacts in 5 districts, the attack rate was 6.3 percent, with a range of 15.4 percent among spouses to 0.36 percent among work and school contacts. The attack rate among quarantined household members increased with age from 5.0 percent in children younger than 10 years to 27.6 percent in adults aged 60 to 69 years. Among almost 14 35 million people screened for fever at the airport, train stations, and roadside checkpoints, only 12 were found to have probable SARS. The national and municipal governments held 13 press conferences about SARS. The time lag between illness onset and hospitalization decreased from a median of 5 to 6 days on or before April 20, 2003, the day the outbreak was announced to the public, to 2 days after April 20. 7.2 SARS OURBREAK IN SINGAPORE The SARS outbreak entered Singapore through three young women, who were in Hong Kong from 20 to 24 February this year. They were infected by a doctor from Guangzhou by a chance encounter in the lift lobby on the 9th floor of the MetropoleHotel in Mongkok in Hong Kong. In that chance encounter, the Chinese doctor was also to spread the disease to four other people besides the three Singaporeans. One was a local Hong Kong resident who visited a friend at the hotel, another was a 55-year-old Vancouver man, the third was a 78-year-old Toronto woman, and the fourth was a 48-year-old American businessman.The local Hongkonger became ill, and for a time was erroneously designated the index case in Hong Kong until the story of the real index case – the Guangzhou professor – surfaced. The rest returned home to become the index cases in Toronto and Vancouver, Hanoi, and Singapore. Singapore, as at 30 March 2003, had 91 cases and three deaths. The secondary cases were hospital doctors, nurses, and family members of the index cases.There are thankfully no cases out in the community, meaning those cases with no known source. This is a new viral infection and its infective capability is still being inferred from the cohort of infected cases in Singapore, Hong Kong and elsewhere. From the Singapore and Hong Kong experiences, the victims shed viruses when they are very ill. This will explain the secondary cases occurring among the healthcare providers in hospitals. Also, the virus is spread to those in close contact with the cases. It also appears that some cases are “Super Infectors”, meaning that these cases are more able to spread the infection to others around them. It is clear with present day travel that a bug can spread very rapidly across countries. As has occurred with the SARS Reflections on the outbreak, the spread to Hong Kong, Vietnam, Canada and Singapore came from one case coming across Guangzhou to Hong Kong. The WHO 36 report dated 29 March showed a tally of 37 cases with 470 cases and 10 deaths in Hong Kong, 58 cases and 4 deaths in Vietnam, 3 deaths in Canada, and 89 cases with 2 deaths in Singapore. An epidemiological network for early reporting remains the best way to limit the global spread. The doctors in Hanoi were fast to report its index case to WHO as a baffling case. This is a judgment call that requires clinical acumen to spot the index case to be unusual. Not always easy, but nevertheless, an important skill. The doctor who did that in Hanoi was Carlo Urbani. “Because of his early detection of SARS, global surveillance was heightened and many new cases have been identified and isolated before they infected hospital staff,” said the Genevabased UN health agency in a statement. Unfortunately, this doctor succumbed to SARS. He was infected in the process of caring for the index case in Hanoi, and eventually died in Bangkok on 29 March, where he had gone for a meeting. The present outbreak in Singapore and in the region, demonstrates the importance of a global and national network of epidemiological collection, investigation, processing, and disseminating points.The WHO, the CDCs and laboratories are crucial in providing the information and in advising communities what need to be done. Obviously, the close cooperation between WHO, countries, centres, and scientists remain paramount. The adequate funding of such a network both locally and globally is good investment for mankind. The cooperation of the community in control measures, like the closing of schools and other activities likely to allow transmission, is crucial. And it is a fine judgment between being too restrictive and too liberal. Until more is known about the ability of the disease to spread, it is safer to take more steps that may turn out to be not necessary later.Having adequate operating information for the public and medical practitioners will help to restore calm and behaviour that will be productive in bringing the infection under control. Each emerging infection that tests the defence network of the human race also reminds us of the great vulnerability of the human race. The possibility of a virulent superbug beyond the grip of medical science and technology is there. All this underscores the importance of the study and practice of communicable disease control, including drastic quarantine measures. It is important not to be lulled into complacency because infectious diseases have receded into the background 37 from the top causes of death of many countries. Each of us is a stakeholder, and if each of us remembers that, the battle is more likely to be won with the least number of victims. The SARS outbreak is a timely reminder of the importance of being prepared against communicable diseases, and where the control of a mysterious bug requires the stakeholder mentality that we are all vulnerable. There is also the confidence that together, we can erect a strong defence against the onslaught of the invisible invader. 8.0 CONCLUSION Though scientists and researchers have established the complete genetic code of the Corona virus, it will be a while before they come up with a suitable treatment option . Currently, the supportive care given to the patient is proving to be an important factor in patient recuperation. However, the combined efforts in the various biotech companies and other research institutes will hopefully shed light on this dreaded disease that has taken a toll on humanity.The SARS outbreak put a large number of patients in hospital, resulted in the death of many patients, disrupted the lives of countless people and damaged the economy.On the positive side, however it highlighted the importance of a cohesive professional and community response in resolving the crisis rapidly. Moving forward, the lessons learnt from SARS will result in countries having a much higher level of preparedness for infectious disease outbreaks. However, the model of close community participation and partnership in tackling public health problems. In this respect, we can learn much more from SARS than just control of infectious diseases. 38 9.0 REFERENCES 19/2/2011 http://www.sarsreference.com/sarsref/treat.htm http://www.clearleadinc.com/site/sars.html http://www.medindia.net/patients/patientinfo/SARS_conclusion.htm#ixzz1EPkhBY7a http://books.google.com.my/books?id=ZGIzRhGo_E0C&pg=PA163&lpg=PA163&dq=c onclusion+for+severe+acute+respiratory+system&source=bl&ots=XJuakX6MA3&sig=v fAZrqI4c3Djc0HdqcjMCZQogiM&hl=en&ei=3NBfTerxC8_HrQeXo_CEAg&sa=X&oi =book_result&ct=result&resnum=10&ved=0CGgQ6AEwCQ#v=onepage&q=conclusion %20for%20severe%20acute%20respiratory%20system&f=fa 17/2/2011 http://www.sarsreference.com/sarsref/epidem.htm http://www.epinorth.org/eway/default. 39 http://www.biomedcentral.com/1471-2334/10/50/prepub 18/2/2011 http://www.who.int http://www.diaspoir.net/health/sars/Malaysia.html. http://straitstimes. asia1.com.sg/columnist/0,1886,56-178860,00.html http://www.who.int/ csr/sarscountry/2003_03_29/en/ http://www.channelnewsasia.com/stories/southeastasia/view/36120/1/.html 21/2/2011 http://respiratory-lung.health-cares.net/sars-diagnosis.php http://www.wrongdiagnosis.com/s/sars/tests.htm http://health.nytimes.com/health/guides/disease/severe-acute-respiratory-syndromesars/overview.html 40