Practical classes
advertisement
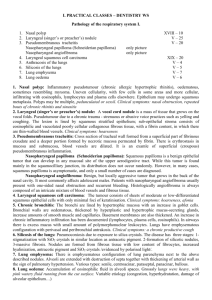
I. INTRODUCTION. PATHOLOGY OF THE RESPIRATORY SYSTEM I. 1. Nasal polyp: Inflammatory pseudotumour (chronic allergic hypertrophic rhinitis), oedematous, sometimes resembling myxoma. Uneven cellularity, with few cells in some areas and more cellular, infiltrating with eosinophils, lymphocytes and plasma cells elsewhere. Epithelium may undergo squamous metaplasia. Polyps may be multiple, pedunculated or sessil. Clinical symptoms: nasal obstruction, repeated bouts of chronic rhinitis and sinusitis 2. Laryngeal (singer’s or preacher’s) nodule: A vocal cord nodule is a mass of tissue that grows on the vocal folds. Pseudotumour due to a chronic trauma - strenuous or abusive voice practices such as yelling and coughing. The lesion is lined by squamous stratified epithelium; sub-epithelial stroma consists of eosinophilic and vacuolated poorly cellular collagenous fibrous tissue, with a fibrin content, in which there are thin-walled blood vessels. Clinical symptoms: hoarseness 3. Pseudomembranous tracheitis: Cross section of tracheal wall formed from a superficial part of fibrinous exsudate and a deeper portion formed by necrotic mucosa permeated by fibrin. There is erythrostasis in mucosa and submucosa, blood vessels are dilated. It is an examle of superficial (croupous) pseudomembranous inflammation. 4. Nasopharyngeal papilloma (Schneiderian papilloma): Squamous papilloma is a benign epithelial tumor that can develop in any mucosal site of the upper aerodigestive tract. While this tumor is found mainly in the squamocilliary junction, its distribution does not occur randomly. However, in many cases, squamous papilloma is asymptomatic, and only a small number of cases are diagnosed. 5. Nasopharyngeal angiofibroma: Benign, but locally aggressive tumor that grows in the back of the nasal cavity. It most commonly affects adolescent males. Patients with nasopharyngeal angiofibroma usually present with one-sided nasal obstruction and recurrent bleeding. Histologically angiofibroma is always composed of an intricate mixture of blood vessels and fibrous tissue. 6. Laryngeal squamous cell carcinoma: The tumour consists of sheets of moderate or low-differentiated squamous epithelial cells with only minimal foci of keratinisation. Clinical symptoms: hoarseness, afonia 7. Chronic bronchitis: The bronchi are lined by hypertrophic mucosa with an increase in goblet cells. Bronchial walls are oedematous, thickened by hyperplastic and hypertrophic mucus-secreting glands, increase amounts of smooth muscle and capillaries. Basement membranes are also thickened. An increase in chronic inflammatory infiltration has been documented (lymphocytes, plasma cells, eosinophils). In airways there is excess mucus with small amount of polymorphonuclear leukocytes. Lungs have emphysematous configuration with perivasal and peribronchial antrakosis. Clinical symptoms: a chronic productive cough 8. Silicosis of the lungs: Pneumoconiosis due to exposure to silica crystals. The disease has three stages: 1stigmatization with SiO2 crystals in similar location as antracotic pigment. 2-formation of silicotic nodules, 3-massive fibrosis. Nodules are formed from fibrous tissue with low content of fibrocytes, increased hyalinization, antracotic pigment and SiO2 crystals /evidenced by polarised light/. 9. Lung emphysema: There is emphysematous configuration of lung parenchyma next to the above described nodules. Alveoli are extended with destruction of septa together with thickening of arterial wall as the sign of pulmonary hypertension. Various types: senile, centroacinar, paraseptal, panacinar, bullous. 10. Lung oedema: Accumulation of eosinophilic fluid in alveoli spaces. Grosssly lungs were heavy, with pink watery fluid running from the cut surface. Variable etiology (congestion, hyperhydratation, damage of alveolar epithelium…) II. INTRODUCTION. PATHOLOGY OF THE RESPIRATORY SYSTEM II. 1. Chronic pulmonary congestion: Mostly in chronic insufficiency of the left ventricle and left atrium. Accumulation of macrophages with haemosiderin in the cytoplasm (blue in the Pearls reaction) due to reccurent alveolar haemorrhages and some interstitial fibrosis = brown induration. The lungs are heavy, congested and wet 2. Haemorrhagic infarction of the lungs: Occlusio of a lobar or segmental artery , especially in the presence of raised pulmonary venous pressure (left ventricular failure, mitral stenosis). Dark red pyramidal shape lesion, note a branch of pulmonary artery occluded by thrombembolus. 3. Bronchopneumonia : Acute catarrhal-suppurative superficial inflammation of the lungs, spreading from minor bronchi and bronchioles, aetiology variable. Alveoli are filled with polymorphonuclear leukocytes, little fibrin can be seen. The appearance of exudate may differ in various parts of the inflamed area. 4. Lobar pneumonia: Mostly infection with Streptococcus pneumoniae. Fibrinous-suppurative inflammation, involving major areas of lung parenchyma, spreading quickly through neighbouring alveoli. Alveoli are completely filled with a meshwork of fibrin fibers with leucocytes Several stages: inflammatory oedema, grey hepatisation (grossly resembles liver tissue), red hepatisation, and resolution. If not resorbed, the exudate can become organized (carnification). 5. Pulmonary carnification (caro = meat): Complication of healing of lobar pneumonia. Caused by incomplete resolution and organisation of the intraalveolar exudate with formation of non-specific granulation tissue (concentric arrangement of fibroblasts and collagen fibres in the alveoli). Irreversible filling of alveoli with connective tissue. 6. Nonsuppurative interstitial pneumocystis pneumonia: At autopsy non-specific finding. Microorganism Pneumocystis jiroveci (a yeast-like fungus) can be visualised in the spumoid masses in alveoli. Alveolar septa are thickened with mononuclear (plasmocytic and lymphocytic) infiltrate. Typical in immunocompromised patients. 7. Miliary tuberculosis: This lung tissue section shows multiple microscopic granulomas consisting of epithelioid and scattered multinucleated Langhans cells, surrounded by a thin layer of lymphocytes. Note accumulation of anthracotic pigment in the perivascular and peribronchial lymphatics. 8. Small cell cancer of the lungs: Second in frequency, this is the most malignant histological type. Oat cell, round cell type, with occasional neurosecretory granules on electron microscopy. Sometimes accompanied by paraneoplastic syndromes (Cushing’s syndrome, hypercalcemia, carcinoid syndrome). 9. Squamous cell carcinoma of the lungs: The most frequent histological form of bronchial carcinoma, especially in smokers (preceding squamous cell metaplasia and dysplasia of the bronchial epithelium). Various degree of differentiation with keratinisation and formation of keratin pearls in the differentiated forms. 10. Adenocarcinoma of the lungs: Tumour rises from bronchial epithelium or bronchial glands, but also without connection with bronchus. Large cell carcinoma: Non-differentiated variant of carcinoma, without morphology of squamous, small cell and adenocarcinoma. Poor prognosis.